Abstract
Background
Malnutrition in patients hospitalized in internal medicine wards is highly prevalent and represents a prognostic factor of worse outcomes. Previous evidence suggested the prognostic role of the nutritional status in patients affected by the coronavirus disease 2019 (COVID-19). We aim to investigate the nutritional risk in patients with COVID-19 hospitalized in an internal medicine ward and their clinical outcomes using the Nutritional Risk Screening 2002 (NRS-2002) and parameters derived from bioelectrical impedance analysis (BIA).
Methods
Retrospective analysis of patients with COVID-19 aimed at exploring: 1) the prevalence of nutritional risk with NRS-2002 and BIA; 2) the relationship between NRS-2002, BIA parameters and selected outcomes: length of hospital stay (LOS); death and need of intensive care unit (ICU); prolonged LOS; and loss of appetite.
Results
Data of 90 patients were analyzed. Patients at nutritional risk were 92% with NRS-2002, with BIA-derived parameters: 88% by phase angle; 86% by body cell mass; 84% by fat-free mass and 84% by fat mass (p-value ≤0.001). In ROC analysis, NRS had the maximum sensitivity in predicting the risk of death and need of ICU and a prolonged hospitalization showing moderate-low specificity; phase angle showed a good predictive power in terms of AUC. NRS-2002 was significantly associated with LOS (β 12.62, SE 5.79). In a multivariate analysis, blood glucose level and the early warning score are independent predictors of death and need of ICU (OR 2.79, p ≤0.001; 1.59, p-0.029, respectively).
Conclusion
Present findings confirm the clinical utility of NRS-2002 to assess nutritional risk in patients with COVID-19 at hospital admission and in predicting LOS, and that bioimpedance does not seem to add further predictive value. An early detection of nutritional risk has to be systematically included in the management of COVID-19 patients hospitalized in internal medicine wards.
Keywords: COVID-19, malnutrition, bioelectrical impedance, nutritional risk score, risk of death, risk of ICU admission, length of hospital stay
Background
In hospitalized patients, malnutrition exhibits a high prevalence, reaching rates up to 50% in the internal medicine wards, and representing a public health issue.1 Nutritional status was found to be associated with the novel Coronavirus disease 2019 (COVID-19) severity, and malnutrition might play a role in this regard, but this aspect was investigated in a limited number of studies.2–4 Previous studies have shown that malnutrition represents an independent risk factor for the prognosis of various infectious diseases including pneumonia.5
Nutritional risk screening tools are useful in the everyday clinical practice to promptly detect potential or evident malnutrition. Identification of patients at nutritional risk allows physicians to perform a nutritional assessment providing the basis to determine the presence of a malnutrition according to the nutrition diagnostic procedure.6 Nutritional risk can be assessed by different tools and the Nutritional Risk Screening 2002 (NRS-2002) is indicated for hospitalized patients.7
The NRS-2002 takes into account the patient’s comorbidities and the clinical severity at admission. The validity of this screening tool for the assessment of nutritional status has been validated previously in several studies in hospitalized patients with multiple diseases,8 but its role in patients with COVID 19 has not been exhaustively elucidated.
The issue becomes even more interesting considering that COVID-19, has the potential to predispose patients to a higher nutritional risk (due to decreased appetite and weight loss as frequent clinical manifestations during the infection) and that the NRS tool utility in specific diseases, such as COVID-19, was investigated in few studies.
A previous study conducted in a Chinese cohort of 140 elderly patients (over 65 years) hospitalized for COVID-19 and later a systematic review, analyzed the usefulness of the different NRS scales, including the NRS-2002, confirming their usefulness in screening patients needing additional nutritional interventions.4,9
Currently, several studies are striving to define the risk factors for the development of severe pneumonia in COVID-19 patients and to identify the factors that can have an impact on patient outcome.10,11 To date, there are also no studies that have evaluated the nutritional status of patients affected by COVID-19 with bioelectrical impedance analysis (BIA). Given the prognostic value of bioimpedance parameters on different clinical outcomes already demonstrated for other categories of patients,11,12 it can be assumed that this could also provide useful information in the management of COVID-19 patients.
In the present study, we retrospectively aim to investigate the nutritional status of a sample of patients with COVID-19 hospitalized in an internal medicine ward, using the NRS-2002 tool and parameters derived by bioimpedance analysis. We also aim to explore the accuracy of the NRS-2002 and BIA parameters and their relationship in predicting: 1) the length of hospital stay (LOS), 2) the occurrence of in-hospital mortality and need of hospitalization in intensive care unit (ICU), 3) a prolonged length of hospital stay and 4) a loss of appetite.
Methods
Study Design and Participants
Retrospective observational study of patients consecutively admitted at the Department of Internal Medicine of the La Carità hospital of Locarno (Ente Ospedaliero Cantonale, Switzerland) in March 2020. All patients hospitalized with a diagnosis of COVID-19 were enrolled in the study.
The diagnosis of COVID-19 was based on 1) positive results of polymerase chain reaction assay performed on the upper or lower respiratory tract, 2) clinical criteria (positive anamnesis for an epidemiological history of exposure; fever (temperature > 37.3 °C), cough, gastrointestinal symptoms), 3) laboratory criteria (total number of white blood cells, lymphocyte count) and iv) radiological pulmonary imaging. The study was approved by the Swiss Ethics Commission and adhered to the principles of the Declaration of Helsinki. Only data of patients who gave written informed consent were analyzed.
