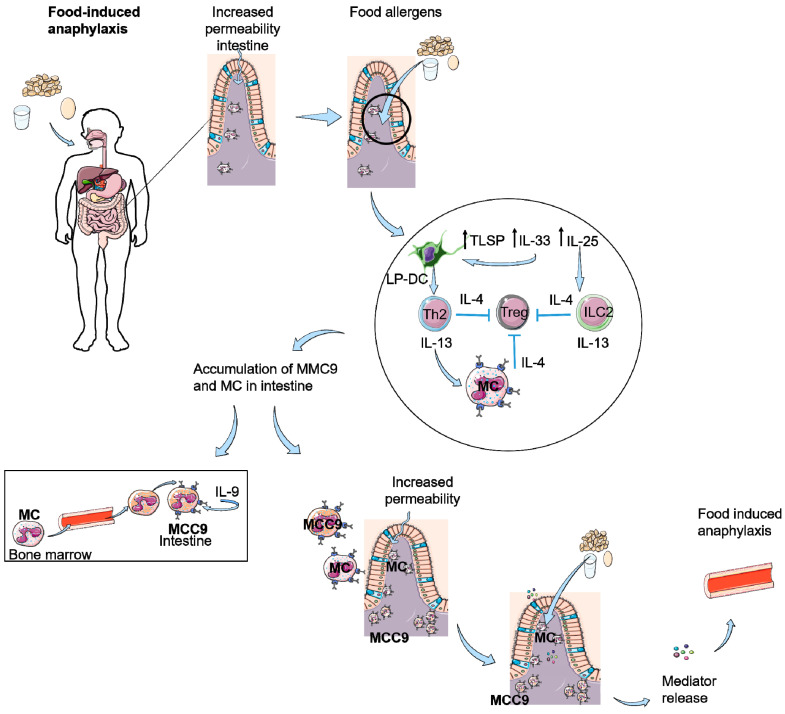
Figure 2.
Food-induced anaphylaxis as a result of scratching or decreased skin barrier function. Intestinal permeability is increased due to influx of mast cells (MC) as a result of scratching or damaged skin. This results an increased entrance of food antigens in the intestine eliciting the production of TSLP, IL-33, and IL-25. IL-25 can activate ILC2 cells and IL-33 and TSLP activate dendritic cells in the lamina propia of the intestine (LP-DC), which activate Th2 cells. Th2 cells and ILC2 cells produce IL-4 and IL-13, resulting in inhibition of Tregs and stimulation of MCs. This leads to an accumulation of (sensitized) MC and IL-9 producing mucosal mast cells (MMC9) in the intestine, which causes an increased permeability of the intestine. Food allergens can passage the epithelial barrier, resulting in IgE-mediated degranulation of the MCs and as a result of mediator release, food-induced anaphylaxis.