Abstract
Objectives
This study examined the association between alcohol consumption trajectory and deaths due to cancer, cardiovascular diseases (CVDs) and all-cause mortality in Thailand.
Design
Data were obtained from a Thai prospective cohort study with more than 30 years of follow-up (n=1961).
Setting
All participants resided in Bangkok and its vicinity.
Participants
Employees from the Electricity Generating Authority of Thailand aged between 35 and 54 years old were randomly selected.
Main outcome measures
Exposure was alcohol consumption trajectory over the study period from 1985 to 2012. The main outcomes were all-cause mortality, and deaths due to cancer and CVDs recorded in national vital registries between 2002 and 2015. Cox’s proportional hazard regression was used to determine the associations between alcohol consumption trajectory and each outcome adjusting for sample characteristics, health behaviours and health conditions.
Results
From a total of 59 312 person years, 276 deaths were observed. Compared with drinkers who drank occasionally or most occasional over their lifetime, consistent regular or mostly consistent-regular drinkers had higher rates of all-cause mortality (HR: 1.53; 95% CI 1.09 to 2.16) and cancer mortality (HR: 2.05; 95% CI 1.13 to 3.74). The study did not find a significant association between trajectory of alcohol consumption and deaths due to CVDs.
Conclusions
Regular drinking of alcohol increased risk for all-cause and cancer mortality. Effective interventions should be implemented to reduce number of regular drinkers in order to saves life of individuals.
Keywords: coronary heart disease, cancer pain, substance misuse
Strengths and limitations of this study.
This study is among the very first studies in low-income and middle-income countries that investigated a relationship between trajectory of alcohol drinking and death due to cancer, cardiovascular diseases and all causes using a longitudinal study design with 30-year follow-up period.
Our study captured the changes of alcohol consumption pattern in the five study waves.
The participants of our study are mainly employees from the Electricity Generating Authority of Thailand; therefore, it may not well represent the whole Thai population.
Introduction
Alcohol consumption has negative impacts on individuals and society. To individuals, alcohol is causally linked with several diseases such as liver cirrhosis,1 fetal alcohol spectrum disorders2 and alcohol use disorder.3 Moreover, alcohol is attributed to more than 230 diseases and injuries such as cancer, tuberculosis and diabetes. The WHO reported that alcohol is one of the four main risk factors that contribute to non-communicable diseases and one in every six people die from alcohol.4 Within a society, alcohol is related to crimes,5 domestic violence,6 road traffic accidents7 and reduction of productivity at the workplace.8
With regards to existing evidence, in high-income countries, an association between alcohol consumption and alcohol-related mortality is well documented. For example, empirical studies confirmed the association between alcohol consumption and deaths due to cancer,9 liver cirrhosis10 and all causes with the risk of death increasing with increasing alcohol consumption.11 However, a recent meta-analysis reported a slight protective effect of cancer for light drinkers in some studies.9 Other studies found a protective effect of moderate drinkers on cardiovascular diseases (CVDs).12–15 For example, a study in eight European countries found that drinking 15.0–29.9 g of pure alcohol per day reduced the hazard rates of non-fatal coronary heart disease by 0.74 times compared with drinking alcohol 0.1–4.9 g/day.15 However, heavy drinking (more than 60 g of pure alcohol per day) was found to increase the risk of ischaemic heart disease.16 Another study by O’Neil et al17 investigated association between trajectory of alcohol drinking and heart diseases across different cohort studies in the UK and France. The study found that consistent abstainers and ex-drinkers found to be at greater risk of coronary heart diseases relative to consistent moderate drinkers. In addition, study in Melbourne found that light-to-moderate drinkers were protective effect of all-cause mortality.18
In Thailand, there were studies that reported a significant association between alcohol consumption and cancer and circulatory disease among ex-drinkers,19 between alcohol consumption and obesity, hypertension and liver disease among heavy drinkers.20 However, those studies have some methodological limitations. For example, the prospective cohort study by Kamsa-ard et al,19 conducted in underdeveloped region, did not account for level of alcohol consumption but focusing on status of drinking. Another study by Wakabayashi et al20 applied a cross-sectional survey instead of a more scientifically rigorous design, like a cohort survey. More importantly, those studies did not take into account changes of drinking patterns across time.
