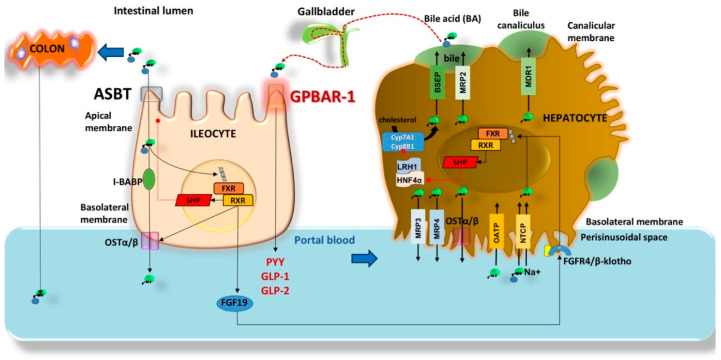
Figure 2.
Mechanisms governing bile acid (BA) enterohepatic circulation. In the liver BA undergo secretion into the perisinusoidal space by multidrug resistance proteins (MRP3, MRP4), and heterodimeric organic solute transporter (OSTα/β). Uptake is via organic anion transporting polypeptides (OATP) and Na+−taurocholate cotransporting polypeptide (NCTP). In the bile canaliculus, BA are secreted by bile acid export pump (BSEP) [21], MRP2, and multidrug resistance protein 1 (MDR1), and stored in the gallbladder upon neurohormonal-mediated contraction. In the terminal ileum, BA uptake occurs across the apical sodium dependent bile acid transporter (ASBT), the intracellular transport requires the intestinal BA binding protein (I-BABP); the secretion into the portal vein requires OSTα/β. BA signal the nuclear receptor Farnesoid X receptor (FXR) and retinoid X receptor (RXR) with effects on the small heterodimer partner (SHP), OSTα/β, and synthesis of the human enterokine fibroblast growth factor 19 (FGF19). BA also signal the ileal membrane receptor GPBAR-1 governing the secretion of peptide YY (PYY), glucagon-like peptide 1 (GLP-1) and glucagon-like peptide 2 (GLP-2) with metabolic effects (see text) [9,22]. Reabsorbed BA undergo peripheral spill over into the systemic circulation by about 10–50% [23]. About 15% of BA enter the colon for biotransformation into secondary BA and passive reabsorption. BA re-entering the liver can interact with GPBAR-1 in Kupffer cells and FXR-RXR-SHP (hepatocytes) [24] pathway which inhibits the activity of hepatocyte nuclear factor 4 (HNF4α) and liver-related homologue-1 (LRH1), resulting in inhibited expression of target genes governing BA synthesis (CYP7A1 and CYP8B1) and fatty acid synthesis. At low concentrations of BA, however, LRH-1 acts with LXR to trigger BA synthesis [25,26,27]. The circulating BA undergo renal uptake by the ASBT in the proximal tubules. MRP 2, 3, 4 transporters regulate glomerular filtration of BA [28]. The dashed red lines (-----●) indicate inhibition.