Abstract
Objectives.
The impact of social distancing on communication and psychosocial variables among individuals with hearing impairment during COVID-19 pandemic. It was our concern that patients who already found themselves socially isolated (Wie, Pripp, & Tvete, 2010) as a result of their hearing loss would be perhaps more susceptible to changes in their communication habits resulting in further social isolation, anxiety and depression. We wanted to better understand how forced social isolation (as part of COVID-19 mitigation) effected a group of individuals with hearing impairment from an auditory ecology and psychosocial perspective. We hypothesized that the listening environments would be different as a result of social isolation when comparing subject’s responses regarding activities and participation prior to COVID-19 and during the COVID-19 pandemic. This change would lead to an increase in experienced and perceived social isolation, anxiety, and depression.
Design.
A total of 48 adults with at least 12 months of cochlear implant experience reported their listening contexts and experiences Pre-COVID and During-COVID using Ecological Momentary Assessment (EMA; methodology collecting a respondent’s self-reports in their natural environments) through a smartphone-based app, and six paper and pencil questionnaires. The Smartphone app and paper-pencil questionnaires address topics related to their listening environment, social isolation, depression, anxiety, lifestyle and demand, loneliness, and satisfaction with amplification. Data from these two time points were compared to better understand the effects of social distancing on the CI recipients’ communication abilities.
Results.
EMA demonstrated that During-COVID CI recipients were more likely to stay home or be outdoors. CI recipients reported that they were less likely to stay indoors outside of their home relative to the Pre-COVID condition. Social distancing also had a significant effect on the overall signal-to-noise ratio (SNR) of the environments indicating that the listening environments had better SNRs. CI recipients also reported better speech understanding, less listening effort, less activity limitation due to hearing loss, less social isolation due to hearing loss, and less anxiety due to hearing loss. Retrospective questionnaires indicated that social distancing had a significant effect the social network size, participant’s personal image of themselves, and overall loneliness.
Conclusions.
Overall, EMA provided us with a glimpse of the effect that forced social isolation has had on the listening environments and psychosocial perspectives of a select number of CI listeners. CI participants in this study reported that they were spending more time at home in a quieter environments During-COVID. Contrary to our hypothesis, CI recipients overall felt less socially isolated and reported less anxiety resulting from their hearing difficulties During-COVID in comparison to Pre-COVID. This, perhaps, implies that having a more controlled environment with fewer speakers provided a more relaxing listening experience.
Introduction
Recommendations from the World Health Organization (WHO) and the Center for Disease Control (CDC) (2020) for slowing the spread of the Novel COVID-19, called SARS-CoV-2, includes social distancing, frequent handwashing, covering your mouth when around others, and cleaning and disinfecting surfaces frequently. People have been requested to shelter-in-place; businesses were forced to close temporarily or permanently; and essential workers found themselves on the frontline of this crisis (Blau, Koebe, & Meyerhofer, 2020). This, as reported by mental health experts, has led to increased anxiety, depression and stress among many individuals (Sarner, 2020) during this pandemic.
As hearing healthcare professionals, the impact of being forced to limit social interactions on individuals with hearing impairment was important for us to understand. We found ourselves postponing cochlear implant (CI) surgeries, evaluations, connections and follow-up care appointments as they were deemed non-urgent patient requests (A. M. Association, 2020). This was concerning as we did not want hearing-related complications to further impact one’s quality of life. Furthermore, it was our concern that patients who already found themselves depressed or socially isolated as a result of their hearing loss (Bigelow et al., 2020; Carlsson et al., 2015; Cosh, Helmer, Delcourt, Robins, & Tully, 2019; Gomaa, Elmagd, Elbadry, & Kader, 2014; Jayakody et al., 2018; Keesom & Hurley, 2020; Wie, Pripp, & Tvete, 2010) would be perhaps more susceptible to the effects of the responsibilities (e.g. staying home, reducing the number of interactions with others, wearing a mask) placed on all individuals during this pandemic. We already understand that the psychosocial aspects of hearing loss are multidimensional and include the emotional, cognitive, interpersonal, behavioral, and physical responses to hearing loss. But we do not have a good understanding about how these psychosocial aspects are entwined and influenced by one’s auditory ecology. Therefore, the goal of this manuscript was to better understand the relationship between these two variables by comparing changes in various aspects of the human condition before and during the pandemic.