Data Collection and Definitions
Anthropometric, clinical, and laboratory testing were recorded within the first 24-h after admission. Parameters collection included height, weight, body mass index (BMI), Early Warning Score (EWS), age, gender, clinical diagnosis, day of hospital admission and laboratory parameters. All measurements were performed using a standardized protocol and calibrated equipment. Nutritional risk screening was performed using the NRS-2002 within the first 24 hours of admission. Patients were reclassified as “at nutritional risk” with a score of ≥3, whereas a score <3 indicated “no nutritional risk”.12
BIA was performed using a portable device (BIA 101, Akern Bioresearch, Florence, Italy). All procedures were carried out by experienced dieticians. All R and Xc assessments were produced following a standardized procedure as indicated by the manufacturer: patient supine on a bed, legs apart, and arms not touching the torso. Original electrodes (BIATRODES Akern Srl; Florence, Italy) were used and placed in predetermined locations following the manufacturer's instructions after cleansing the skin with alcohol. All measurements were performed with the same device striving to guarantee reproducibility.
The procedure was not performed in case of fever or diaphoresis. It is important to note that the internal management protocol for COVID-19 patients at the moment of the study inclusion recommended to avoid fever using if necessary a multi-drug approach (eg, paracetamol, metamizole, NSAID, and corticosteroid infusions).
Impedance values of resistance (R) and reactance (Xc) were measured in stable conditions, and phase angle (PhA), fat-free mass (FFM), fat mass (FM) and body cell mass (BCM) were obtained as suggested by the manufacturer using the BodyGram™ (Version 1.31, Akern Bioresearch, Pontassieve FL, Italy), a software validated in different clinical settings.13–17
The participants were considered as malnourished when BIA parameters were lower than the 15th percentile, corresponding to the following values: PhA 4.3°, FFM kg/m 27.9, FM Kg/m 6.2, BCM 13.7 kg/m.
The performance of NRS and BIA parameters in predicting a composite outcome of death and admission in an intensive care unit (ICU), a prolonged hospitalization and a loss of appetite was investigated. Mortality and ICU admission were defined as in-hospital death or unplanned intensive care unit transfer during the index admission. The relationship between NRS-2002, BIA-derived parameters and LOS was also explored. LOS, expressed in days, was calculated from admission to discharge and a prolonged hospital stay was defined as a LOS ≥21 days. Data of NRS-2002 and BIA parameters were collected following standardized procedures in the COVID-19 ward. NRS and BIA were performed as default assessments. The hospital dietician team, and a clinical nutrition physician consultant, performed first a nutritional risk screening with NRS-2002 and then a BIA. All procedures were performed ensuring the safety of patients and healthcare professionals.
Statistical Analysis
Continuous variables were shown as the mean ± SD and categorical data as percentages. X2 and t-test, as appropriate were used to examine the differences between the nutritional status assessed by NRS and BIA parameters.
The performance of NRS and BIA parameters in predicting the occurrence of clinical outcomes was assessed using Receiver Operating Characteristic (ROC) curves. The association between NRS-2002, BIA-derived parameters and length of hospital stay were explored using linear regression models. Β-coefficient and Standard Error (SE) were shown. The relationship between nutritional NRS-2002, BIA parameters and clinical outcomes (death and need of ICU, prolonged hospitalization, loss of appetite) was analyzed by logistic regression analysis. Crude (Model 1) and adjusted models (Model 2) were shown. Model 2 was adjusted for selected covariates to examine potential confounding effects. Age, gender, body mass index, Early Warning Score, diabetes, hypertension, history of cardiovascular disease, hemoglobin, c-reactive protein, fasting glucose and total body water were included in the multivariate model as covariates. Odds Ratio (OR) and confidence intervals were shown. Data analysis was performed using R statistical software (www.r-project.org) and SPSS (version 18.0, Chicago, IL, USA). Statistical significance for all outcomes was set at p ≤ 0.05.
Results
Data of 90 patients with COVID-19 were analyzed. There were 61 males and 29 females, and the average age was 64.5 ± 13.7 years. One-third of patients were affected by cardiovascular diseases or hypertension (30 and 35%, respectively) and 10% by diabetes.
Markers of body composition showed the following results: PhA, 5.6 ± 1.14°; TBW 25.5 ± 4.2 L/m; Fat-free mass index 34.3 ± 6.0 kg/m; Fat mass 12.4 ± 5.4 kg/m; BCM, 17.8 ± 4.7 Kg/m.
In-hospital deaths and ICU need were 18 (20%). Mean LOS was 16.4 ± 14.9 days, 19 (21.0%) patients had a prolonged hospitalization, whilst 28 patients (31.0%) had a loss of appetite during hospitalization (Table 1).
Table 1.
