Abstract
As the COVID‐19 pandemic unfolds, emergency department (ED) personnel will face a higher caseload, including those with special medical needs such as persons living with spinal cord injuries and disorders (SCI/D). Individuals with SCI/D who develop COVID‐19 are at higher risk for rapid decompensation and development of acute respiratory failure during respiratory infections due to the combination of chronic respiratory muscle paralysis and autonomic dysregulation causing neurogenic restrictive/obstructive lung disease and chronic immune dysfunction. Often, acute respiratory infections will lead to significant mucus production in individuals with SCI/D, and aggressive secretion management is an important component of successful medical treatment. Secretion management techniques include nebulized bronchodilators, chest percussion/drainage techniques, manually assisted coughing techniques, nasotracheal suctioning, and mechanical insufflation–exsufflation. ED professionals, including respiratory therapists, should be familiar with the significant comorbidities associated with SCI/D and the customized secretion management procedures and techniques required for optimal medical management and prevention of respiratory failure. Importantly, protocols should also be implemented to minimize potential COVID‐19 spread during aerosol‐generating procedures.
Keywords: COVID‐19, paraplegia, pneumonia, quadriplegia, respiratory failure, spinal cord injury
1. INTRODUCTION
During the COVID‐19 pandemic, emergency department (ED) personnel are facing higher caseloads, including those with special medical needs. Persons with spinal cord injuries and disorders (SCI/D) presenting to the ED with respiratory complaints require special consideration if diagnosed with COVID‐19 because they are at higher risk for rapid decompensation and progression to acute respiratory failure due to the combination of chronic respiratory muscle weakness and autonomic dysregulation, which cause neurogenic restrictive/obstructive lung disease and chronic immune dysfunction. In this review, we highlight the greater susceptibility of persons with SCI/D to death from respiratory infections, describe methods to aide in recognition of respiratory infections including COVID‐19 in persons with SCI/D, and discuss treatment strategies to better manage respiratory complications of COVID‐19 infections in this population.
2. EPIDEMIOLOGY
Almost 300,000 persons in the United States are living with SCI/D. 1 The most common cause of death in this population is pneumonia and respiratory diseases. Persons with SCI/D have greater mortality from pneumonia and influenza compared to the general population with the standardized mortality ratio for pneumonia and influenza for all types of SCI/D calculated approximately 40. 2 , 3 Here, the standardized mortality ratio estimates the ratio between the observed number of deaths in SCI/D patients, or subgroups of SCI/D patients, compared to the expected number of deaths based on age‐ and sex‐specific rates in the general population. The finding that the ratio of observed–expected deaths (the standardized mortality ratio) far exceeds 1.0 indicates that SCI/D patients experience a manyfold higher rate of “excess deaths” from pneumonia and influenza compared to their counterparts without SCI/D. For individuals with complete tetraplegia, and therefore greater respiratory muscle paralysis and secondary respiratory compromise, the risk of death is considerably higher with standardized mortality ratio = 143. 2 Compared to those with incomplete tetraplegia who ambulate, non‐ambulators with C1–C4 tetraplegia are 6 times more likely to die from pneumonia or influenza. 4 Persons with complete paraplegia, preservation of full diaphragm innervation, and at least partial maintenance of accessory muscles of respiration and abdominal musculature, have a lower standardized mortality ratio of 15.2. Those who have been injured for >20 years have standardized mortality ratio = 60. 2 , 5 Additionally, persons with SCI/D are at higher risk of developing venous thromboembolism and pulmonary embolism, with the standardized mortality ratio for pulmonary embolism = 45. 3 Individuals with other neuromuscular diseases causing respiratory muscle weakness such as multiple sclerosis, amyotrophic lateral sclerosis, muscular dystrophies, myotonic dystrophies, spinal muscular atrophies, myasthenia, inflammatory demyelinating polyradiculoneuropathies, and spino‐cerebellar ataxias may be at higher risk of respiratory infection complications and benefit from similar management strategies.