Considering country context, there is limited evidence quantifying the effect of alcohol consumption trajectory on alcohol-related mortality, particularly in low-income and middle-income countries. Drinking patterns of a population in a high-income country context and Thai context are likely to be differed. Thai drinkers are mostly occasional drinkers21 and abstention rates are higher in Thailand compared with high-income countries.4 Thus, the differences in drinking patterns between high-income countries and Thailand may yield different results.
The objective of the study is to examine associations between alcohol consumption trajectory and all-cause mortality, and deaths due to cancer and CVDs. Our hypothesis is that maintained regular drinkers are more likely to die from all causes, cancer and CVDs compared with those who drink occasionally over their lifetime.
Methods
Data source
We used secondary data from the Electricity Generating Authority of Thailand (EGAT) prospective cohort study, which began the recruitment of the participants in 1985. Employees of EGAT were about 35–54 years of age and were randomly selected. All participants resided in Bangkok and its vicinity. The total sample size was 3482.
There were five waves of data collection: wave 1 in 1985, wave 2 in 1997, wave 3 in 2002, wave 4 in 2007 and wave 5 in 2012.22 The number of deaths was followed from 2002 to 2015. Data collected from the EGAT employees were linked with the national vital registration database using national identification numbers. The causes of death were later verified by trained staff of EGAT.
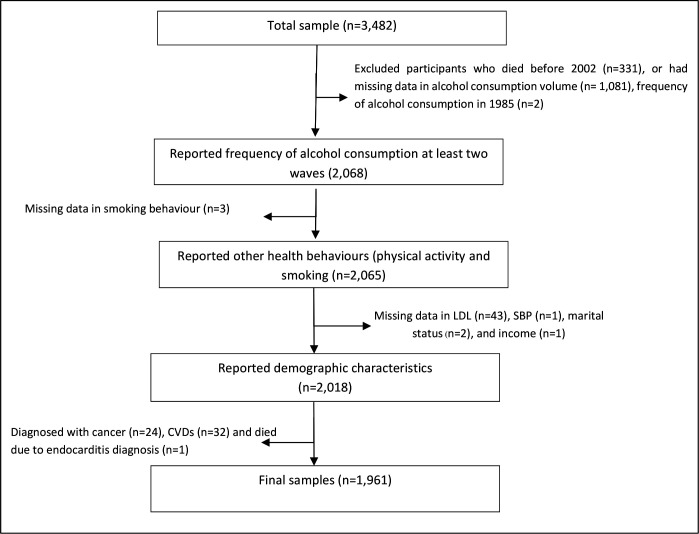
Figure 1 shows a flow chart of the study. We excluded those who died before 2002 (n=331), those who had missing data in volume of alcohol consumption in 2002 (n=1081), and frequency of drinking in 1985 (n=2). We also dropped some records that missed some key variables: smoking behaviour (n=3), low-density lipoprotein (LDL) (n=43), systolic blood pressure (SBP) (n=1), marital status (n=2) and income (n=1). We also excluded those who were diagnosed with cancer (n=24) and CVDs (n=32) and died from Endocarditis (n=1) from the beginning of the cohort. This made our final sample size amounted to 1961.
Figure 1.
Flow chart of study sample. CVDs, cardiovascular diseases; LDL, low-density lipoprotein; SBP, systolic blood pressure.
Exposures
The main exposure variable was alcohol consumption trajectory over the study period, which computed from patterns of drinking in the five study waves. In each wave, respondents were asked how often they drank any kinds of alcoholic beverages in the past year with possible responses, namely (1) daily, (2) 4–6 times per week, (3) 2–3 times per week, (4) 1 time per week, (5) 2–3 times a month or less, (6) ever drunk but stopped drinking in the past year and (7) never drunk. Based on this information, pattern of drinking in each wave was categorised into four categories: (1) regular drinkers-those who drink on a weekly basis, (2) occasional drinkers-those who drink less than once a week, (3) ex-drinkers-those who ever drunk, but stopped drinking in the past year and (4) abstainers are those who abstain drinking throughout the lifetime (see online supplemental table S1). Then, alcohol consumption trajectory was computed from pattern of drinking available in at least two waves as described in table 1. The categorisation was applied from previous literature.17 For those who died before year 2012, we used data in the last wave that they still survived. For those who changed the drinking patterns across the study waves, we classified them according to the drinking pattern that appeared most. We combined consistent-occasion drinkers with mostly consistent-occasion drinkers due to small sample size of consistent-occasion drinking group.
Table 1.