Baseline Characteristics of 90 Patients Admitted to an Internal Medicine Ward for COVID-19
| Characteristics | Total |
|---|---|
| Age, years | 64.5 ± 13.7 |
| Gender, females | 29 (32.2) |
| Body mass index, kg/m2 | 27.1 ± 4.0 |
| SBP, mmHg | 133.1 ± 20.3 |
| DBP, mmHg | 79.0 ±10.9 |
| Heart rate, beats/sec | 86.3±15.61 |
| Breathing rate | 21.8 ± 5.6 |
| Hemoglobin, g/L | 141.7 ± 16.9 |
| Fasting glucose, mmol/l | 7.3 ± 2. 5 |
| ESW | 5.5 ± 2.9 |
| Creatinine, µmol/L | 103.9 ± 111.9 |
| Sodium, mmol/L | 136.6 ± 3.5 |
| Potassium, mmol/L | 3.8 ± 0.44 |
| Calcium, mmol/L | 2.19 ± 0.11 |
| C-reactive protein, mg/L | 89.0 ± 71.5 |
| CVD, % | 27 (30.0) |
| Diabetes mellitus, % | 9 (10.0) |
| Hypertension, % | 32 (35.6) |
| PhA, ° | 5.6 ± 1.14 |
| TBW, L/m | 25.5 ± 4.2 |
| Fat-free mass, kg | 58.2 ± 10.7 |
| Fat-free mass index, kg/m | 34.3 ± 6.0 |
| Fat mass, kg | 21.1± 9.1 |
| Fat mass, kg/m | 12.4 ± 5.4 |
| BCM, kg/m | 17.8±4.7 |
| NRS-2002 | 4.4 ± 1.27 |
| Length of hospital stay, days | 16.4 ± 14.9 |
| Prolonged hospitalization, n % | 19(21) |
| In-hospital deaths or ICU needing, n (%) | 18(20) |
| Loss of appetite, (n %) | 28 (31%) |
Abbreviations: SBP, systolic blood pressure; DBP, diastolic blood pressure; ESW, early warning score; CVD, cardiovascular diseases; PhA, phase angle; TBW, total body water; BCM, body cell mass; ICU, intensive care unit; NRS, nutritional risk screening.
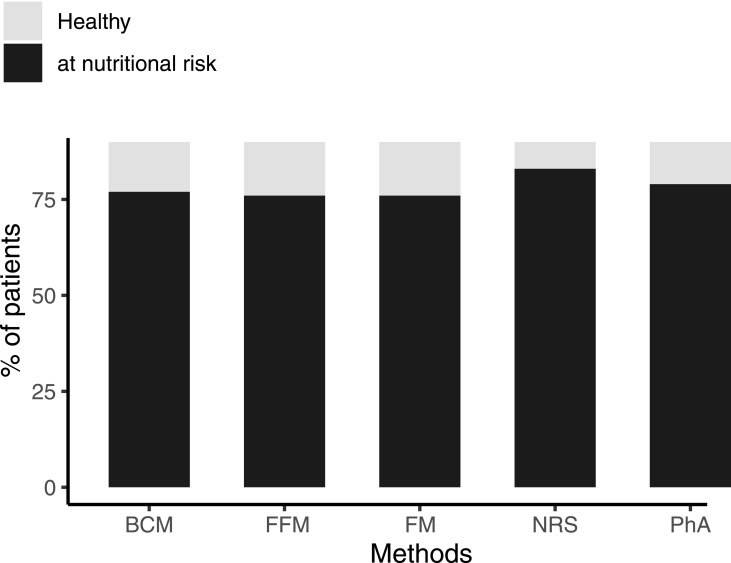
Based on NRS-2002 and BIA parameters, patients were classified as normal or at nutritional risk with the following percentages: 7 (7.8%) and 83 (92.2%) with NRS-2002, 11 (12.0%) and 79 (88%) with phase angle; 14 (15.6%) and 76 (84.4%) with fat-free mass; 14 (15.6%) and 76 (84.4%) with fat mass and 13 (14.5%) and 77 (85.5%) with BCM (Figure 1). The percentage of the group found to be at risk varied significantly between NRS-2002, PhA, FFM, FM and BCM (p < 0.001) (Figure 1).
Figure 1.
Risk groups’ comparison between NRS-2002 and BIA parameters. The percentage of the group found to be at risk varied significantly between NRS-2002, PhA, FFM, FM and BCM (p < 0.001).
Differences in parameters of body composition by outcomes under investigation are presented in Table 2. No differences were detected among groups.
Table 2.