COVID‐19 has infected at least 25,248,595 persons worldwide through August 31, 2020, causing 846,877 deaths. In the United States, as of August 31, 2020, at least 5,997,622 persons have been infected with the virus and 183,068 have died from complications of COVID‐19. 6
The epidemiology of COVID‐19 in persons with SCI/D is incompletely understood but appears to be similar to the general population; there have been a range of presentations from mild to severe disease. 7 , 8 , 9 , 10 , 11 In addition to respiratory weakness, the SCI/D population has a high prevalence of hypertension, coronary artery disease, diabetes, and obesity, which are recognized to increase risk of COVID‐19 complications. 12 , 13 Of 25 cases of COVID‐19 infection reported thus far, one sudden death has been described in a patient with new traumatic SCI/D and mild COVID‐19, 5 cases were described as severe with Modified Early Warning Scale (MEWS) score ≥3 and <5, and the remainder were non‐severe. 7 , 8 , 9 , 10 , 11 Recovery courses have ranged from 10 days to a few months, with older patients with high tetraplegia, tracheostomy, and severe COVID‐19 courses having the slowest recovery. In the general population, deaths from COVID‐19 are associated with the development of acute respiratory infections, sepsis, thromboembolic events, and acute respiratory failure that may be complicated by the acute respiratory distress syndrome (ARDS). 12 A study of COVID‐19 case‐fatality rates in the United States in veterans with traumatic or non‐traumatic SCI/D (not including multiple sclerosis or amyotrophic lateral sclerosis) identified 140 veterans who were positive for COVID‐19 among the 17,452 veterans in the SCI/D Registry. Of these, 26 died, all within 30 days of testing positive. The case‐fatality rate of 19% for veterans with SCI/D was 2.4 times that of 7.7% in non‐SCI/D veterans. However, this rate is falsely elevated due to inability to capture COVID‐19 infections that go undetected if patients are asymptomatic or if mild symptoms are attributed to other common conditions causing fever in the SCI/D population (eg, urinary tract infections). 14
3. PERTINENT PATHOPHYSIOLOGY OF SCI/D
3.1. Aging with SCI/D
Individuals with SCI/D often develop respiratory complications due to age‐related alveolar changes and reductions in vital capacity superimposed on baseline neuromuscular weakness; lung and chest wall compliance changes due to respiratory muscle weakness, spasticity, or hypotonia; obesity; kyphoscoliosis; and sleep‐disordered breathing, including both central and obstructive sleep apnea. These issues increase the baseline risk of acute respiratory failure in persons with SCI/D, particularly those with underlying respiratory or cardiovascular disease, neoplastic conditions, or immune dysfunction. Consequently, respiratory infections such as COVID‐19 may increase morbidity and mortality in the SCI/D population.
3.2. Immune compromise
Individuals with chronic SCI/D are immunocompromised for several reasons: maladaptive sympathetic—neuroendocrine adrenal reflexes, 15 immune suppression with secondary immune deficiency syndrome, 16 obesity‐related inflammation with reduced natural killer cell expression, 17 and increased lung inflammation similar to mild asthma. 18
3.3. Neurogenic respiratory muscle paralysis (restrictive lung defect)
Various degrees of respiratory muscle paralysis are present in most individuals with tetraplegia and many with paraplegia due to inspiratory and expiratory muscle weakness (Table 1). 19 Level and completeness of injury dictate the likelihood of restrictive and obstructive lung dysfunction.
TABLE 1.
Respiratory muscles and SCI/D‐related dysfunction
| Muscle(s) | Innervation | Dysfunction |
|---|---|---|
| Inspiratory musculature | ||
| Diaphragm | C3–C5, phrenic nerve | Inspiratory weakness |
| External intercostals | T1–T11 spinal nerves | |
| Accessory inspiratory muscles | ||
| Scalenes | C4–C6 | Inspiratory weakness |
| Trapezius | Spinal accessory nerve, C4 | |
| Sternocleidomastoid | Spinal accessory nerve, C4 | |
| Expiratory musculature | ||
| Internal intercostals | T1–T11 spinal nerves | Expiratory weakness |
| Transversus abdominus | T6–T11 spinal nerves | Decreased cough force |
| Internal oblique | T6–T11 spinal nerves | |
| External oblique | T6–T11 spinal nerves |
Paralysis of a major portion of the expiratory muscles used to generate an effective cough results from SCI at or above the T6 spinal level. Weakened expiratory muscles lead to decreased peak cough flow, 20 tenacious secretions, and atelectasis. Reduced alveolar expansion decreases surfactant production, increases alveolar surface tension, and markedly increases the work of breathing.
Expiratory muscle paralysis also is associated with outward expansion of the abdominal wall resulting in shortening of the diaphragm, reducing its resting length, diminishing inspired volume, and alveolar expansion. Diaphragm resting length can be easily restored through appropriate use of an elastic abdominal binder, improving breathing efficiency when upright (Figure 1). 21 , 22
FIGURE 1.