Definition and category of alcohol consumption trajectory
| Category of trajectory of drinking | Definition |
| Consistent-regular drinkers/mostly consistent-regular drinkers | Drinkers who drink alcohol regularly in all study waves or drinkers identifying themselves as regular drinkers in three to four out of five study waves or at least 50% of the study waves |
| Consistent-occasional/mostly consistent-occasional drinkers | Drinkers who drink alcohol occasionally in all study waves or those who reported themselves as occasional drinkers in at least three out of five study waves |
| Ex-drinkers with less regular/less occasional drinking history | Drinkers who reported regular or occasional drinking patterns up to two out of five study waves and stopped drinking in the last waves |
| Maintaining abstainers | Respondents who never drink in their lifetime/reported abstention from drinking in all study waves |
bmjopen-2020-038198supp001.pdf (60.5KB, pdf)
Outcomes
There were three main outcomes of this study: all-cause mortality and deaths due to cancer and CVD (see International Classification of Diseases, Tenth Revision (ICD-10) codes in online supplemental table S2).
Covariates
We included all covariates collected at baseline, year 1895, included gender, age, marital status, educational status, individual income at baseline, smoking behaviour, physical activity and blood pressure (systolic blood pressure and diastolic blood pressure), drinking level of alcohol consumption in 2002, low-density lipoprotein (LDL) level, high-density lipoprotein (HDL) level and body mass index (BMI). To avoid recall bias, blood pressure, LDL, HDL and BMI (weight and height) were measured by medical examination. For smoking behaviours, respondents were asked about their smoking experiences by provided choices: (1) never smoked (2) smoked and then quit (3) occasional smokers and (4) regular smokers. Participants answering (3) or (4) would be further asked about the number of cigarettes per day by provided choices: (1) less than 10 cigarettes, (2) 10–20 cigarettes and (3) 21–40 cigarettes. Subsequently, we categorised smokers into four different categories: (1) those who never smoked, (2) light smokers referring to those who smoked less than 10 cigarettes a day, (3) heavy smokers referring to those who smoked more than 10 cigarettes a day and (4) ex-smokers referring to who had ever smoked but quit more than a year. Physical activities were measured by asking respondents on their engagement in various types of sports in weekly period and categorised them as (1) never, (2) sometimes (1 times/week), (3) 2 times/week, and (4) 3 times or more in a week. We estimated frequency of physical activities by summing up frequency of all sports involved.
Drinking level of alcohol consumption was estimated from volume of alcohol consumption in 2002. In year 2002, respondents were asked about frequency of alcohol consumption, quantify per drinking occasion (either beer or spirits or wine) over the past years. The frequency includes (1) 2–3 times/month, (2) once a week, (3) 2–3 times/week, (4) 4–6 times/week, and (5) every day. We estimated pure alcohol from those questions based on calculation methods suggested by WHO.21 We calculated amount of alcohol consumed per day and classified participants into (1) abstainers (2) light to moderate drinkers (1–40 g/day for females and 1–60 g/day for males), (3) heavy drinkers (more than 40 g/day for females and more than 60 g/day for males), and (4) ex-drinkers.22 We found that there was a due amount of missing data in alcohol consumption data (about 34% of the total samples). However, we found that characteristics of samples with complete dataset and those with missing data on alcohol consumption did not show a marked difference; see more details in online supplemental table S3. Therefore, we proceeded a complete case analysis on the data.
Data analysis
We used Stata V.12 to analyse the data (license number: 401406358220).
Descriptive analysis
We calculated means and SD to present the distribution of continuous variables and frequency and percentage for categorical variables.
Inferential analysis
Time-to-event variable was computed for each study outcomes from starting date in 1985 to death date or censored at the last date respondents participated in the study cohort or until 2015. Survival analysis was performed to analyse this time-to-event data.
We employed Cox’s proportional hazard regression to investigate associations between alcohol consumption trajectory and the three outcomes: death (from all causes), cancer and CVDs. To take drinking level into account, alcohol consumption volume in 2002 was included. The final model adjusted for covariate collected at baseline, including gender, age, marital status, education, monthly income, smoking status, physical activity, LDL, HDL and BMI to control for confounding effects.
Informed consent was signed by all EGAT study participants and all were informed about the objectives and their rights to withdraw from the study at any time.
Patient and public involvement
No patient involved.
Results
Sample characteristics
Of the 1961 respondents, the majorities were male (78%), married (87%), completed vocational school (37%), reported monthly income between 5000 and 10 000 baht (39%), had never smoked (44%) and were consistent-occasional drinkers or mostly consistent-occasional drinkers (32%) and being light-to-moderate drinkers (48%). The average daily alcohol consumption was 31 g/day. Most respondents were physically active and had normal BMI. LDL level at baseline was 148 mg/dL and HDL 47 mg/dL (table 2).