Body Composition and Nutritional Risk Screening According to Outcomes Under Study
| Characteristics | Combined Outcomes | p-value | Prolonged Hospitalization | p-value | Loss of Appetite | p-value | |||
|---|---|---|---|---|---|---|---|---|---|
| PhA,° | 5.7 ± 4 1.1 | 5.4 ± 1.3 | 0.386 | 5.7 ± 1.1 | 5.2 ± 1.3 | 0.1094 | 5.5± 1.1 | 5.8 ± 1.1 | 0.286 |
| R, Ω | 495.9 ± 87.2 | 484.7 ± 111.2 | 0.648 | 490.7 ± 90.5 | 504.6 ± 98.9 | 0.562 | 499.2 ± 101.7 | 481.4 ± 65.1 | 0.398 |
| XC, Ω | 48.5 ± 9.8 | 44.8 ± 11.3 | 0.175 | 48.4 ± 10.1 | 45.3 ± 10.1 | 0.243 | 47.4 ± 10.6 | 48.5 ± 9.2 | 0.654 |
| TBW (%) | 54.8 ± 7.0 | 55.3 ± 7.4 | 0.787 | 55.1 ± 7.3 | 54.1 ± 6.2 | 0.578 | 55.4 ± 7.29 | 53.8 ± 6.8 | 0.320 |
| ECW (%) | 47.5 ± 6.6 | 49.6 ± 7.1 | 0.254 | 47.3 ± 6.5 | 50.5 ± 7.4 | 0.066 | 48.3 ± 7.3 | 47.2 ± 5.3 | 0.508 |
| Hydration (TBW/FFM), % | 74.3 ± 2.7 | 75.2 ± 3.2 | 0.204 | 74.3 ± 2.3 | 75.2 ± 4.2 | 0.226 | 74.6 ± 3.0 | 74.2 ± 2.1 | 0.546 |
| Fat-free mass, kg/m | 12.4 ± 5.3 | 12.5 ± 5.93 | 0.921 | 12.2 ± 5.5 | 13.1 ± 4.9 | 0.520 | 11.9 ± 5.2 | 13.4 ± 5.9 | 0.233 |
| Fat-free mass index, kg/m | 33.9 ± 4.9 | 35.8 ± 9.4 | 0.253 | 34.1 ± 5.2 | 34.8 ± 8.6 | 0.658 | 34.3 ± 6.8 | 34.1 ± 4.2 | 0.888 |
| BCM, Kg | 17.6 ± 3.9 | 18.9 ± 6.9 | 0.297 | 18.2 ±4.8 | 16.4 ± 4.4 | 0.143 | 17.8 ± 5.2 | 17.9 ± 3.5 | 0.920 |
| NRS-2002 | 4.3± 1.3 | 4.9 ± 0.8 | 0.095 | 4.4 ± 1.4 | 4.7 ± 0.9 | 0.352 | 4.1 ± 3.8 | 5.2 ± 0.8 | <0.001 |
Abbreviations: PhA, phase angle; ECW, extracellular water; TBW, total body water; NRS-2002, Nutritional Risk Screening 2002; BCM, body cell mass.
The results of ROC curve analyses showed that NRS and PhA were more effective in predicting the occurrence of worse clinical outcomes, whereas other BIA-derived parameters were less effective (Table 3).
Table 3.
ROC Curves in Predicting Clinical Outcomes, Prolonged Hospitalization and Loss of Appetite According to NRS and Bioimpedance Parameters
| Composite Outcome | Prolonged Hospitalization | Loss of Appetite | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivity | Specificity | AUC (95% CI) | p-value | Sensitivity | Specificity | AUC (95% CI) |
p-value | Sensitivity | Specificity | AUC (95% CI) | p-value | |
| NRS-2002 | 100 | 0.217 | 0.549 (0.514–0.583) | 0.911 | 100 | 0.229 | 0.549 (0.514–0.584) | 0.991 | 100 | 0.337 | 0.556 (0.517–0.596) | 0.991 |
| PhA | 0.835 | 0.454 | 0.597 (0.486–0.708) | 0.033 | 0.823 | 0.455 | 0.589 (0.483–0.696) | 0.045 | 0.909 | 0.342 | 0.563 (0.505–0.621) | 0.125 |
| FM | 0.802 | 0.214 | 0.507 (0.409–0.605) | 0.884 | 0.857 | 0.224 | 0.532 (0.448–0.615) | 0.500 | 0.714 | 0.316 | 0.509 (0.429–0.590) | 0.823 |
| FFM | 0.803 | 0.214 | 0.507 (0.409–0.605) | 0.884 | 0.857 | 0.224 | 0.532 (0.448–0.615) | 0.500 | 0.786 | 0.329 | 0.535 (0.460–0.611) | 0.399 |
| BCM | 0.846 | 0.208 | 0.521 (0.435–0.607) | 0.654 | 0.818 | 0.385 | 0.575 (0.467–0.683) | 0.107 | 0.923 | 0.351 | 0.579 (0.518–0.640) | 0.08 |
Abbreviations: ROC, receiver operating characteristics; AUC; area under the curve; NRS-2002, Nutritional Risk Screening 2002; PhA, phase angle; FM, fat mass; FFM, fat-free mass; BCM, body cell mass.
In particular, NRS-2002 has a 100% sensitivity for the composite outcome, prolonged hospitalization and loss of appetite, but a low specificity (22%, 23% and 34% respectively). PhA showed an AUC for the composite outcome of 0.597 (CI 95%, 0.486–0.708) and for the prolonged hospitalization of 0.589 (CI 95%, 0.483–0.696) and a sensitivity of 82 and a specificity of 45%.
The relationship between NRS-2002, BIA-derived parameters and length of hospitalization was explored in a linear regression analysis (Table 4). In both adjusted and unadjusted models NRS-2002 was found to be significantly associated with LOS (β 12.62, SE 5.79, p-value 0.030; β 12.82, SE 5.96, p-value 0.030). No significant associations were found between BIA-derived parameters and LOS. A multivariate regression analysis of the NRS and bioimpedance parameters for clinical outcomes in Patients with COVID-19 showed that independent predictors of death/necessity of ICU were blood glucose level and EWS; OR 2.80 (CI 95% 1.41–5.53, p-value ≤0.001) and 1.59 (CI 95% 1.06–2.39, p-value 0.026) respectively. A strong association was found between NRS-2002 and the risk of loss of appetite in both unadjusted and adjusted models; OR 3.07 (CI 95% 1.65–6.68, p-value ≤0.001) and 7.33 (CI 95% 2.62–20.47, p-value ≤0.001) respectively (Table 5).
Table 4.