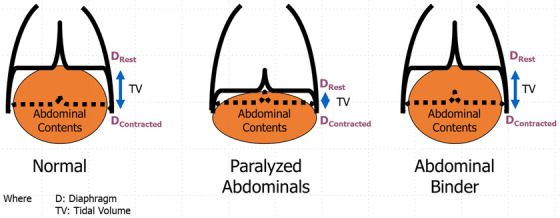
Resting diaphragm length under normal, paralyzed, and abdominal binder conditions
3.4. Neurogenic obstructive lung disease
In individuals with SCI/D above T6, para‐sympathetic predominance leads to bronchiolar constriction, hyper‐reactive airways, and increased mucus secretion. 23
4. DIAGNOSIS
4.1. Confounding conditions in persons with SCI/D
It is important that ED personnel be aware of comorbidities in individuals with SCI/D which may thwart diagnosis of COVID‐19 when they present with potentially infectious complaints. In addition to obvious motor paralysis and sensory loss, persons with SCI/D may have thermoregulatory dysfunction with lower baseline body temperatures and blunted febrile responses, sympathetic blunting, autonomic dysreflexia, neurogenic bowel, neurogenic bladder, spasticity, and pressure injuries. 24
Other conditions can make it difficult to determine the cause of symptoms. For example, poikilothermia—the inability to regulate body temperature—can lead to temperature elevations if the patient is bundled with multiple layers of fabric; and asymptomatic bacteriuria with fever was mistaken for urinary tract infection in a person with SCI/D infected with COVID‐19. 7
ED staff may be unfamiliar with signs such as increased spasticity, urinary incontinence, and autonomic dysreflexia that can be surrogates for pain or infection in persons with SCI/D who may be unable to describe what is happening below their neurological level of injury. 25 See Figure 2 for diagnostic workups and best practices to consider 26 depending on presentation. In addition to pulmonary/critical care specialists and respiratory therapists, consultation with physical medicine and rehabilitation (PM&R) or SCI medicine specialists may be helpful to assist with interpretation of signs and symptoms in the context of SCI/D and formulation of the differential diagnosis and treatment plan.
FIGURE 2.
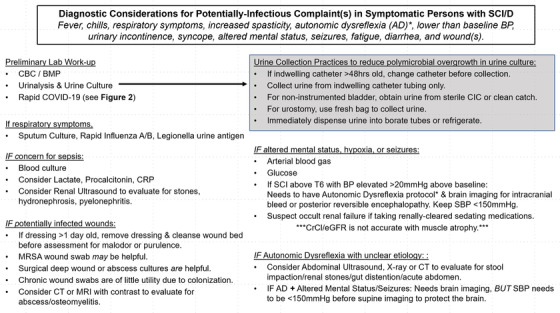
Approach to diagnostic workup for persons with SCI/D. 26 *See Clinical Practice Guideline for details 27
4.2. Exposure risk
Persons with SCI/D who require home care assistance may be exposed to multiple clinical or personal visitors per day. Therefore, it is critical for ED personnel to take special precautions when evaluating this population due to ease of COVID‐19 transmission in the home. Initial suspicion of COVID‐19 infection may be low if the patient has an atypical presentation of COVID‐19 or mild COVID‐19 with concurrent infection such as urinary tract infection. Figure 3 provides a suggested testing algorithm for this patient population.
FIGURE 3.
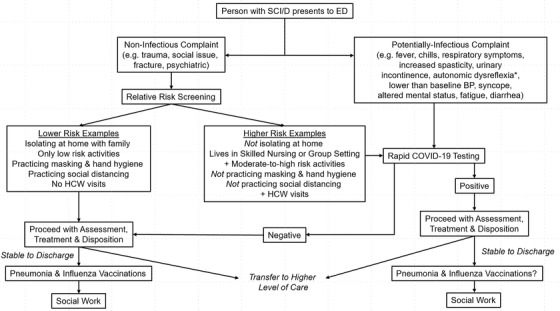
Suggested COVID‐19 testing algorithm for persons with SCI/D presenting to ED. HCW, health care worker
4.3. Presentation of respiratory failure
The typical signs of acute respiratory failure such as dyspnea and tachypnea may not be apparent in individuals with neuromuscular weakness associated with SCI/D. In fact, hypotension, severe hypoxemia, hypercarbia, and altered mental status may be the only presenting signs and symptoms. Therefore, despite a relatively “stable” initial presentation, late‐onset ventilatory failure may develop without a previous ventilator dependence. For this reason, early hospitalization is recommended in the setting of acute respiratory tract infections, especially for those with high tetraplegia, SCI/D for >20 years, or age‐related comorbidities. 2 , 28
4.4. COVID‐19 presentation in SCI/D
Much of the published information on COVID‐19 presentation in persons with SCI/D comes from European SCI specialty and rehabilitation centers. Common presenting symptoms include prolonged fever with varying severity that does not improve with antibiotics, dry cough, fatigue/weakness, dyspnea, increased expectoration, diarrhea, and anosmia. 7 , 8 , 9 , 10 , 11 , 29 An international survey of 783 SCI/D clinicians reported the most common presenting symptom of COVID‐19 in patients with SCI/D was fever (86.2%), followed by shortness of breath (62.1%), body aches/worsening pain (20.7%), sweats (20.7%), and chest pain (13.8%). Cough was not reported in this survey. Atypical presentations reported include increased spasticity (10.3%), rigors (6.9%), or no symptoms (6.9%). 30 Laboratory and radiographic findings have been similar to COVID‐19 in the general population. Multiple articles described COVID‐19 testing and diagnosis being delayed because fever was initially attributed to urinary tract infection or sepsis. 7 , 8 , 10
A prospective case–cohort study of all SCI patients and healthcare workers in an Italian rehabilitation center found that one‐third of infected SCI patients had asymptomatic COVID‐19 infections compared to 11% of the healthcare workers, despite higher age and prevalence of comorbidities. Clinical courses, treatments, and outcomes were also similar with the exception that 60% of SCI patients required supplemental oxygen compared to 30% of healthcare workers. However, the majority of the SCI patients had incomplete injuries in this study and may not be representative of the entire SCI/D population. 9