As part of a larger study funded at the University of Iowa, we have been studying the impacts of hearing loss and intervention on real-world hearing-related outcomes of function and disability. We have particularly focused our research on understanding domains of activity limitation and participation restrictions, and their effects on quality of life and depression, and how those relate to changes in the listener’s auditory ecology (Gatehouse, Elberling, & Naylor, 1999) for individuals with hearing impairment. Auditory ecology has been described as the range, type, and importance of the listening environments that individuals function (Gatehouse et al., 1999). We have been studying this in listeners with hearing impairment from two perspectives, in situ (in the actual place) through real-world smartphone surveys and through retrospective paper and pencil questionnaires. Both methodologies provide useful information to understand outcomes of function and disability. Retrospective questionnaires, which have historically been widely used to measure subjective outcomes of hearing healthcare, provide the subject’s “believed” perspective of the questionnaire domain as it relies on the subject recalling and summarizing their listening experience based on listening scenarios that the subject might have encountered in the last two-weeks to one-month time period. Contrary, in situ questionnaires using the methodology of Ecological Momentary Assessment (EMA) (Shiffman, Stone, & Hufford, 2008) report on the respondents “experienced” perspective during or right after (i.e., momentary) listening in their natural environments (i.e., ecological) through repeated questionnaires with detailed contextual information to understand the reported environment.
This study sought to better understand the effect that social isolation (as part of COVID-19 mitigation) has had on a group of individuals with hearing impairment from an auditory ecology and psychosocial perspective. Both in situ and retrospective methodologies along with a battery of psychosocial assessments would provide a unique perspective of the complexities involved with social isolation on individuals with hearing impairment. It was our hope that this information would be useful to clinicians and could lead to more insightful questions that clinicians could ask when programming the cochlear implant. Therefore, understanding of the changes to one’s auditory ecology as a result and its influence on psychosocial outcomes have direct consequence to counseling.
Several studies throughout the world have documented levels of anxiety and depression throughout the pandemic (Cao et al., 2020; Hyland et al., 2020; Sarner, 2020; Wang et al., 2020). In fact, it was reported that individuals aged 65 and older had significantly higher levels of COVID-19 related anxiety than adults aged 18-34 (Hyland et al., 2020). Although, the impact of COVID-19 on college-aged students indicated that economic effects, and effects on daily life, as well as delays in academic activities, were positively associated with anxiety symptoms (Cao et al., 2020). The psychological impact of COVID-19 was also evaluated in China on 333 individuals at the initial outbreak of COVID-19 and after epidemic’s peak four weeks later. Through a survey using the Impact of Event Scale-Revised (Christianson & Marren, 2012) and the Depression, Anxiety and Stress Scale-21 (Norton, 2007) scale the respondents initially reported moderate-to-severe stress, anxiety and depression and no significant longitudinal changes in stress, anxiety and depression levels after four weeks (Wang et al., 2020). Unfortunately, this study does not document these levels Pre-COVID and so it is unknown if COVID was the trigger for these levels of stress, depression, and anxiety.
None of the noted studies above reported specifically on individuals who have hearing loss or directly on changes in the respondent’s surroundings. We consider listeners with hearing impairment a vulnerable population given their already reported levels of anxiety and depression often reported with hearing loss (Bigelow et al., 2020; Carlsson et al., 2015; Cosh et al., 2019; Gomaa et al., 2014; Jayakody et al., 2018; Keesom & Hurley, 2020; Wie et al., 2010). As a result, we hypothesized that psychosocial variables including anxiety, depression, and social isolation would be increased during-COVID compared to pre-COVID. We also anticipate that the landscape of the subject’s auditory ecology would also be different when comparing subject’s activity limitation and participant restriction questions prior to COVID-19 and during the COVID-19 pandemic.
