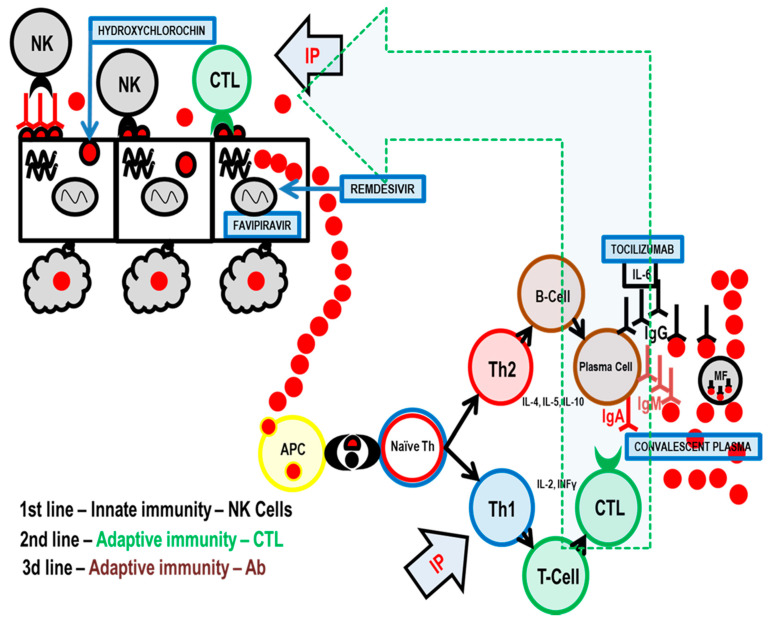
Figure 1.
Three levels of antiviral immunity and the influence of specific COVID-19 treatment options. Legend: red dot—virus SARS-CoV-2; IP—inosine pranobex; NK cells—natural killer cells; CTL—cytotoxic T-lymphocyte (CD8+); APC—antigen presenting cell; Naïve Th—naïve helper T lymphocyte (CD4+ cell); Th1—type of helper cells that lead to an increased cell-mediated immunity; Th2—type of helper cells that lead to a humoral immune (antibody) response; T-Cell—a type of lymphocyte, which differentiate into helper, regulatory, or cytotoxic T cells or become memory T cells; B-Cell—B cells are involved in humoral immunity and differentiate into a plasma cell; plasma cell—short-lived antibody-producing cell derived from B-Cell; IgA, IgM, IgG—antibody classes of immunoglobulins; MF—macrophages, specialized cells involved in the detection, phagocytosis and destruction of SARS-CoV-2 virus; convalescent plasma—high titers of neutralizing antibodies against SARS-CoV-2 to experimentally treat several critical COVID-19 patients; tocilizumab—a humanized monoclonal antibody against the interleukin-6 receptor (IL6); favipiravir—an antiviral medication used to treat influenza and experimentally also COVID-19; hydroxycholochin (hydroxychloroquine)—suggested early in the pandemic as prevention or treatment method for COVID-19; remdesivir—a nucleotide analog prodrug indicated for treatment of COVID-19 disease in hospitalized patients.