One asymptomatic individual with new paraplegia, incidentally diagnosed with COVID‐19, developed extensive bilateral lower extremity venous thromboembolism while on chemoprophylaxis and, later, pleuritic chest pain due to pulmonary embolism developed while receiving therapeutic anticoagulation. 11
5. TREATMENT
Many primary care and emergency clinicians are unfamiliar with both the unique physiology associated with SCI/D 31 and the specialized respiratory interventions and techniques to treat individuals with SCI/D. The choice of treatments will depend on the person's neurological level of injury, functional status, and clinical presentation. Persons with SCI/D at or above T6 who present with infectious complaints, regardless of COVID‐19 status, should receive treatments for atelectasis prevention and treatment, because bed rest for illness can worsen baseline lung function. If hypoxemic, oxygen supplementation should be combined with nebulizers and atelectasis treatment. If increased secretions are present, then additional treatments are needed to loosen and mobilize secretions. Those with injuries below T6 may also need cough‐assist due to impairment in expiratory strength and ineffective peak cough flow. Techniques available in the ED may be limited, but ideally would include access to the methods described below (Table 2).
TABLE 2.
Respiratory management in SCI/D
| Simple interventions | Complex interventions |
|---|---|
| Moisten and loosen secretions | |
| Combination bronchodilators | Combination bronchodilators |
| Nebulized normal saline | Nebulized hypertonic saline |
| Flutter valve | Nebulized acetylcysteine |
| Percussion and postural drainage | High frequency chest wall oscillation vest |
| Remove secretions | |
|---|---|
| Airway suctioning with directional catheter | Mechanical insufflation/exsufflation |
| Manually assisted cough (“quad cough”) | Bronchoscopy |
| Decrease atelectasis | |
|---|---|
| Incentive spirometry a and deep breathing | Positive‐expiratory pressure devicesa |
| Abdominal binder (used while seated) | Positive airway pressure systems |
Patients with tetraplegia and limited hand function may need assistance using the devices.
5.1. Hypoxemia management
In general, independent respiration should be maintained as long as possible. Prolonged invasive ventilation can cause deconditioning of already weak respiratory muscles, extended weaning, and/or long‐term ventilatordependency in persons with SCI/D, particularly those with high tetraplegia. Provision of supplemental oxygen (O2) via low flow nasal cannula to achieve appropriate oxygen saturation should be a first‐line intervention in the setting of hypoxia. High‐flow nasal cannula O2 (HFNO2) should be considered next but requires measures to reduce risk of spreading COVID‐19 containing aerosols. Non‐invasive ventilation with face mask may be poorly tolerated if the patient is unable to adjust their mask due to upper limb paralysis. Those who are already ventilatordependent may require an increase in oxygen percentage compared to the usual. Details of when to choose which ventilation modality is outside the scope of this article; however, frailty scores based on physical function measures should not be used in persons with SCI/D or other neurological deficits to judge who qualifies for advanced care. 32
5.2. Atelectasis prevention
Persons with diaphragmatic and intercostal weakness due to SCI/D have reduced inspiratory force and impaired ability to activate incentive spirometry or use deep breathing alone to effectively open alveoli. Taking successive deep breaths without exhaling in between, also known as “breath stacking,” can be helpful in inflating the lungs fully, but typically takes time to learn to perform effectively. These individuals may require positive expiratory pressure devices or positive‐airway pressure (PAP) treatments to prevent or reverse atelectasis, which require systems modifications to ensure safety (see Safety section).
5.3. Secretion management
For individuals with SCI/D and significant airway secretions, aggressive pulmonary management techniques are critical for successful treatment of respiratory infections. Equally important is the early involvement of skilled personnel, including certified/registered respiratory therapists.
Due to preserved vagal innervation of the bronchial tree and parasympathetic predominance, the use of a combined anticholinergic/beta‐2 adrenergic agonist agent (eg, ipratropium bromide and albuterol sulfate), can be effective in reducing bronchial tone, facilitating removal of secretions, and reducing the level of dyspnea. 33 Long‐acting antimuscarinic agents (eg, tiotropium) may also be helpful in the chronic management of these patients.