Methods
Participants
A total of 48 adults (females = 29), who live in the Midwestern United States, reported their listening contexts and experiences using EMA and paper and pencil questionnaires as part of the larger study prior to the COVID-19 pandemic (referred to as Pre-COVID). All CI recipients were post-lingually deafened and had at least 1 year of CI experience at this test session (mean = 7.41 years and SD = 6.4) and ranged in age from 27 to 78 years (mean = 60, SD = 12.7). Nine recipients had bilateral CIs; six had a unilateral CI and no hearing in the contralateral ear; 16 had a CI and a hearing aid (HA) on opposite ears; and 17 had a combination of a CI and a HA in the same ear with a HA on the contralateral ear. The subject’s unaided low-frequency pure-tone average (125, 250, 500 Hz) in the implanted ear was 70 dB HL (SE: 6.0). The averaged CNC word score in their everyday listening condition closest to their During-COVID test session was 77% (SE: 2.7). These same individuals were invited via a letter to report their listening contexts and experiences again using EMA and paper and pencil questionnaires during implementation of social distancing to slow COVID-19 spread (referred to as During-COVID). Time between the Pre- and During-COVID conditions ranged between 2 months to 20 months (mean = 10.2 months; SD = 4.18). Data from these two time points was compared to better understand the effects of social distancing on the CI recipients’ auditory ecology and psychosocial outcomes.
COVID-19 Guidelines
The earliest a participant started their During-COVID EMA assessment was April 23, 2020 and the latest was May 8, 2020. All surveys were completed by May 15, 2020. The median start date of the surveys was April 26, 2020 and the median end date was May 3, 2020.
A summary of the timeline of restrictions in the State of Iowa began on March 17, 2020, with the Iowa Governor issuing a State of Public Health Disaster Emergency. On April 1, non-essential businesses (e.g. fitness centers, theaters, casinos, senior citizen centers, swimming pools, salons, barbershops) were closed and gatherings of 11 or more people was restricted through the end of April. No “stay-at-home” order was ever issued in Iowa. On May 1, 2020, 77 counties within Iowa where the infected rate had been reduced could reopen restaurants, malls, and retail stores. All places were encouraged to practice social distancing (e.g. 6 ft distance between individuals) and businesses that reopened were required to operate at 50 percent capacity. On May 13, 2020, the Governor announced the reopening of businesses in all 99 counties. The reopening did not include bars, casinos, or movie theatres.
Materials
Ecological Momentary Assessment (EMA)
EMA’s validity and reliability in other disciplines (Hektner, Schmidt, & Csikszentmihalyi, 2007) and in audiology research (Wu, Stangl, Zhang, & Bentler, 2015) has been confirmed. EMA was implemented using an application (app), AudioSense (Hasan, Chipara, Wu, & Aksan, 2014; Hasan, Lai, Chipara, & Wu, 2013), on the CI recipients’ own smartphones (i.e., smartphone based EMA). AudioSense is a two-tier system consisting of smartphones and a backend server. The app is compatible for both iPhones and Android phones and consisted of survey questions focusing on characteristics such as listening environment, sound source, speech understanding, and how their listening difficulties affected their feelings. The entire survey consists of 32 questions that the CI recipients answered. Among them, 17 questions that are more relevant to social distancing are analyzed and reported in this paper. See Table 1 for the survey questions and the associated responses that were analyzed. The questions were developed by some of the authors in this manuscript as part of the larger study at the University of Iowa. The EMA questions were presented adaptively such that certain answers determined whether follow-up questions would be elicited. For example, the Speech Understanding question would be presented only when CI recipients indicated that they were listening to speech in the beginning of the survey. CI recipients tapped the buttons on the app screen to answer the questions. Note that some EMA questions are categorical variables (e.g., “Where were you?”; Indoor at home / Indoors other than home / Car / Outdoors) while others are ordinal variables (e.g., “I could follow the conversation/speech”; Strongly agree / Agree / Neutral / Disagree / Strongly disagree). In the data analysis of the present study, the two example variables just mentioned were referred to as the “Location” variable and the “Speech Understanding” variable, respectively. See square brackets in Table 1 for the names of all variables. Also note, the listener was asked how their hearing loss affected their momentary feelings of depression, social isolation, and anxiety. This is different from the retrospective questionnaires that assess respondents’ depression, loneliness, and anxiety in general (see the Retrospective questionnaires section below).
Table 1.