Table 2.
Characteristics of respondents at baseline
| Characteristics | n (%) |
| Gender | |
| Male | 1539 (78.48) |
| Female | 422 (21.52) |
| Age (year), mean (SD) | 42.01 (4.77) |
| Marital status | 42.47 (4.83) |
| Single | 158 (8.06) |
| Married | 1709 (87.15) |
| Divorced/widowed/separated | 94 (4.79) |
| Education attainment | |
| Primary school | 313 (15.96) |
| High school | 333 (16.98) |
| Vocational school | 734 (37.43) |
| Bachelor school or higher | 581 (29.63) |
| Monthly income | |
| ≤5000 baht | 323 (16.47) |
| 5000–10 000 baht | 774 (39.47) |
| 10 000–20 000 baht | 757 (38.60) |
| >20 000 baht | 107 (5.46) |
| Smoking status | |
| Never smoked | 864 (44.06) |
| Light smoker | 310 (15.81) |
| Heavy smoker | 500 (25.50) |
| Ex-smoker | 287 (14.64) |
| Drinking level | |
| Abstainers | 483 (24.63) |
| Low-to-moderate drinkers | 941 (47.99) |
| Heavy drinkers | 137 (6.99) |
| Ex-drinkers | 400 (20.40) |
| Alcohol consumption per day (g/day), mean (SD) | 30.90 (71.22) |
| Frequency of physical activity (times/week), mean (SD) | 13.58 (3.47) |
| Systolic blood pressure (mm Hg), mean (SD) | 119.50 (14.82) |
| Diastolic blood pressure (mm Hg), mean (SD) | 74.44 (10.30) |
| Low-density lipoprotein | 147.61 (39.92) |
| High-density lipoprotein | 47.05 (11.15) |
| Body mass index | 23.03 (2.99) |
| Trajectory of alcohol consumption | |
| Consistent-occasion/mostly consistent-occasion drinkers | 646 (32.94) |
| Consistent-regular drinkers/mostly consistent-regular drinkers | 434 (22.13) |
| Less regular/less occasion ex-drinkers | 458 (23.36) |
| Maintaining abstainers | 423 (21.57) |
US$1≈30 baht.
Mortality rates of all causes, cancer and CVDs across trajectory groups of alcohol consumption
The total follow-up time was 59 312 person years and there were 276 deaths, 89 due to cancer, 64 due to CVDs and 123 due to other causes. The mortality rates were 5 deaths per 1000 person years for all causes and 2 deaths per 1000 person years for cancer and 1 death per 1000 person-years for CVDs.
Consistent-regular drinkers or mostly consistent-regular drinkers had the greatest all-cause mortality rate (7 deaths per 1000 person years) followed by ex-drinkers with less regular or less occasional drinking history (5 deaths per 1000 person years), consistent-occasional or mostly consistent-occasional drinkers (4 deaths per 1000 person years) and maintaining abstainers (3 deaths per 1000 person years). Furthermore, consistent-regular or mostly consistent-regular groups had the highest cancer mortality rates (3 deaths per 1000 person years), while maintaining abstainers had the lowest cancer mortality rates (1 death per 1000 person years). In addition, we found that ex-drinkers and consistent-occasional drinkers or mostly consistent-occasional drinkers had the highest CVD mortality rates (1 death per 1000 person years; table 3).
Table 3.
Mortality rates from all causes and cancer and cardiovascular diseases (CVDs)
| Alcohol consumption trajectory | All causes | Cancer | CVDs | ||||||
| Person time (years) | Number of cases | Incidence rate* | Person time (years) | Number of cases | Incidence rate* | Person time (years) | Number of cases | Incidence rate* | |
| Consistent-occasional/mostly consistent-occasional drinkers | 19 614 | 78 | 3.98 | 19 614 | 23 | 1.17 | 19 614 | 24 | 1.22 |
| Consistent-regular drinkers/mostly consistent-regular drinkers | 12 939 | 86 | 6.65 | 12 939 | 36 | 2.78 | 12 939 | 13 | 1.00 |
| Less regular/less occasion ex-drinkers | 13 827 | 74 | 5.35 | 12 933 | 19 | 1.37 | 12 933 | 18 | 1.30 |
| Maintaining abstainers | 12 933 | 38 | 2.94 | 59 312 | 11 | 0.85 | 59 312 | 9 | 0.70 |
| Total | 59 312 | 276 | 4.65 | 19 614 | 89 | 1.50 | 19 614 | 64 | 1.08 |
*Per 1000 person years.