When persons with SCI/D and respiratory infections present with increased expectoration, nasotracheal suctioning, postural percussion, and drainage (chest physiotherapy), 34 flutter valves, chest wall oscillation vests, and use of mechanical insufflation/exsufflation devices are useful mechanical methods of secretion clearance.
5.3.1. Airway suctioning
Nasotracheal suctioning or tracheal suctioning in individuals with tracheostomies are effective methods of removing upper airway secretions. Directional catheters have the capacity to suction both the right and left main stem bronchi and therefore may be much more effective than the use of standard catheters.
5.3.2. Postural percussion/drainage
Patient positioning and percussion can be an extremely effective method of secretion clearance and should be performed by qualified personnel including respiratory therapists, physical therapists, and/or trained nurses. Specific physician orders are typically needed for these treatments to be implemented. Full prone positioning to improve lung aeration may be difficult to accomplish in person with SCI/D having joint contractures and/or limited cervical range of motion; modified proning may be required.
5.3.3. Mechanical insufflation–exsufflation
The use of a mechanical insufflator/exsufflator device, also known as a “cough‐assist,” 35 has been shown to be extremely useful in patients with SCI/D (Video 1, courtesy of Kessler Foundation) for both removal of secretions and prevention and treatment of atelectasis. Mechanical insufflation–exsufflation was also shown to mobilize a larger volume of secretions than standard chest physiotherapy in adult mechanically ventilated ICU patients. 36 This device delivers a positive pressure breath (+20 to +50 cmH2O), which is then switched to negative pressure (−20 to −50 cmH2O) to clear respiratory secretions. Each change from positive to negative pressure represents a cough cycle; a series of 6–10 cycles provides a full treatment. This technique is minimally invasive, can clear secretions not reachable via tracheal suction, and may reduce the need for bronchoscopy to clear mucus plugging. 28 , 37 Ideally, mechanical insufflation–exsufflation should be combined with one of the manually assisted cough techniques described below to optimize peak cough flow and clearance of secretions during the expiratory phase of the cough cycle. Persons with SCI who are ventilatordependent typically use mechanical insufflation‐exsufflation as part of their regular respiratory treatments and may have their own device. Mechanical insufflation–exsufflation should not be used if there is hemoptysis, pneumothorax, barotrauma, bullous emphysema, nausea, or vomiting.
5.3.4. Manually assisted cough
Another method for secretion clearance is “manual assist” or “quad coughing,” that uses 1‐ or 2‐handed abdominal thrust against a closed glottis, similar to a Heimlich maneuver (Video 2, courtesy of Kessler Foundation). This can also be used in combination with the exsufflation phase of mechanical insufflation–exsufflation. This technique can be effective but is contraindicated in persons who have an inferior vena caval filter (IVCF) in place for pulmonary embolus prophylaxis, as the filter may be dislodged and migrate up or through the inferior vena cava. 38
Hospital‐wide preparations for the care of individuals with SCI/D including obtaining needed equipment in advance and training respiratory and other medical staff on these techniques are necessary to provide optimal management.
6. SAFETY
Although the above‐mentioned respiratory techniques benefit persons with SCI/D with heavy secretions and/or atelectasis, in the setting of a highly transmissible virus, an important concern in emergency care settings is the need for extreme caution during aerosol‐generating procedures including bag valve mask ventilation, oropharyngeal suctioning, endotracheal intubation, nebulizer treatment, positive expiratory pressure treatments, mechanical insufflation‐exsufflation, percussive and postural drainage therapies, HFNO2, CPAP and non‐invasive ventilation, sputum induction, bronchoscopy, and resuscitation involving emergency intubation and/or CPR, among others. Therefore, there is a high risk associated with potential of COVID‐19 aerosol or droplet spread if the individual with SCI/D who is undergoing these procedures is not in isolation and/or the health care providers are not wearing appropriate PPE. 39
Because individuals with SCI/D may require these aerosol generating procedures to adequately recover, rapid transition to a negative‐pressure room, higher level of care, or an isolated area within the emergency facilities where these procedures can be safely performed should be achieved whenever possible. In addition to the use of PPE for airborne protection, medications should be given via metered dose inhalers with spacers and at a higher dose to reach nebulizer equivalence. If nebulizers, HFNO2, and/or non‐invasive ventilation are required, they should be administered in a negative pressure or single room with contact, droplet, and airborne precautions, which should be maintained for at least 30 minutes after completion of an aerosol‐generating procedure. 40 , 41 , 42
Positive expiratory pressure devices should be fitted with an anti‐viral filter. Those with tracheostomies who are not ventilatordependent should wear a heat and moisture exchanger and mask over their nose, mouth, and tracheostomy tube. Tracheostomy tubes should preferentially be cuffed with the cuff inflated during aerosol‐generating procedures. 43 Non‐invasive ventilation set‐ups should be converted to a closed system with a dual lumen circuit with heat and moisture exchanger/viral filter attached to exhaust systems, and a non‐vented full‐face mask or helmet over nasal pillows. Mechanical insufflation–exsufflation can be used with an anti‐viral filter, tubing, and tracheostomy adapter attached to filter protecting the machine. Prolonged negative pressure can be maintained afterward while separating the adaptor or face mask from the patient in order to draw aerosols and droplets into the filter. The circuit tubing and filter can then be removed from the mechanical insufflation–exsufflation device and joined into a circle using the trach adapter to avoid leakage of exsufflated materials before disposal.