EMA survey questions used in the present study and their responses. Square brackets show the name of the variable used in analysis. Numbers in parentheses show how the responses are coded in the EMA app.
| Questions | Responses |
|---|---|
| [Active Listening] Were you actively listening most of the time during the previous 5 to 10 minutes? | □ Yes (1) □ No (2) |
| [Location] Where were you? | □ Indoors at home (1) □ Indoors other than home (2) □ Car (3) □ Outdoors (4) |
| [Speech Activity] What kind of speech listening activity were you engaged in? | □ Live conversation with one □ person (1) □ Live conv. With more than one (2) □ Conv. On electronic device (3) □ Speech listening, live (4) □ Speech listening on electronic device (TV, radio, etc.) (5) |
| [Distance] How far away was the sound you were trying to listen to? | □ No distance (e.g., streaming) (1) □ 3 feet or less (2) □ 4 to 10 feet (3) □ More than 10 feet (4) |
| [Signal Type] What kind of sounds were you listening to? (select all that apply) | □ Speech (1) □ Music (2) □ Other (3) |
| [Visual Cues] Could you see the talker’s face? | □ No (1) □ Yes, but only sometimes (2) □ Almost Always (3) |
| [Talker Familiarity] Were you familiar with the talker(s)? | □ Unfamiliar (1) □ Somewhat unfamiliar (2) □ Somewhat familiar (3) □ Familiar (4) |
| [Noisiness] Overall, how loud were the background/environmental sounds? | □ Very loud (1) □ Loud (2) □ Medium (3) □ Soft (4) □ Very soft (5) |
| [Signal-to-Noise Ratio] The speech of interest was ______ when compared to all other sounds. | □ Much louder (1) □ Somewhat louder (2) □ Equally loud (3) □ Somewhat softer (4) □ Much softer (5) |
| [Importance] “In this situation it was important for me to hear well.” | □ Strongly agree (1) □ Agree (2) □ Neutral (3) □ Disagree (4) □ Strongly disagree (5) |
| [Speech Understanding] “I could follow the conversation/speech.” | □ Strongly agree (1) □ Agree (2) □ Neutral (3) □ Disagree (4) □ Strongly disagree (5) |
| [Listening Effort] “I had to strain to listen.” | □ Strongly agree (1) □ Agree (2) □ Neutral (3) □ Disagree (4) □ Strongly disagree (5) |
| [Activity Limitation] “My hearing difficulties limited what I wanted to do or say.” | □ Strongly agree (1) □ Agree (2) □ Neutral (3) □ Disagree (4) □ Strongly disagree (5) |
| [Device Satisfaction] “I was satisfied with my devices in the previous 5 to 10 minutes.” | □ Strongly agree (1) □ Agree (2) □ Neutral (3) □ Disagree (4) □ Strongly disagree (5) |
| [Depression] “My hearing difficulties made me feel sad or depressed.” | □ Strongly agree (1) □ Agree (2) □ Neutral (3) □ Disagree (4) □ Strongly disagree (5) |
| [Social Isolation] “My hearing difficulties made me feel lonely or isolated.” | □ Strongly agree (1) □ Agree (2) □ Neutral (3) □ Disagree (4) □ Strongly disagree (5) |
| [Anxiety] “My hearing difficulties made me feel nervous or anxious.” | □ Strongly agree (1) □ Agree (2) □ Neutral (3) □ Disagree (4) □ Strongly disagree (5) |
The EMA assessments in the Pre- and During-COVID conditions each lasted one week. The EMA app was configured to notify participants to complete surveys (by audio alarm or vibration) approximately every 2 hours during a time-window specified by CI recipients (e.g. 8 am to 8 pm). Once the notification has been delivered, CI recipients had 5 minutes to respond to it. A survey needed to be completed in 7 minutes. CI recipients could ignore any surveys that were inconvenient, or “snooze” the survey if they knew that they would not be able to respond to one during the next 30 minutes. CI recipients were also encouraged to initiate surveys when they had experienced a significant listening event.
Retrospective questionnaires
Six questionnaires were also completed as part of this research study.
Auditory Lifestyle and Demand Questionnaire (ALDQ)
This questionnaire was designed to evaluate the frequency and importance of 24 diverse listening situations on a three-point scale. The ALDQ (Gatehouse et al., 1999) has two scores, one indicating how often an individual encountered different situations (e.g., listening in a background of noise) (referred to as ALDQ-freq) and one indicating the listening demand of those situations (ALDQ-demand). The higher the score, the richer the auditory lifestyle and the higher the listening demand.
