FIGURE 2.
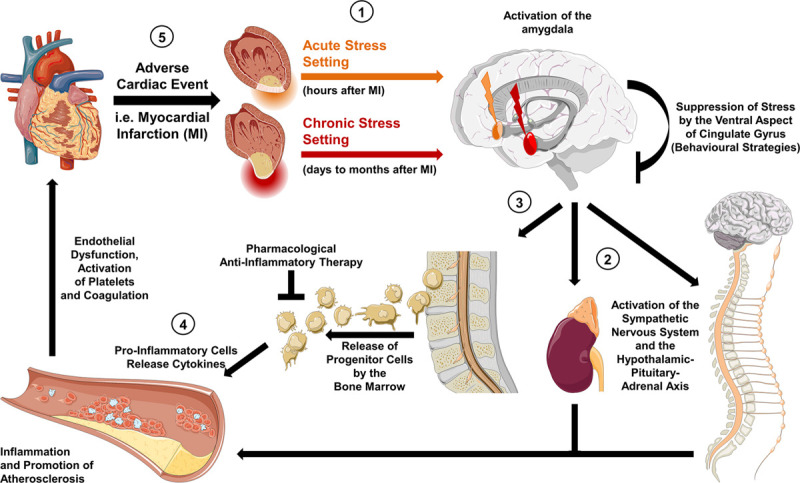
Hypothetic mechanisms of the neuro-inflammatory-vascular circuit. (1) Activity in the brain’s salient network is induced by acute stress (orange arrow) and chronic stress (red arrow), thereby triggering the activation of the amygdala. (2) Efferent projections to the brainstem upregulate sympathetic activity as well as the hypothalamic-pituitary-adrenal axis leading to an increase in circulating norepinephrine and cortisol. In an acute setting this results in an increased heart rate and blood pressure, which can be pharmacologically targeted by sympatholytic agents. In a chronic state, the tonic firing of the amygdala leads to modulation of central brain structures, such as the locus coeruleus, and to a chronic inflammatory state. (3) This is reflected by enhanced bone marrow activity and release of progenitor inflammatory cells. (4) Inflammatory cytokines (interleukin-6 and interleukin-18) promote endothelial dysfunction and progression of atherosclerosis. (5) The latter increases the risk of adverse cardiac events. Targeted anti-inflammatory treatment or behavioral strategies (e.g., stress reduction concepts) have the potential to diminish detrimental effects on the cardiovascular system.