7. LOGISTICAL CONCERNS
Many persons with SCI/D have limited mobility and may arrive in a manual or power wheelchair, and with assistive devices and medical equipment that may also be contaminated. Transfers to examination tables will often require the assistance of additional medical personnel or special equipment, such as lifts. Personal protective equipment (PPE) and airborne precautions must be employed, as well as ensuring patient‐handling equipment is sanitized before admission and upon discharge. It should also be noted that these individuals are also at high risk of pressure injuries, venous thromboembolism, and pulmonary embolism at baseline. Some may already be ventilator‐ or non‐invasive ventilation‐dependent. Additional staff may be required to address unique care needs of patients with SCI/D, such as turning and repositioning, management of neurogenic bowel and bladder, feeding, drinking, and respiratory care during their time in an ED. 31
8. DISPOSITION
Even in mild to moderate‐severe cases, due to the high acuity of nursing care required for activities of daily living, neurogenic bowel care, and turning for pressure redistribution, or in the case of pre‐morbid ventilator dependence, the safest location for a person with SCI/D and COVID‐19 may be an intensive care unit or step‐down unit with a higher nurse‐to‐patient ratio than is available on a med‐surg floor. This is particularly true for those who may need specialized air mattresses and frequent turning for pressure injury prevention. Goals of care should be discussed with the patient and family as early as possible to ensure patients' desires are respected particularly as they relate to intubation and code status is appropriate; this may guide disposition.
For those appropriate to discharge home (regardless of COVID‐19 diagnosis), social work should be involved to ensure adequate home care is in place. Medical follow‐up post ED visit should ideally occur via telemedicine with home tele‐monitoring when possible to permit patients to remain isolated. Supplemental O2 and monitoring devices such as oximeters should be supplied when needed. For those who are clinically suitable for and agreeable to vaccination, influenza and pneumonia vaccines should be administered prior to discharge. 44
9. CONCLUSIONS
In summary, the majority of individuals who become infected with COVID‐19 will develop only mild symptoms. However, individuals with SCI/D are at much higher risk of complications of respiratory infections including the more rapid onset of respiratory failure and death due to respiratory muscle paralysis, other chronic respiratory or cardiac conditions, and chronic immune dysfunction. When necessary, aggressive secretion management techniques and a low threshold for transfer to a higher level of care are warranted. The secretion management techniques described above will likely be required for individuals with high thoracic or cervical SCI/D. It cannot be emphasized enough that the proper personnel including PM&R/SCI medicine, pulmonary/critical care physicians, and respiratory therapists be involved early in the care of individuals with SCI/D to provide optimal respiratory care for all respiratory infections to reduce an otherwise high morbidity and mortality.
Supporting information
Supplementary information
Supplementary information
Henzel MK, Shultz JM, Dyson‐Hudson TA, Svircev JN, DiMarco AF, Gater DR. Initial assessment and management of respiratory infections in persons with spinal cord injuries and disorders in the COVID‐19 era. JACEP Open. 2020;1:1404–1412. 10.1002/emp2.12282
Supervising Editor: Henry E. Wang, MD, MS.
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
REFERENCES
- 1. National Spinal Cord Injury Statistical Center , Facts and Figures at a Glance. Birmingham, AL: University of Alabama at Birmingham, 2019. [Google Scholar]
- 2. Soden RJ, Walsh J, Middleton JW, et al. Causes of death after spinal cord injury. Spinal Cord. 2000;38(10):604‐610. [DOI] [PubMed] [Google Scholar]
- 3. DeVivo MJ, Kartus PL, Stover SL, et al. Cause of death for patients with spinal cord injuries. Arch Intern Med. 1989;149(8):1761‐1766. [PubMed] [Google Scholar]
- 4. DiPiro ND, Cao Y, Krause JS. A prospective study of health behaviors and risk of all‐cause and cause‐specific mortality after spinal cord injury. Spinal Cord. 2019;57(11):933‐941. [DOI] [PubMed] [Google Scholar]
- 5. Berlowitz DJ, Wadsworth B, Ross J. Respiratory problems and management in people with spinal cord injury. Breathe. 2016;12(4):329‐340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Johns Hopkins University . COVID‐19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6. Accessed 31 August 2020.