Associations between trajectory of alcohol consumption and deaths from all causes, cancer and CVDs
Table 4 shows the results of the Cox’s proportional hazard regression model predicting death from all causes, cancer and CVDs. After adjusting for all covariates, consistent-regular or mostly consistent-regular drinking group had greater hazard rates of all-cause mortality compared with consistent-occasional or mostly consistent-occasional drinkers (HR: 1.53; 95% CI 1.09 to 2.16). The study also found that consistent-regular or mostly consistent-regular drinkers had greater hazard rates of cancer compared with consistent-occasional drinkers or mostly consistent-occasional drinkers (HR: 2.05; 95% CI 1.13 to 3.74). The study did not find a statistically significant association between trajectory of alcohol consumption and death due to CVDs (table 4).
Table 4.
Associations between alcohol consumption trajectory and deaths from all causes, cancer and cardiovascular diseases (CVD), using Cox’s proportional hazard regression
| All causes | Cancer | CVDs | ||||
| HR (95% CI) | P value | HR (95% CI) | P value | HR (95% CI) | P value | |
| Alcohol consumption trajectory (vs consistent-occasional/mostly consistent-occasional drinkers) | ||||||
| Consistent-regular drinkers/ mostly consistent-regular drinkers | 1.53 (1.09 to 2.16) | 0.014 | 2.05 (1.13 to 3.74) | 0.019 | 0.74 (0.35 to 1.54) | 0.418 |
| Less regular/less occasion ex-drinkers | 0.89 (0.62 to 1.29) | 0.548 | 0.85 (0.42 to 1.69) | 0.635 | 0.86 (0.42 to 1.76) | 0.688 |
| Maintaining abstainers | 1.16 (0.48 to 2.80) | 0.749 | 0.48 (0.15 to 1.60) | 0.233 | 1.62 (0.19 to 13.44) | 0.656 |
| Level of drinking (lifetime abstainers) | ||||||
| Low-to-moderate drinkers | 1.08 (0.46 to 2.53) | 0.864 | 0.50 (0.16 to 1.54) | 0.228 | 1.65 (0.21 to 12.68) | 0.631 |
| Heavy drinkers | 1.03 (0.40 to 2.69) | 0.949 | 0.63 (0.17 to 2.28) | 0.478 | 1.05 (0.10 to 11.12) | 0.970 |
| Former drinkers | 1.67 (0.71 to 3.92) | 0.241 | 0.72 (0.23 to 2.27) | 0.576 | 1.41 (0.18 to 10.93) | 0.745 |
| Gender | ||||||
| Female (vs male) | 0.97 (0.59 to 1.60) | 0.912 | 1.22 (0.53 to 2.84) | 0.639 | 0.39 (0.11 to 1.32) | 0.129 |
| Age (year) | 1.10 (1.07 to 1.13) | <0.001 | 1.07 (1.02 to 1.12) | 0.007 | 1.12 (1.06 to 1.18) | <0.001 |
| Marital status (vs single) | ||||||
| Married | 0.79 (0.49 to 1.27) | 0.340 | 0.65 (0.32 to 1.35) | 0.247 | 1.65 (0.39 to 6.93) | 0.493 |
| Divorced/widowed/separated | 0.80 (0.41 to 1.58) | 0.529 | 0.61 (0.20 to 1.89) | 0.396 | 2.54 (0.47 to 13.73) | 0.278 |
| Education attainment (vs primary school) | ||||||
| High school | 0.94 (0.64 to 1.38) | 0.747 | 0.75 (0.37 to 1.51) | 0.418 | 0.38 (0.14 to 1.04) | 0.060 |
| Vocational school | 1.18 (0.80 to 1.73) | 0.408 | 1.07 (0.54 to 2.14) | 0.838 | 1.38 (0.65 to 2.90) | 0.405 |
| Bachelor school or higher | 0.88 (0.54 to 1.46) | 0.627 | 0.89 (0.37 to 2.13) | 0.787 | 0.99 (0.36 to 2.72) | 0.985 |
| Monthly Income (vs <5000 baht) | ||||||
| 5000–10 000 baht | 0.63 (0.44 to 0.89) | 0.010 | 0.53 (0.29 to 0.97) | 0.041 | 0.60 (0.29 to 1.26) | 0.175 |
| 10 000–20 000 baht | 0.44 (0.28 to 0.69) | <0.001 | 0.39 (0.18 to 0.86) | 0.020 | 0.28 (0.11 to 0.71) | 0.008 |
| >20 000 baht | 0.43 (0.21 to 0.90) | 0.025 | 0.80 (0.25 to 2.54) | 0.709 | 0.34 (0.08 to 1.45) | 0.145 |
| Smoking behaviour | ||||||
| Light smoker | 1.20 (0.77 to 1.85) | 0.417 | 0.82 (0.35 to 1.93) | 0.652 | 1.39 (0.55 to 3.49) | 0.489 |
