Abstract
Background
Montefiore Medical Center (MMC) is a large tertiary care center in the Bronx, New York City, with 245 internal medicine residents. Beginning on February 29, 2020, residents became ill with COVID-19-like illness (CLI), which required absence from work. There was initially a shortage of personal protective equipment and delays in SARS-CoV-2 testing, which gradually improved during March and April 2020.
Objective
We evaluated the relationship between CLI-related work absence rates of internal medicine residents and MMC's COVID-19 hospital census over time.
Methods
Data on resident work absence between February 29 and May 22 were reviewed along with MMC's COVID-19 hospital census data. To determine the effect of patient exposure on resident CLI incidence, we compared the mean incidence of CLI per patient exposure days (PED = daily hospital census × days pre- or post-peak) before and after peak COVID-19 hospital census.
Results
Forty-two percent (103 of 245) of internal medicine residents were absent from work, resulting in 875 missed workdays. At the peak of resident work absence, 16% (38 of 245) were out sick. Residents were absent for a median of 7 days (IQR 6–9.5 days). Mean resident CLI incidence per PED (CLI/PED) was 13.9-fold lower post-peak compared to pre-peak (P = .003).
Conclusions
At the beginning of the COVID-19 pandemic in New York City, a large portion of internal medicine residents at this single center became ill. However, the incidence of CLI decreased over time, despite ongoing exposure to patients with COVID-19.
Introduction
In March 2020, New York City became an epicenter of the COVID-19 pandemic.1 Montefiore Medical Center (MMC) is a tertiary care center in the Bronx, New York City, with 2 internal medicine residency programs comprised of 245 physicians. Beginning on February 29, 2020, internal medicine residents became ill with fever and/or respiratory symptoms consistent with COVID-19-like illness (CLI) requiring absence from work, in accordance with current CDC recommendations at the time. Initially, there was limited access to diagnostic testing for both health care workers and patients in the New York area.2 Residents with COVID-19 or CLI without SARS-CoV-2 testing were quarantined at home for 7 days from the onset of symptoms or 3 days from the time of last fever, whichever was longer.3 Initially, there were national and regional shortages of personal protective equipment (PPE), such as N-95 masks, gowns, and face shields, which improved during March and April 2020.4 We evaluated the relationship between CLI-related work absence rates of internal medicine residents and MMC's COVID-19 hospital census.
Methods
Residents who were out sick with CLI were tracked in real-time to maintain pre-pandemic staffing levels across inpatient services. These data were reviewed retrospectively along with MMC's COVID-19 hospital census data. New York City incidence data were obtained from public records.1 To determine the effect of patient exposure on resident CLI incidence, we compared the mean incidence of CLI per patient exposure days (PED = daily hospital census × days pre- or post-peak) before and after peak COVID-19 hospital census using a t test with R software, version 3.5.1 (R Foundation). This index compares resident CLI incidence with the burden of patient exposure as approximated by the COVID-19 patient census and is a useful way to track resident illness over time with data that are readily available. The CLI/PED index accounts for inpatient COVID-19 volume and was therefore chosen over patient exposure hours alone, which would not consider the degree of exposure to patients with COVID-19. Use of the hospital census peak as a natural cut-off point allowed for evaluation of pre-peak interventions to minimize COVID-19 exposure in aggregate, despite approximately similar PED.
This study was approved by the Albert Einstein College of Medicine Institutional Review Board.
Results
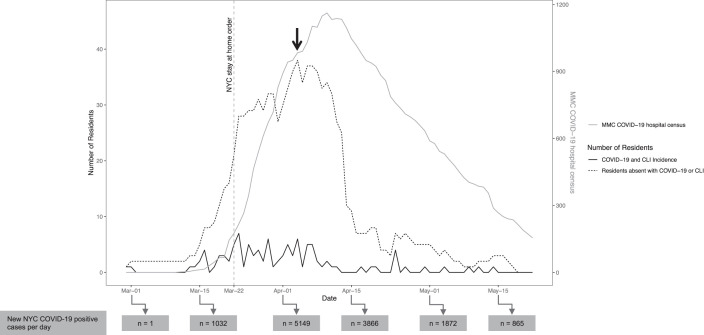
Between February 29 and May 22, 2020, 42% (103 of 245) of internal medicine residents were absent from work due to COVID-19 or CLI, resulting in 875 missed workdays. Residents were absent for a median of 7 days (interquartile range 6–9.5 days). Seventy-seven percent of sick residents (n = 79) underwent SARS-CoV-2 RNA testing by nasopharyngeal swab and 53% (n = 42) tested positive. There were no fatalities, but 2% (n = 2) of sick residents required hospitalization. Two residents were absent with CLI on March 10 before there were any patients with COVID-19 at MMC. Resident absence peaked at 16% (n = 38) on April 4, then sharply declined despite a rising COVID-19 hospital census (Figure). The incidence of CLI for residents declined before the hospital COVID-19 census peak. We compared resident CLI incidence per PED (CLI/PED) before and after the MMC COVID-19 census peak and found that mean post-peak CLI/PED was 13.9-fold lower (P = .003) than mean pre-peak CLI/PED (Figure provided as supplemental material).
Figure.
Montefiore Medical Center COVID-19 Inpatient Census and Resident Quarantine Experience
Note: The left y-axis describes the number of residents absent and the incidence of new resident COVID-19 or COVID-19-like illness (CLI). Resident absence peaked at 16% (n = 38) on April 4, 2020 (black arrow). The right y-axis describes the number of COVID-19 positive patients admitted to MMC per day. At the peak of the COVID-19 census, MMC increased its inpatient capacity from 1558 to 1923 beds. New York City COVID-19 incidence data are shown at the bottom.