- 7. Righi G, Del Popolo G. COVID‐19 tsunami: the first case of a spinal cord injury patient in Italy. Spinal Cord Ser Cases. 2020;6(1):22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pattanakuhar S, Tangvinit C, Kovindha A. A patient with acute cervical cord injury and COVID‐19: a first case report. Am J Phys Med Rehabil. 2020;99(8):674‐676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. D'Andrea S, Berardicurti O, Berardicurti A, et al. Clinical features and prognosis of COVID‐19 in people with spinal cord injury: a case‐control study. Spinal Cord Ser Cases. 2020;6(1):69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rodríguez‐Cola M, Jiménez‐Velasco I, Gutiérrez‐Henares F, et al. Clinical features of coronavirus disease 2019 (COVID‐19) in a cohort of patients with disability due to spinal cord injury. Spinal Cord Ser Cases. 2020;6(1):39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pisano TJ, Joki J, Hon B, Cuccurullo S. Pulmonary embolism after acute spinal cord injury and COVID‐19: a case report [published online ahead of print August 26, 2020]. Am J Phys Med Rehabil. 2020. 10.1097/PHM.0000000000001578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jutzeler CR, Bourguignon L, Weis CV, et al. Comorbidities, clinical signs and symptoms, laboratory findings, imaging features, treatment strategies, and outcomes in adult and pediatric patients with COVID‐19: a systematic review and meta‐analysis. Travel Med Infect Dis. 2020;37:101825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gater DR Jr, GJ Farkas, Berg AS, Castillo C. Prevalence of metabolic syndrome in veterans with spinal cord injury. J Spinal Cord Med. 2019;42(1):86‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Burns SP, Eberhart AC, Sippel JL, Wilson GM, Evans CT. Case‐fatality with coronavirus disease 2019 (COVID‐19) in United States Veterans with spinal cord injuries and disorders. Spinal Cord. 2020;58(9):1040‐1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Pruss H, Tedeschi A, Thiriot A, et al. Spinal cord injury‐induced immunodeficiency is mediated by a sympathetic‐neuroendocrine adrenal reflex. Nat Neurosci. 2017;20(11):1549‐1559. [DOI] [PubMed] [Google Scholar]
- 16. Riegger T, Conrad S, Schluesener HJ, et al. Immune depression syndrome following human spinal cord injury (SCI): a pilot study. Neuroscience. 2009;158(3):1194‐1199. [DOI] [PubMed] [Google Scholar]
- 17. Herman P, Stein A, Gibbs K, et al. Persons with chronic spinal cord injury have decreased natural killer cell and increased toll‐like receptor/inflammatory gene expression. J Neurotrauma. 2018;35(15):1819‐1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Radulovic M, Bauman WA, Wecht JM, et al. Biomarkers of inflammation in persons with chronic tetraplegia. J Breath Res. 2015;9(3):036001. [DOI] [PubMed] [Google Scholar]
- 19. Chatwin M, Toussaint M, Goncalves MR, et al. Airway clearance techniques in neuromuscular disorders: a state of the art review. Respir Med. 2018;136:98‐110. [DOI] [PubMed] [Google Scholar]
- 20. Park JH, Kang S‐W, Lee SC, et al. How respiratory muscle strength correlates with cough capacity in patients with respiratory muscle weakness. Yonsei Med J. 2010;51(3):392‐397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wadsworth BM, Haines TP, Cornwell PL, et al. Abdominal binder use in people with spinal cord injuries: a systematic review and meta‐analysis. Spinal Cord. 2009;47(4):274‐285. [DOI] [PubMed] [Google Scholar]
- 22. Wadsworth BM, Haines TP, Cornwell PL, et al. Abdominal binder improves lung volumes and voice in people with tetraplegic spinal cord injury. Arch Phys Med Rehabil. 2012;93(12):2189‐2197. [DOI] [PubMed] [Google Scholar]
- 23. Schilero GJ, Bauman WA, Radulovic M. Traumatic spinal cord injury: pulmonary physiologic principles and management. Clin Chest Med. 2018;39(2):411‐425. [DOI] [PubMed] [Google Scholar]
- 24. Gater DR. Neurogenic bowel and bladder evaluation strategies in spinal cord injury: new directions. J Spinal Cord Med. 2020;43(2):139‐140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sánchez‐Raya J, Sampol J. Spinal cord injury and COVID‐19: some thoughts after the first wave. Spinal Cord. 2020;58(8):841‐843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. LaRocco MT, Franek J, Leibach EK, et al. Effectiveness of preanalytic practices on contamination and diagnostic accuracy of urine cultures: a laboratory medicine best practices systematic review and meta‐analysis. Clin Microbiol Rev. 2016;29(1):105‐147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Consortium for Spinal Cord Medicine . Acute management of autonomic dysreflexia: individuals with spinal cord injury presenting to health‐care facilities. 2nd ed. Washington, DC: Paralyzed Veterans of America; 2001. Available at: https://pva-cdnendpoint.azureedge.net/prod/libraries/media/pva/library/publications/cpg_autonomic-dysreflexia.pdf. Accessed August 30, 2020. [Google Scholar]
- 28. Bach JR. Noninvasive respiratory management of patients with neuromuscular disease. Ann Rehabil Med. 2017;41(4):519‐538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gambarrutta‐Malfatti C, López‐Dolado E, Bravo‐Cortés P, et al. (English translation: J Taylor) Respiratory rehabilitation protocol for patients with spinal cord injury and COVID‐19. National Hospital for Paraplegics. Toledo (Spain). Published April 04, 2020. Available at: https://www.iscos.org.uk/uploads/CV-19/updated%20files%204%2024%2020/ENG_SCI_and_COVID_19_Respiratory.pdf. Accessed August 30, 2020.