Social Network Index (SNI)
The SNI (Cohen, Doyle, Skoner, Rabin, & Gwaltney, 1997) assesses 12 types of social positions/identities held by an individual, including relationships with family members and members of religious groups. An individual is assigned one point for each role (e.g., parent; “How many children do you have?”). The points are summed and range from 0 to 12. This score estimates the diversity of an individual’s social network (SNI-diversity). When an individual holds a given role (e.g., parent), they list the number of people associated with the role (e.g., children) whom they interact with at least once every 2 weeks. The sum of the number of people associated with a role (up to seven, depending on the role; SNI-size) across social roles is used to estimate the size of network and ranges from 0 to 75. Higher numbers indicated more high context social roles and larger social networks.
Satisfaction with Amplification in Daily Life (SADL), Cochlear Implant version
The 15-item SADL measures an individual’s overall satisfaction with their current cochlear implants. The wording “hearing aid” in the original SADL (Cox & Alexander, 1999) was replaced by “cochlear implant.” Four subscales comprise the SADL; Positive Effect (SADL-PE; 6 items), Negative Features (SADL-NF; 3 items), Personal Image (SADL-PI; 3 items) and Service and Cost. A sample question of the SADL-PI is “Do you think people notice your hearing loss more when you wear your cochlear implant(s)?” In the present study, the result of the Service and Cost subscale is not reported because the CI recipients were not billed for audiological services when participating in research the same day as a clinical visit. To answer the SADL items, an individual rates their satisfaction on a 7-point scale. Higher scores indicate more satisfaction on each subscale.
Beck Depression Inventory—II (BDI-II)
The BDI-II (Beck, Steer, & Brown, 1996) is a 21-item scale designed to assess symptoms associated with the diagnosis of depression listed in the Diagnostic and Statistical Manual of Mental Disorders IV (A. P. Association, 2000). An individual answered each item based on how they have been feeling in the past two weeks and their answers to each item are awarded points ranging from 0 to 4. (e.g., “I am no more irritable than usual / I am more irritable than usual / I am much more irritable than usual / I am irritable all the time”). The points of each items are summed for a total score ranging from 0 to 84. Higher scores indicate an increase in depressive symptoms over the past 2 weeks.
UCLA Loneliness Scale Version 3 (UCLA)
The 20-item UCLA (Russell, 1996) self-report inventory assesses feelings of loneliness including items such as companionship and isolation. An individual is instructed to rate how often they feel the described aspects of loneliness on a scale from 1 to 4 (e.g., “How often do you feel in tune with the people around you?”). The total score is the sum of all the items and higher scores indicate more feelings of loneliness.
Beck Anxiety Inventory (BAI)
The BAI (Beck, Brown, Epstein, & Steer, 1988) is a 21-item self-report measure designed to assess the severity of anxiety symptoms in an individual. An individual rates their anxiety-related symptoms (e.g., unable to relax, hands trembling, and scared) on a scale from 0 to 3 during the past week. Higher scores indicate an increase in anxiety-related symptoms over the past week.
Procedures
Prior to each participant’s first EMA assessment (i.e., Pre-COVID), the CI recipients were thoroughly trained in person on completing surveys using the smartphone app. A power-point presentation wherein each question and possible responses were described in detail was shown to each participant by the researcher. All participant questions about the survey were answered and a short 2-sided instruction sheet was sent home with the CI recipients. A researcher downloaded and configured the app on the participants’ personal smartphones. CI recipients then answered questions about their daily listening activities throughout the day for one week using the survey app.
During social distancing (i.e., During-COVID) CI recipients were contacted by the research audiologist though phone or email. The CI recipients were told that the study was looking at what impact social distancing might have on their ability to communicate. The researcher instructed each participant through the app set-up procedures over the phone or sent detailed app set-up instructions via email. Whether the app was set-up independently through the written instructions or with the research audiologist over the phone, the research audiologist checked the settings in the data server to ensure that the app was set-up and communicating with the server correctly. CI recipients then completed one week of EMA surveys in the same manner as their Pre-COVID EMA week. The EMA results were automatically uploaded by the app to a server located at the University of Iowa.