Linear Regression Exploring the Correlation Between NRS-2002, Bioimpedance Parameters and Length of Hospitalization
| Model 1-Unadjusted | |||
|---|---|---|---|
| Beta Coefficient | Standard Error | p-value | |
| NRS-2002 ≥3 | 12.62 | 5.79 | 0.030* |
| PhA ≤15th percentile | 8.39 | 4.79 | 0.083 |
| FM ≤15th percentile | −2.66 | 4.35 | 0.558 |
| FFM ≤15th percentile | −5.37 | 4.37 | 0.222 |
| BCM ≤15th percentile | 2.57 | 4.54 | 0.573 |
| Model 2-Adjusted | |||
| NRS-2002 ≥3 | 12.82 | 5.96 | 0.038* |
| PhA ≤15th percentile | 4.77 | 4.92 | 0.335 |
| FM ≤15th percentile | −4.87 | 4.81 | 0.313 |
| FFM ≤15th percentile | −7.87 | 5.72 | 0.173 |
| BCM ≤15th percentile | 0.93 | 4.69 | 0.843 |
Notes: Model 2 is adjusted for age, sex, BMI, hypertension, diabetes, cardiovascular diseases, early warning score, serum glucose; *p-value <0.05.
Abbreviations: NRS-2002, Nutritional Risk Screening 2002; PhA, phase angle; FM, fat mass; FFM, fat-free mass; BCM, body cell mass.
Table 5.
Multivariate Regression Analysis of NRS and Bioimpedance Parameters for Clinical Outcomes in Patients with COVID-19
| Model 1-Unadjusted | ||||||
|---|---|---|---|---|---|---|
| Combined Outcomes | Prolonged Hospitalization | Loss of Appetite | ||||
| OR (95% CI) | p value | OR (95% CI) | p value | OR (95% CI) | p value | |
| NRS | 1.54 (0.90.2.65) | 0.110 | 1.24 (0.78–1.96) | 0.362 | 3.07 (1.65–5.68) | ≤0.001* |
| PhA | 0.50(0.24–1.06) | 0.071 | 1.48 (0.15–14.62) | 0.735 | 2.08 (0.95–4.53) | 0.066 |
| FM | 0.96(0.86–1.07) | 0.471 | 0.99 (0.89–1.11) | 0.990 | 1.12 (0.99–1.25) | 0.051 |
| FFM | 1.06 (0.96–1.18) | 0.243 | 1.20 (0.68–2.12) | 0.532 | 0.96 (0.85–1.09) | 0.513 |
| BCM | 1.14 (0.96–1.37) | 0.124 | 0.69 (0.22–2.16) | 0.524 | 0.89 (0.71–1.13) | 0.364 |
| Model 2-Adjusted | ||||||
| NRS | 1.68 (0.59–4.72) | 0.326 | 1.13 (0.62–2.06) | 0.702 | 7.33 (2.62–20.47) | ≤0.001* |
| PhA | 0.59 (0.21–1.71) | 0.332 | 1.04 (0.12–8.63) | 0.974 | 2.53 (0.38–16.74) | 0.334 |
| FM | 0.65 (0.44–0.97) | 0.036 | 1.13 (0.86–1.48) | 0.396 | 0.93 (0.72–1.21) | 0.613 |
| FFM | 0.84 (0.68–1.05) | 0.152 | 1.17 (0.60–2.25) | 0.650 | 0.94 (0.65–1.35) | 0.742 |
| BCM | 1.28 (0.96–1.72) | 0.093 | 0.95 (0.32–2.84) | 0.932 | 0.71 (0.29–1.68) | 0.435 |
| Gender, females | 1.23 (0.08–19.53) | 0.881 | 4.32 (0.25–76.0) | 0.317 | 0.54 (0.04–6.43) | 0.622 |
| Age | 0.96 (0.88–1.06) | 0.484 | 1.00 (0.94–1.08) | 0.930 | 0.92 (0.86–0.99) | 0.027* |
| ESW | 1.59 (1.06–2.39) | 0.026* | 1.09 (0.85–1.39) | 0.498 | 1.07 (0.83–1.39) | 0.602 |
| Glucose | 2.80 (1.41–5.53) | ≤0.001* | 1.73 (1.06–2.83) | 0.028* | 0.99 (0.69–1.42) | 0.947 |
| CRP | 1.00 (0.99.1.01) | 0.609 | 0.99 (0.99–1.00) | 0.610 | 0.99 (0.99–1.00) | 0.483 |
| Hemoglobin | 0.95 (0.88–1.03) | 0.185 | 1.04 (0.98–1.10) | 0.259 | 0.97 (0.92–1.02) | 0.236 |
| BMI | 1.53 (0.95–2.45) | 0.080 | 0.79 (0.52–1.18) | 0.243 | 1.26 (0.86–1.85) | 0.231 |
| Hypertension | 0.58 (0.09–3.64) | 0.564 | 1.22 (0.31–4.83) | 0.773 | 0.28 (0.07–1.24) | 0.094 |
| CVD | 2.94 (0.39–21.8) | 0.292 | 1.44 (0.33–6.42) | 0.626 | 1.08 (0.24–4.93) | 0.914 |
| Diabetes | 0.35 (0.02–6.58) | 0.484 | 2.18 (0.22–21.54) | 0.504 | 1.26 (0.08–18.92) | 0.865 |
Note: *p-value<0.05.