- 30. Stillman MD, Capron M, Alexander M, Di Giusto ML, Scivoletto G. COVID‐19 and spinal cord injury and disease: results of an international survey. Spinal Cord Ser Cases. 2020;6(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Milligan J, Lee J, Smith M, et al. Advancing primary and community care for persons with spinal cord injury: key findings from a Canadian summit. J Spinal Cord Med. 2020;43(2):223‐233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Palipana D. COVID‐19 and spinal cord injuries: the viewpoint from an emergency department resident with quadriplegia. Emerg Med Australas. 2020;32(4):692‐693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Schilero GJ, Hobson JC, Singh K, et al. Bronchodilator effects of ipratropium bromide and albuterol sulfate among subjects with tetraplegia. J Spinal Cord Med. 2018;41(1):42‐47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Davis K, Johannigman JA, Campbell RS, et al. The acute effects of body position strategies and respiratory therapy in paralyzed patients with acute lung injury. Crit Care. 2001;5(2):81‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Prevost S, Brooks D, Bwititi PT. Mechanical insufflation‐exsufflation: practice patterns among respiratory therapists in Ontario. Can J Respir Ther. 2015;51(2):33‐38. [PMC free article] [PubMed] [Google Scholar]
- 36. Ferreira de Camillis ML, Savi A, Goulart Rosa R, et al. Effects of mechanical insufflation‐exsufflation on airway mucus clearance amount mechanically ventilated ICU subjects. Respir Care. 2018;63(12):1471‐1477. [DOI] [PubMed] [Google Scholar]
- 37. Zakrasek EC, Nielson JL, Kosarchuk JJ, et al. Pulmonary outcomes following specialized respiratory management for acute cervical spinal cord injury: a retrospective analysis. Spinal Cord. 2017;55(6):559‐565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kinney TB, Rose SC, Valji K, et al. Does cervical spinal cord injury induce a higher incidence of complications after prophylactic Greenfield inferior vena cava filter usage. J Vasc Interv Radiol. 1996;7(6):907‐915. [DOI] [PubMed] [Google Scholar]
- 39. Pirzada AR, Aleissi SA, Almeneessier AS, BaHammam AS. Management of aerosol during noninvasive ventilation for patients with sleep‐disordered breathing: important messages during the COVID‐19 pandemic [published online ahead of print June 17, 2020]. Sleep Vigil. 2020:1‐6. 10.1007/s41782-020-00092-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Agency for Clinical Innovation . Aerosol generating respiratory therapies: Nebulizers. Version 1. New South Wales Government; March 23, 2020. Available at: https://www.iscos.org.uk/uploads/CV-19/updated%20files%204%2024%2020/ENG_COVID_19_and_High_Risk_Thera%20-%20Copy%201.pdf. Accessed August 28, 2020.
- 41. Agency for Clinical Innovation . Aerosol generating respiratory therapies: Non‐invasive ventilation (NIV). Version 1. New South Wales Government; March 23, 2020. Available at: https://www.iscos.org.uk/uploads/CV-19/updated%20files%204%2024%2020/ENG_COVID_19_and_High_Risk_Thera.pdf. Accessed August 28, 2020.
- 42. Agency for Clinical Innovation . Aerosol generating respiratory therapies: High flow nasal prong oxygen (HFNPO2). Version 1. New South Wales Government; March 23, 2020. Available at: https://www.iscos.org.uk/uploads/CV-19/updated%20files%204%2024%2020/ENG_COVID_19_and_High_Risk_Thera%20-%20Copy%202.pdf. Accessed August 28, 2020.
- 43. Young EI, Manta D, Sah BP, Brooks BR. Modification of non‐invasive ventilation for the advanced amyotrophic lateral sclerosis patient during the COVID‐19 pandemic ‐ do it now. J Neurol Sci. 2020;414:116893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Evans CT, Weaver FM, Rogers TJ, et al. Guideline‐recommended management of community‐acquired pneumonia in veterans with spinal cord injury. Top Spinal Cord Inj Rehabil. 2012;18(4):300‐305. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary information
Supplementary information