Pre-COVID, the CI recipients filled the six questionnaires out as part of their clinical research visits related to a separate study. During-COVID CI recipients were mailed packets of questionnaires to complete along with a cover letter informing the participants that the researchers were interested in understanding how social distancing associated with COVID-19 affected their overall well-being, including how they hear. The letter also included instructions about filling-out and returning the questionnaires. A stamped, return envelope was included to facilitate return of the questionnaires. Our research team simultaneously contacted the participants and set-up the smartphone survey app to facilitate participation in the EMA portion of the study. CI recipients were paid for their participation in the questionnaires and EMA during both the Pre- and During-COVID assessments.
Statistical Analyses
For EMA, each participant had the opportunity to respond to multiple surveys throughout the week both Pre-COVID and During-COVID. To account for the correlation between these repeated observations per participant we implemented generalized linear mixed models. Each model included a fixed effect for condition (Pre-COVID, During-COVID=reference), a fixed effect to account for participant age, and a random intercept for subject.
When the outcome variable has a dichotomous response (i.e., YES or NO of the Active Listening variable), our mixed model was a mixed effects logistic regression model.
For the categorical variables obtained from single-select questions (i.e., the Location variable, Speech Listening Activity variable, Relative Listening Sound Variable, Relative Background Sound variable, and Distance variable), we analyzed each response option separately by treating them as a binary outcome and then fit a mixed effects logistic regression model to each response option keeping the fixed effect as condition (Pre-COVID, During-COVID=reference). Multiple tests in these situations were also controlled for using a Bonferroni correction at a family-wise alpha level of 0.05.
For the categorical response variable obtained from the multi-select question (i.e., “select all that apply” of the What Sounds Listening to Variable, Who Listening to Variable, and Environmental or Background Sounds Variable), we again analyzed each response option separately by treating them as a binary outcome. We fit a mixed effects logistic regression model to each response option keeping the fixed effect as condition (Pre-COVID, During-COVID=reference). Multiple testing for each question was again controlled for using the Bonferroni correction at a family-wise alpha level of 0.05.
For EMA questions that yielded ordinal outcomes (i.e., Background Sound level Variable, the Signal to Noise Variable, the Speech Understanding variable, the Strain to Listen Variable, the Sound Detection Variable, the Sound Quality Variable, the Satisfaction Variable, the Hearing Limitations Variable, the Hearing Difficulty Depressed Variable, the Hearing Difficulty Isolated Variable, the Hearing Difficulty Anxious Variable, and the Hearing Importance Variable), we used a linear mixed model where the fixed effect in these models was again condition (Pre-COVID, During-COVID=reference).
The CI recipients also completed a retrospective questionnaire both Pre-COVID and During-COVID. For each questionnaire, we performed a linear mixed model to determine the effect of condition keeping the fixed effect as condition (Pre-COVID, During-COVID=reference). For the questionnaires that have multiple subscales, we analyzed each subscale separately.
All analyses were carried out in R v 4.0.2 (Team, 2020) with mixed models performed using the lme4 package (Bates, Machler, Bolker, & Walker, 2015). Degrees of freedom were approximated by the Satterthwaite approximation using the lmerTest package (Kuznetsova, Brockhoff, & Christensen, 2017).
Results
EMA
Across the Pre- and During-COVID conditions, 3075 EMA surveys were completed by the 48 CI recipients (Pre-COVID: n = 1509; During-COVID: n = 1566). Among the 3075 surveys, 41.11% were initiated by the CI recipients (Pre-COVID: 37.08%; During-COVID: 44.34%). Furthermore, of those initiated by the subjects, 72.6% (SD=33%) Pre-COVID and 67.4% (SD=27.1%) During-COVID were initiated in active listening events. This is consistent with the result of Figure 1A. On average each participant completed 31.4 surveys (SD = 10.9, range = 16 to 84, median = 29) and 32.6 surveys (SD = 15.1, range = 5 to 88, median = 30.5) in the Pre- and During-COVID conditions, respectively.