Abbreviations: NRS, nutritional risk score; PhA, phase angle; FM, fat mass; FFM, fat-free mass; BCM, body cell mass; EWS, early warning score; CRP, c-reactive protein; BMI, body mass index, CVD, cardiovascular diseases; TBW, total body water.
Discussion
Results of the present study show that a high proportion of patients with COVID-19 are at nutritional risk (92%) and that NRS-2002 has an excellent sensitivity in identifying patients with poor clinical outcomes. Moreover, NRS-2002 is significantly associated with length of hospitalization and with an increased risk of loss of appetite even after controlling for several confounding factors. Among BIA-parameters PhA revealed the best predictive power for all explored outcomes.
Present results confirm the high prevalence of nutritional risk in COVID-19 patients, recently highlighted in two cross-sectional studies. The first one, conducted in Italy has recently shown a prevalence of 77% of patients at nutritional risk as assessed by NRS-2002.18 We can speculate that the higher prevalence of patients at nutritional risk here identified could be related on one hand to the older age of our population and on the other, to the fact that modified criteria of the NRS-2002 were used in the Italian study. The second one, conducted in Wuhan in patients older than 65 years, showed however a proportion of patients at nutritional risk very similar to that found here.
In hospitalized patients with infections and especially in the elderly, the early nutritional risk identification still represents a challenge; even more so considering that malnutrition could be a risk factor as well as a consequence of infections themselves.19,20 Nevertheless, to date, most previous studies have been focused on exploring the relationship between obesity and clinical outcomes in COVID-19 patients and only a limited number of investigations have been focused on other nutritional parameters.3,21
Here we strive to define the prevalence of nutritional risk in hospitalized patients with COVID-19, aiming to assess the utility of NRS-2002 and of bioimpedance analysis in this class of patients.
In an unselected internal medicine population we found that the 2002 nutritional screening is helpful in identifying patients with COVID-19 at nutritional risk and is predictive of worse outcome and prolonged LOS.
The association between malnutrition and LOS was well investigated in other clinical conditions and settings.22,23 The present results confirm that also in COVID-19 the nutritional risk based on the NRS-2002 independently predicts LOS.
Considering the relationship between LOS and patients’ clinical outcomes,24–26 an early identification of potential risk factors for LOS, is a fundamental step for better patient management, especially in those at high-risk such as COVID-19 patients.
Considering that hospitalized COVID-19 patients often show clinical manifestations such as fever, loss of appetite and/or weight up to anorexia, the risk of a further decline of the nutritional status appears high.27,28
Hence, the identification of nutritional risk in this class of patients can favour the adoption of measures to prevent worsening of nutritional status during hospitalization.
Even if beyond the scope of this study it is also conceivable that early nutritional support of these patients could result in an improvement of clinical outcomes. Larger studies are advocated in order to establish the magnitude of the impact of malnutrition on disease-related mortality in this class of patients.
In this study, multivariate regression analysis revealed that prolonged LOS and poorer appetite were significantly associated with the NRS-2002 assessed nutritional risk. Early interventions for patients with COVID-19 at nutritional risk are recommended.
Moreover, here we found that 34 patients with normal BMI (18.5 < BMI < 25) were classified as having nutritional risk according to NRS-2002. This aspect is in line with findings of previous studies indicating a scarce agreement between anthropometric measures and NRS,25 suggesting the importance of the nutritional assessment not only based on height and weight but also including the NRS-2002 screening of all patients with COVID-19 admitted to a hospital.
In our study, we confirmed that EWS is significantly associated with the risk of mortality and ICU admission in COVID-19 patients. The Early Warning Score is widely used to quantify patients’ deterioration.29 The rapid and early recognition of patients requiring ICU admission represents a challenge in the clinical management of patients with COVID-19. Our data are in line with findings of previous studies suggesting the use of this tool by clinicians to promote the early identification of COVID-19 patients with a serious disease and at high risk of ICU admission.30,31
Results of our study emphasize another important aspect in the COVID-19 disease: the strong relationship between glucose level at admission and worst prognosis. It is well noted that hyperglycemia at admission in the hospital could negatively impact patients’ prognosis and that the rapid recognition and correction would considerably improve hospitalized patients’ outcomes.32 The present results are in line with previous findings in which the role of hyperglycemia on COVID-19 patients’ prognosis was highlighted.33,34
We have to acknowledge several limitations in the present study. Firstly, the number of patients included in the analysis was small. Secondly, it was a single-center study. Thirdly, all the intrinsic limitations of its retrospective design were unavoidable. Moreover, we did not perform a randomised comparison, and therefore we cannot exclude possible unmeasured confounding. Last but not least, in our study, we did not collect in a systematic way data on the nutritional support offered to our patients. We are aware that this information could have been useful from a clinical perspective for the management of COVID-19 patients. Regrettably, due to the lack of information available on the disease, when the pandemic started, we did not plan to collect these data. Overall, regarding the nutritional support offered, we can affirm that most patients in our cohort showed lack of appetite, often associated with dysosmia and dysgeusia. The hospital diet was standardized as a soft diet regime, which was individualized based on patient’s clinical conditions. Patients transferred to the intensive care unit started enteral nutrition based on the estimated needs (scarcely reached due to the high prevalence of diarrhoea). A nutritional physician operating in the COVID-19 ward prescribed all nutritional therapies. Further studies should be performed to investigate the relationship between specific nutritional supports in hospitalized COVID-19 patients identified by the NRS tools and clinical outcomes.
