Figure 1.
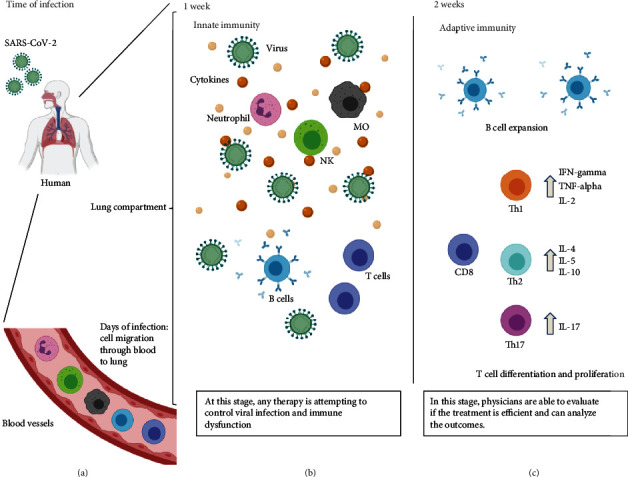
Immune response during COVID-19. (a) After SARS-CoV-2 contact with the respiratory tract of a human, susceptible cells are infected by entry through ACE2 or CD147 surface receptors. Once in the lung compartment, the first line of defense made of dendritic cells and other cells, such as macrophages, are able to recruit other immune cells. Then, cell migration through blood vessels are directed to the lung compartment, where cell activation occurs, initiating the inflammation process on the first week of signals and symptoms (b), inducing natural killer cell (NK), neutrophil, and macrophage (MO) activation in the lungs, causing the phenomenon called “cytokine storm.” In the mean time, B cells are producing antibodies, and immature T cells are also activated attempting to control the viral infection, although apoptotic events can also occur, reducing the number of T cells in the lungs and in the peripheral blood. After that, in two or more weeks (c), adaptive immune response is raised to specific IgG and neutralizing antibodies to contribute to the recovery and viral elimination. At this time, CD8 T cells are activated as cytotoxic phenotype, with the same aim, driving towards virus elimination. Meanwhile, the differentiation of CD4 T cells can trigger for more help for viral elimination by Th1 cells, but it can also lead to more lung damage by inflammatory phenotypes, such as Th2 and Th17 cells. Physicians and clinicians should evaluate each case to introduce the immunotherapies attempting to control the immune dysfunction. Created with BioRender.com.