| Heavy smoker | 2.36 (1.66 to 3.33) | <0.001 | 2.70 (1.48 to 4.91) | 0.001 | 2.98 (1.43 to 6.21) | 0.004 |
| Ex-smoker | 1.80 (1.22 to 2.65) | 0.003 | 1.29 (0.61 to 2.71) | 0.500 | 2.83 (1.30 to 6.18) | 0.009 |
| Average frequency of physical activity (time/week) | 1.03 (1.00 to 1.07) | 0.039 | 1.02 (0.95 to 1.09) | 0.616 | 1.03 (0.98 to 1.09) | 0.255 |
| Systolic blood pressure (mm Hg) | 1.01 (0.99 to 1.02) | 0.302 | 1.00 (0.98 to 1.02) | 0.840 | 1.02 (1.00 to 1.05) | 0.037 |
| Diastolic blood pressure (mm Hg) | 1.02 (1.00 to 1.04) | 0.013 | 1.04 (1.00 to 1.07) | 0.025 | 0.99 (0.96 to 1.03) | 0.598 |
| Low-density lipoprotein | 1.00 (1.00 to 1.00) | 0.933 | 1.00 (1.00 to 1.01) | 0.592 | 1.00 (1.00 to 1.01) | 0.736 |
| High-density lipoprotein | 0.99 (0.98 to 1.01) | 0.356 | 1.00 (0.98 to 1.02) | 0.857 | 1.00 (0.98 to 1.03) | 0.813 |
| Body mass index | 1.05 (1.01 to 1.10) | 0.015 | 1.02 (0.95 to 1.10) | 0.523 | 1.12 (1.03 to 1.21) | 0.008 |
Bold values are statistically significant at p<0.05.
Discussion
Result discussion
Based on a 30-year cohort, this study found that there are associations between alcohol consumption trajectory and death from all causes and cancer, but not for CVDs. People who regularly drink alcohol across the study periods (or in almost all periods) had higher risk of death from all causes and cancer-related deaths than those who drink occasionally.
We found that consistent regular drinkers had greater risk of all-cause mortality than occasional drinkers (either consistent-occasion group or mostly consistent-occasion group), which was consistent with previous study by Malyutina et al.23 Note that our study did not find J-shape relationship between alcohol consumption and deaths from all causes (J-shape relationship refers to high average daily consumption of alcohol had increased risk of death, but moderate drinking relative to abstinence had reduced mortality risk). A study in Melbourne found that people who consistently had light-to-moderate amounts of alcohol drinking tended to have lower risk of all-cause mortality compared with consistent abstainers.18 The explanation for the difference in findings might be that previous study applied volume of alcohol consumption across the entire cohort, but we adjusted volume of alcohol consumption only one study wave due to the limitation in data availability.
The effect of alcohol consumption on cancer-related mortality was statistically significant among consistent-regular drinkers, but not among other drinking groups. This finding coincided with previous study in the USA, which found that heavy drinkers had increased mortality due to cancer compared with lifetime light drinkers. We also found a greater magnitude of association between alcohol consumption and cancer-related deaths compared with previous study by Kunzmann et al.24 The strong association may explain by adherence to regular drinking pattern over long period of time compared with previous study that measured alcohol drinking pattern only in a single wave. Additionally, previous study by Marron et al25 suggested those who had quit drinking for more than 20 years would be protected against cancer; however, our study did not find such effect. The explanation for the differences would be different in study designs, previous study applied case-control studies, and had greater sample size.