Despite its limitations, this study has the strength of being the first research aimed at exploring the nutritional status in patients hospitalized with COVID-19, with screening and bioimpedance tools, highlighting once again the importance of in-hospital nutritional screening for these patients.
Conclusions
The present study confirms that the NRS-2002 is a useful and practical tool to assess nutritional risk, to predict clinical outcomes and to implement rapid additional nutritional interventions in patients with COVID-19. It also shows that bioimpedance does not seem to add further predictive value. Our findings further point out the importance of a rapid nutritional screening upon admission in patients hospitalized with COVID-19 and suggest that further research in this area, to identify early nutritional needs, could be useful in improving disease outcomes. The early diagnosis and treatment of malnutrition should be systematically included in the management of COVID-19 patients hospitalized in an internal medicine ward.
Acknowledgments
No funding or sponsorship was received for this study or publication of this article. All named authors meet the International Committee of Medical Journal Editors’ (ICMJE) criteria for authorship, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Funding Statement
No funding or sponsorship was received for this study or its publication. This research received no specific grant from any public funding agency, commercial or not-for-profit sectors.
Abbreviations
COVID-19, coronavirus disease 2019; NRS, nutritional risk screening; ICU, intensive care unit; BIA, bioelectrical impedance analysis; EWS, early warning score; PhA, phase angle; BCM, body cell mass; FFM, fat-free mass; FM, fat mass; LOS, length of hospital stay.
Data Sharing Statement
The dataset analyzed during the current study is available from the corresponding author upon reasonable request.
Compliance with Ethics Guidelines
The study was conducted in accordance with the Declaration of Helsinki. The study was approved by the Swiss Ethics Commission (2020-01697, CE3697). All patients gave written informed consent.
Consent for Publication
All authors have provided consent to publish.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest.
References
- 1.Hiesmayr M, Tarantino S, Moick S, et al. Hospital malnutrition, a call for political action: a public health and nutritionday perspective. J Clin Med. 2019;8(12):pii: E2048. doi: 10.3390/jcm8122048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gualtieri P, Falcone C, Romano L, et al. Body composition findings by computed tomography in SARS-CoV-2 patients: increased risk of muscle wasting in obesity. Int J Mol Sci. 2020;21(13):4670. doi: 10.3390/ijms21134670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lidoriki I, Frountzas M, Schizas D. Could nutritional and functional status serve as prognostic factors for COVID-19 in the elderly? Med Hypotheses. 2020;144:109946. doi: 10.1016/j.mehy.2020.109946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Silva DFO, Lima SCVC, Sena-Evangelista KCM, Marchioni DM, Cobucci RN, Andrade FB. Nutritional risk screening tools for older adults with COVID-19: a systematic review. Nutrients. 2020;12(10):E2956. doi: 10.3390/nu12102956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abugroun A, Nayyar A, Abdel-Rahman M, Patel P. Impact of malnutrition on hospitalization outcomes for older adults admitted for sepsis. Am J Med. 2020. doi: 10.1016/j.amjmed.2020.06.044 [DOI] [PubMed] [Google Scholar]
- 6.Cederholm T, Barazzoni R, Austin P, et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr. 2017;36(1):49–64. doi: 10.1016/j.clnu.2016.09.004 [DOI] [PubMed] [Google Scholar]
- 7.Bolayir B, Arik G, Yeşil Y, et al. Validation of nutritional risk screening-2002 in a hospitalized adult population. Nutr Clin Pract. 2019;34(2):297–303. doi: 10.1002/ncp.10082 [DOI] [PubMed] [Google Scholar]
- 8.Chávez-Tostado M, Cervantes-Guevara G, López-Alvarado SE, et al. Comparison of nutritional screening tools to assess nutritional risk and predict clinical outcomes in Mexican patients with digestive diseases. BMC Gastroenterol. 2020;20(1):79. doi: 10.1186/s12876-020-01214-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu G, Zhang S, Mao Z, Wang W, Hu H. Clinical significance of nutritional risk screening for older adult patients with COVID-19. Eur J Clin Nutr. 2020;74(6):876–883. doi: 10.1038/s41430-020-0659-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu D, Cui P, Zeng S, et al. Risk factors for developing into critical COVID-19 patients in Wuhan, China: a multicenter, retrospective, cohort study. EClinicalMedicine. 2020;25:100471. doi: 10.1016/j.eclinm.2020.100471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ou M, Zhu J, Ji P, et al. Risk factors of severe cases with COVID-19: a meta-analysis. Epidemiol Infect. 2020;148:e175. doi: 10.1017/S095026882000179X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kondrup J, Rasmussen HH, Hamberg O, Stanga Z. Ad Hoc ESPEN Working Group. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr. 2003;22(3):321–336. doi: 10.1016/S0261-5614(02)00214-5 [DOI] [PubMed] [Google Scholar]