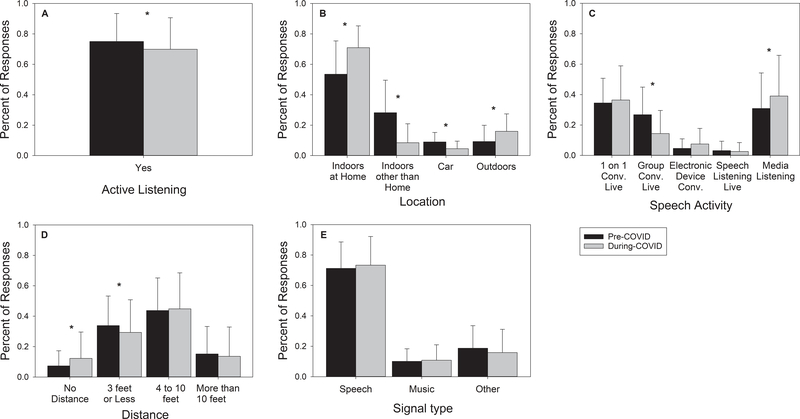
Figure 1.
Mean proportion of times of a response was selected of EMA categorical variables that described listening contexts. Error bars = 1 SD. *: p < 0.05. Conv.: Conversation.
Context: categorical variables
Figure 1 shows the results of the five categorical variables that describe listening context: Active Listening, Location, Speech Activity, and Distance, Signal Type. Note that although the Distance variable looks like an ordinal variable (from “No distance” to “More than 10 feet”), we consider it a categorical variable because “No distance” indicates activity such as using telephone, which is categorically different from face-to-face conversation or watching TV.
The Active Listening variable (Figure 1A) has two response options (i.e., YES or NO). Results from the mixed effects logistic regression model indicate that the CI recipients were less likely to do active listening in the During-COVID condition (b=−0.30, OR=1.35, z=−3.42, p = <.001).
Figures 1B to 1D show the proportion of times of each response of the three variables where only one response option was allowed (Location, Speech Activity, and Distance). The results of the Location variable (Figure 1B), with b representing the mean difference between proportions Pre-COVID versus During-COVID, indicate that During-COVID CI recipients were more likely to stay home (b=−0.89, OR = 0.41, 1/OR = 2.44, z = −10.95, p < .001) and be outdoors (b=−0.62, OR = 0.54, 1/OR = 1.85, z = −5.33, p <.001) while they were less likely to stay indoors outside of their home (indoor other than home: b=1.78, OR = 5.93, z = 14.64, p < .001) and stay in cars (b=0.73, OR = 2.08, z = 4.82, p < .001) relative to the Pre-COVID condition. For the Speech Activity and Distance variables, a mixed effects logistic regression model was fit to each response option because the normality assumption was violated.) During COVID CI recipients were less likely to be engaged in group conversation (Figure 1C, b = 0.81, OR = 2.25, z = 6.30, p = <.001) and were more likely to be engaged in media listening (b = −0.50, OR = 0.61, 1/OR = 1.64, z = −4.36, p = <.001). Closely connected with this, CI recipients also reported being more likely to experience sound that came in the form of streaming (e.g., Zoom) or phone conversations (Figure 1D, b = −0.62, OR = 0.54, 1/OR = 1.85, z = −3.82, p = < .001).
The Signal Type variable (Figure 1E) allowed more than one response (i.e., “select all that apply”, see Table 1). The results from the mixed effects logistic regression model indicated no significant effect on signal type (p = .080 to .502). See Appendix A for detailed statistics.
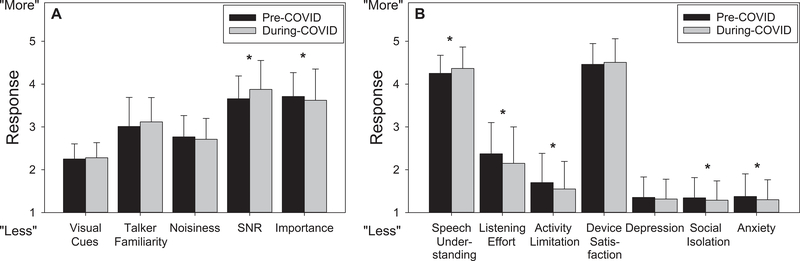
Context: Ordinal variables
Figure 2A shows the five ordinal variables included in this study to describe the listening context: Visual Cues, Talker Familiarity, Noisiness, Signal-to-Noise Ratio (SNR), and Importance. To help data interpretation, in Figure 2A the top of the figure represents “more” (i.e., more visual cues, more talker familiarity, more noise, more/better SNR, and more importance). Therefore, the coded responses of the Noisiness, SNR, and Importance variables (see Table 1) have been reversed in Figure 2A. The results from statistical models indicated a significant effect on the SNR (b=0.22, d = 0.225, t(1717)=5.73, p<.001) and Importance variables (b=−0.09, d = −0.076, t(3036.00)=−2.40, p=.016), such that the listening environments had better SNRs and were less important During-COVID. See Appendix A for detailed statistics.