We did not find association between drinking patterns and CVDs. Our study found inconsistent finding compared with previous study by O’Neill et al17 which applied similar category of drinking trajectories. Previous study found that consistent abstainers appeared to face a greater risk of coronary heart diseases compared with consistent moderate drinkers. Moreover, the study found inconsistent findings compared with previous study conducted in Thailand by Kamsa-ard et al,19 which found that ex-drinkers were more likely to experience death due to circulatory system relative to never drinkers. This difference could be explained by using different methods in classifying main independent variable: we used trajectory of alcohol consumption measured over time instead of pattern of drinking measured at one point of time.
Strength and limitations
This study was one of few studies to investigate a relationship between trajectory of alcohol drinking and deaths due to cancer, CVDs and all causes using a longitudinal study design in a middle- income country. Results of this study can contribute to knowledge on the association between alcohol consumption and alcohol-related deaths, especially in a middle-income country context.
However, there remain some limitations that need to be acknowledged. First, the EGAT cohort studies recruited only employees of the EGAT; thus, the sample may not be representative of the whole population. Second, we could not separate types of cancer and CVDs due to limitation in number of cases among those diseases and due to the fact that our data followed the ICD-10 list linked to the vital registry, which most of the time lacked of the details of cancer types. This means that the detailed effect of alcohol consumption on different cancer types and CVDs might be overlooked. Finally, there remain other variables that might influence the association between alcohol consumption and death (such as diet, living environment and a genetic predisposition) that had not been included in the analysis.
Conclusion
We found that adherence to regular drinking patterns over period of time was a significant risk factor for all-cause mortality and deaths due to cancer. However, we could not find a significant association between trajectory of alcohol consumption and CVDs. To reduce the number of alcohol-related deaths, interventions or campaigns to reduce the consumption of alcohol should be prioritised for certain group of drinkers who posed the greatest risk of deaths; that is, those who maintain regular drinking pattern.
Supplementary Material
Acknowledgments
The study was funded by Burden of Disease, International Health Policy Program. The authors would like to acknowledge the team of EGAT, particularly Krittika Saranburut and Nisakorn Thongmung. The authors gratefully acknowledge the funding support through the International Health Policy Program (IHPP) from the Thailand Science Research and Innovation (TSRI) under the Senior Research Scholar on Health Policy and System Research (Contract no. RTA6280007). The authors also would like to acknowledge Edward McNeil for editing this work and Patinya Srisai for her support.
Footnotes
Correction notice: This article has been corrected since it was published. Orcid ids of authors have been corrected.
Contributors: JJ, SC, KB and RS designed the study. Statistical analyses were done by JJ, SC and KM. Interpretation of findings, manuscript writing and critical revision was done by JJ, SC, KB, RS and OW. Review and comments were done by KB, RS, SC, OW, KM, PS, PV and CW. Final approval of the submitted manuscript was done by all authors.
Funding: The study was funded by Thai Health Promotion Foundation, grant number 58-00-1875.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The cohort study was approved by the Ethical Clearance Committee on Human Rights Related to Research Involving Human Subjects, Faculty of Medicine, Ramathibodi Hospital, Mahidol University.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data may be obtained from a third party and are not publicly available. All data relevant to the study are included in the article.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.Roerecke M, Vafaei A, Hasan OSM, et al. . Alcohol consumption and risk of liver cirrhosis: a systematic review and meta-analysis. Am J Gastroenterol 2019;114:1574–86. 10.14309/ajg.0000000000000340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Popova S, Lange S, Shield K, et al. . Prevalence of fetal alcohol spectrum disorder among special subpopulations: a systematic review and meta-analysis. Addiction 2019;114:1150–72. 10.1111/add.14598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Griswold MG, Fullman N, Hawley C, et al. . Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the global burden of disease study 2016. The Lancet 2018;392:1015–35. 10.1016/S0140-6736(18)31310-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization Global status report on alcohol and health 2018. Geneva: World Health Organization; 2018. [Google Scholar]
- 5.Greenfield LA. Alcohol and crime: an analysis of national data on prevalence of alcohol involvement in crime. Washington, DC: Bureau of Justice Statistics; 1998. [Google Scholar]
- 6.Chan C. Alcohol issues in domestic violence: Australian domestic and family violence Clearinghouse 2005.