- 13.Grundmann O, Yoon SL, Williams JJ. The value of bioelectrical impedance analysis and phase angle in the evaluation of malnutrition and quality of life in cancer patients–a comprehensive review. Eur J Clin Nutr. 2015;69(12):1290–1297. doi: 10.1038/ejcn.2015.126 [DOI] [PubMed] [Google Scholar]
- 14.Bansal N, Zelnick LR, Himmelfarb J, Chertow GM. Bioelectrical impedance analysis measures and clinical outcomes in CKD. Am J Kidney Dis. 2018;72(5):662–672. doi: 10.1053/j.ajkd.2018.03.030 [DOI] [PubMed] [Google Scholar]
- 15.Barak N, Wall-Alonso E, Cheng A, Sitrin D. Use of bioelectrical impedance analysis to predict energy expenditure of hospitalized patients receiving nutrition support. JPEN J Parenter Enteral Nutr. 2003;27(1):43–46. doi: 10.1177/014860710302700143 [DOI] [PubMed] [Google Scholar]
- 16.Lukaski HC, Vega Diaz N, Talluri A, et al. Classification of hydration in clinical conditions: indirect and direct approaches using bioimpedance. Nutrients. 2019;11(4):809. doi: 10.3390/nu11040809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moon JR, Tobkin SE, Smith AE, et al. Percent body fat estimations in college men using field and laboratory methods: a three-compartment model approach. Dyn Med. 2008;7(1):7. doi: 10.1186/1476-5918-7-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pironi L, Sasdelli AS, Ravaioli F, et al. Malnutrition and nutritional therapy in patients with SARS-CoV-2 disease. Clin Nutr. 2020;27 S0261-5614(20)30437-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Piccoli A. Identification of operational clues to dry weight prescription in hemodialysis using bioimpedance vector analysis. The Italian Hemodialysis-Bioelectrical Impedance Analysis (HD-BIA) Study Group. Kidney Int. 1998;53(4):1036–1043. doi: 10.1111/j.1523-1755.1998.00843.x [DOI] [PubMed] [Google Scholar]
- 20.Schaible UE, Kaufmann SHE. Malnutrition and infection: complex mechanisms and global impacts. PLoS Med. 2007;4(5):e115. doi: 10.1371/journal.pmed.0040115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sharma A, Garg A, Rout A, Lavie CJ. Association of obesity with more critical illness in COVID-19. Mayo Clin Proc. 2020;95(9):2040–2042. doi: 10.1016/j.mayocp.2020.06.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kwok S, Adam S, Ho JH, et al. Obesity: A critical risk factor in the COVID-19 pandemic. Clin Obes. 2020;e12403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lim SL, Ong KC, Chan YH, Loke WC, Ferguson M, Daniels L. Malnutrition and its impact on cost of hospitalization, length of stay, readmission and 3-year mortality. Clin Nutr. 2012;31(3):345–350. doi: 10.1016/j.clnu.2011.11.001 [DOI] [PubMed] [Google Scholar]
- 24.Kyle UG, Genton L, Pichard C. Hospital length of stay and nutritional status. Curr Opin Clin Nutr Metab Care. 2005;8(4):397–402. doi: 10.1097/01.mco.0000172579.94513.db [DOI] [PubMed] [Google Scholar]
- 25.Lingsma HF, Bottle A, Middleton S, Kievit J, Steyerberg EW, Marang-van de Mheen PJ. Evaluation of hospital outcomes: the relation between length-of-stay, readmission, and mortality in a large international administrative database. BMC Health Serv Res. 2018;18(1):116. doi: 10.1186/s12913-018-2916-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Asher RAJ. The dangers of going to bed. BMJ. 1947;ii:867–868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kandula P, Wenzel R. Postoperative wound infection after total abdominal hysterectomy: a controlled study of the increased duration of hospital stay and trends in postoperative wound infection. Am J Infect Control. 1993;21(4):201–204. doi: 10.1016/0196-6553(93)90032-Y [DOI] [PubMed] [Google Scholar]
- 28.Chen L, Li Q, Zheng D, et al. Clinical characteristics of pregnant women with Covid-19 in Wuhan, China. N Engl J Med. 2020;382(25):e100. doi: 10.1056/NEJMc2009226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Guan WJ, Ni ZY, Hu Y, et al. China medical treatment expert group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Occelli C, Contenti J. Early warning scores: are they clinically relevant? Eur J Emerg Med. 2020;27(5):325–326. [DOI] [PubMed] [Google Scholar]
- 31.Myrstad M, Ihle-Hansen H, Tveita AA, et al. National Early Warning Score 2 (NEWS2) on admission predicts severe disease and in-hospital mortality from Covid-19 – a prospective cohort study. Scand J Trauma Resusc Emerg Med. 2020;28(1):66. doi: 10.1186/s13049-020-00764-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weng Z, Chen Q, Li S, et al. ANDC: an early warning score to predict mortality risk for patients with Coronavirus disease 2019. J Transl Med. 2020;18(1):328. doi: 10.1186/s12967-020-02505-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McAlister FA, Majumdar SR, Blitz S, Rowe BH, Romney J, Marrie TJ. The relation between hyperglycemia and outcomes in 2471 patients admitted to the hospital with community-acquired pneumonia. Diabetes Care. 2005;28(4):810–815. doi: 10.2337/diacare.28.4.810 [DOI] [PubMed] [Google Scholar]
- 34.Singh AK, Singh R. Hyperglycemia without diabetes and new-onset diabetes are both associated with poorer outcomes in COVID-19. Diabetes Res Clin Pract. 2020;167:108382. doi: 10.1016/j.diabres.2020.108382 [DOI] [PMC free article] [PubMed] [Google Scholar]