Discussion
Forty-two percent of residents from 2 large urban internal medicine residency programs experienced absences from work due to COVID-19 or CLI. Internal medicine residents are an at-risk population during a respiratory viral pandemic given their direct exposure to patients. Resident illness prior to confirmed inpatient cases suggests that community spread, in addition to occupational exposure, might have contributed. We also found a statistically significant decrease in the incidence of residents with COVID-19 and CLI after the peak of the hospital COVID-19 census compared to before, despite similar levels of patient exposure. These findings have implications for future outbreaks and for residency programs that have not yet been severely affected by the COVID-19 pandemic.
The decrease in resident CLI post-peak was likely related to multiple measures taken to decrease disease transmission, including rapid patient and employee testing, limiting conference room capacity, delivering conferences using video conferencing software, suspending bedside rounds, the citywide stay at home order,5 increased availability of PPE, and distributing PPE at hospital entrances. PPE availability improved throughout March and April as supply to our region improved, as well as when the distribution was systematized, and staff were instructed on how to reuse PPE. Furthermore, turnaround time for COVID-19 testing decreased throughout March and April as the hospital laboratory developed its own assay.
This study raises several questions for future studies of resident illness during the COVID-19 pandemic and perhaps other outbreaks. A robust sick resident coverage system was vital for maintaining resident and patient safety. In anticipation of large numbers of resident absences, all residents were removed from electives, subspecialty rotations, and outpatient clinics, which were closed for in-person visits in early March (in conjunction with Accreditation Council for Graduate Medical Education emergency pandemic status). This created a pool of internal medicine residents available for 2 innovative system changes: surge staffing and an expanded sick resident coverage system. We created a new call schedule, converting from 6 days on with 1 day off to 7 days on with 7 days of combined off time and sick resident coverage time. These scheduling changes facilitated the creation of the 24 new teams that were needed during the COVID-19 surge, increasing our total inpatient team count from 20 to 44 teams. The surge staffing structure consisted of a minimum of 4 residents per 12-patient ICU team and decreased general medical floor teams from 3 residents per 16 patients to 2 or 3 residents per 12 patients. The general medical floor intern cap of 8 patients was decreased to 6 patients due to the overall higher acuity of most COVID-19 patients. In order to staff 24 new teams, non-internal medicine residents were recruited to join ward teams and function as internal medicine interns. These residents came from a wide range of training programs, including radiology, physiatry, psychiatry, podiatry, orthopedic surgery, dermatology, radiation oncology, and urology. This was unprecedented for our institution and was a novel solution required to care for the expanded volume of medical inpatients, most of whom had COVID-19. Later in the surge, fourth-year medical students who graduated early volunteered to join this surge staffing system.
This study has limitations. We did not have access to data on PPE use among residents. In future studies, data on resident access to PPE and reuse of PPE should be collected prospectively to determine need and impact of this equipment. In addition, the data from this study represent a single center dramatically affected by the COVID-19 pandemic and might not be generalizable to other medical centers.
Conclusions
At the start of the COVID-19 pandemic in New York City, our residency programs were seriously affected by CLI and work absences. The incidence of CLI among internal medicine residents decreased over time, despite ongoing exposure to patients with COVID-19.
Supplementary Material
Footnotes
Funding: The authors report no external funding source for this study.
Conflict of interest: The authors declare they have no competing interests.
The authors would like to thank William Southern, MD, for his assistance in revising this manuscript.
Contributor Information
Ross Merkin, Chief Resident, Moses/Weiler Internal Medicine Residency, Albert Einstein College of Medicine and Montefiore Medical Center.
Ariel Kruger, Instructor, Department of Ecology, Evolution, and Natural Resources, Rutgers University.
Gaurav Bhardwaj, Chief Resident, Wakefield Internal Medicine Residency, Albert Einstein College of Medicine and Montefiore Medical Center.
Grace R. Kajita, Program Director, Wakefield Internal Medicine Residency, and Assistant Professor, Department of Internal Medicine, Division of General Internal Medicine, Albert Einstein College of Medicine and Montefiore Medical Center.
Lauren Shapiro, Program Director, Montefiore/Weiler Internal Medicine Residency, and Associate Professor, Department of Internal Medicine, Division of General Internal Medicine, Albert Einstein College of Medicine and Montefiore Medical Center.
Benjamin T. Galen, Associate Program Director, Montefiore/Weiler Internal Medicine Residency, and Associate Professor, Department of Internal Medicine, Division of Hospital Medicine, Albert Einstein College of Medicine and Montefiore Medical Center.
References
- 1.Health NYC. Covid19 Data. 2020 https://www1.nyc.gov/site/doh/covid/covid-19-data.page Accessed October 8.
- 2.Goldstein J, Ferré-Sadurní L, Randle A. Coronavirus in N.Y.: Desperate for a Test, They Couldn't Get One. The New York Times. 2020 https://www.nytimes.com/2020/03/11/nyregion/coronavirus-testing-newyork.html Accessed October 8.
- 3.Centers for Disease Control and Prevention. Criteria for Return to Work for Healthcare Personnel with Suspected or Confirmed COVID19 (Interim Guidance) 2020 https://www.cdc.gov/coronavirus/2019-ncov/hcp/return-to-work.html Accessed October 8.
- 4.Ranney M, Griffeth V, Jha A. Critical supply shortages—the need for ventilators and personal protective equipment during the Covid-19 pandemic. N Engl J Med. 2020;382(18):e41. doi: 10.1056/NEJMp2006141. [DOI] [PubMed] [Google Scholar]
- 5.New York State. New York State on PAUSE. 2020 https://coronavirus.health.ny.gov/new-york-state-pause Accessed October 8.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.