- 7.Herman J, Ameratunga S, Jackson R. Burden of road traffic injuries and related risk factors in low and middle-income Pacific Island countries and territories: a systematic review of the scientific literature (TRIP 5). BMC Public Health 2012;12:479. 10.1186/1471-2458-12-479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thavorncharoensap M, Teerawattananon Y, Yothasamut J, et al. . The economic impact of alcohol consumption: a systematic review. Subst Abuse Treat Prev Policy 2009;4:20. 10.1186/1747-597X-4-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bagnardi V, Rota M, Botteri E, et al. . Alcohol consumption and site-specific cancer risk: a comprehensive dose-response meta-analysis. Br J Cancer 2015;112:580–93. 10.1038/bjc.2014.579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Corrao G, Bagnardi V, Zambon A, et al. . Meta-Analysis of alcohol intake in relation to risk of liver cirrhosis. Alcohol and Alcoholism 1998;33:381–92. 10.1093/oxfordjournals.alcalc.a008408 [DOI] [PubMed] [Google Scholar]
- 11.Stewart D, Han L, Doran T, et al. . Alcohol consumption and all-cause mortality: an analysis of general practice database records for patients with long-term conditions. J Epidemiol Community Health 2017;71:729–35. 10.1136/jech-2017-209241 [DOI] [PubMed] [Google Scholar]
- 12.Larsson SC, Wallin A, Wolk A. Alcohol consumption and risk of heart failure: meta-analysis of 13 prospective studies. Clin Nutr 2018;37:1247–51. 10.1016/j.clnu.2017.05.007 [DOI] [PubMed] [Google Scholar]
- 13.Corrao G, Rubbiati L, Bagnardi V, et al. . Alcohol and coronary heart disease: a meta-analysis. Addiction 2000;95:1505–23. 10.1046/j.1360-0443.2000.951015056.x [DOI] [PubMed] [Google Scholar]
- 14.Zhao J, Stockwell T, Roemer A, et al. . Alcohol consumption and mortality from coronary heart disease: an updated meta-analysis of cohort studies. J Stud Alcohol Drugs 2017;78:375–86. 10.15288/jsad.2017.78.375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ricci C, Wood A, Muller D, et al. . Alcohol intake in relation to non-fatal and fatal coronary heart disease and stroke: EPIC-CVD case-cohort study. BMJ 2018;361:k934. 10.1136/bmj.k934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roerecke M, Rehm J. Chronic heavy drinking and ischaemic heart disease: a systematic review and meta-analysis. Open Heart 2014;1:e000135. 10.1136/openhrt-2014-000135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O’Neill D, Britton A, Hannah MK, et al. . Association of longitudinal alcohol consumption trajectories with coronary heart disease: a meta-analysis of six cohort studies using individual participant data. BMC Med 2018;16:124. 10.1186/s12916-018-1123-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jayasekara H, MacInnis RJ, Hodge AM, et al. . Alcohol consumption for different periods in life, intake pattern over time and all-cause mortality. J Public Health 2015;37:fdu082–33. 10.1093/pubmed/fdu082 [DOI] [PubMed] [Google Scholar]
- 19.Kamsa-ard S, Promthet S, Lewington S, et al. . Alcohol consumption and mortality: the Khon Kaen cohort study, Thailand. J Epidemiol 2014;24:154–60. 10.2188/jea.JE20130092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wakabayashi M, McKetin R, Banwell C, et al. . Alcohol consumption patterns in Thailand and their relationship with non-communicable disease. BMC Public Health 2015;15:1297. 10.1186/s12889-015-2662-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Statistical Office The smoking and drinking behaviour survey 2017. Bangkok: National Statistical Office; 2017. [Google Scholar]
- 22.Vathesatogkit P, Woodward M, Tanomsup S, et al. . Cohort profile: the electricity generating authority of Thailand study. Int J Epidemiol 2012;41:359–65. 10.1093/ije/dyq218 [DOI] [PubMed] [Google Scholar]
- 23.Malyutina S, Bobak M, Kurilovitch S, et al. . Relation between heavy and binge drinking and all-cause and cardiovascular mortality in Novosibirsk, Russia: a prospective cohort study. Lancet 2002;360:1448–54. 10.1016/S0140-6736(02)11470-X [DOI] [PubMed] [Google Scholar]
- 24.Kunzmann AT, Coleman HG, Huang W-Y, et al. . The association of lifetime alcohol use with mortality and cancer risk in older adults: a cohort study. PLoS Med 2018;15:e1002585. 10.1371/journal.pmed.1002585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marron M, Boffetta P, Zhang Z-F, et al. . Cessation of alcohol drinking, tobacco smoking and the reversal of head and neck cancer risk. Int J Epidemiol 2010;39:182–96. 10.1093/ije/dyp291 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-038198supp001.pdf (60.5KB, pdf)