Figure 2.
Mean scores of EMA categorical variables that describe listening contexts (2A) and EMA ordinal variables that describe outcomes (2B). Top of the figure represents “more” (e.g., more visual cues and more speech understanding). Error bars = 1 SD. *: p < 0.05. SNR: signal-to-noise ratio.
Outcome: Ordinal variables
Figure 2B shows the mean score of seven ordinal variables that describe outcomes: Speech Understanding, Listening Effort, Activity Limitation, Device Satisfaction, Depression, Social Isolation, and Anxiety. Because the top of the figure represents “more” (e.g., more speech understanding, more listening effort, and more anxiety), the coded responses of all variables have been reversed in the figure. The results from linear mixed models indicated that during COVID the CI recipients were more likely to report better speech understanding (b=0.10, d = 0.139, t(1720)=3.38, p = <.001), less listening effort (b=−0.16, d = −0.141, t(2149)=−4.10, p < .001), less activity limitation due to hearing loss (b=−0.15, d = −0.168, t(3032)=−5.89, p < .001), less social isolation due to hearing loss (b=−0.06, d = −0.096, t(3030)=−3.59, p < .001), and less anxiety due to hearing loss (b=−0.08, d = −0.123, t(3030.)=−4.54, p < .001). See Appendix A for detailed statistics.
Retrospective questionnaires
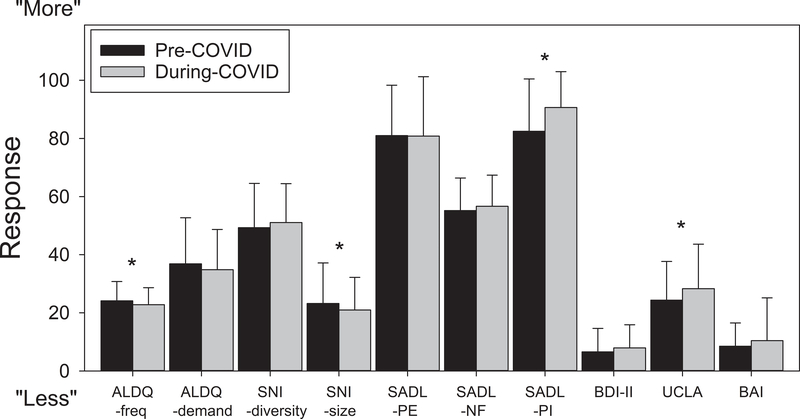
Forty-eight CI recipients completed the six questionnaires in the Pre-COVID and 45 CI recipients completed the six questionnaires in the During-COVID condition: ALDQ, SNI, SADL-CI, BDI-II, UCLA, and BAI (Figure 3). For the three that did not complete During-COVID questionnaires, their Pre-COVID questionnaires were not analyzed. Note that in Figure 3 the top of the figure represents “more” (e.g., larger social network, and more loneliness). Also note that all scores shown in the figure have been linearly transformed so that the score ranges from 0 to 100. The results from the linear mixed models indicate a significant effect on ALDQ-freq (b=1.27, d = 0.201, t(44)=2.04, p = .048), SNI-size (b=2.95, d = 0.246, t(41)=2.24, p = .031), SADL-PI (b=−0.49, d = −0.525, t(44)=−4.13, p = <.001), and UCLA (b=−2.36, d =0.271, t(44)=−2.42, p = .020). Specifically, in the During-COVID condition the CI recipients reported fewer different types of listening environments (ALDQ-freq), fewer people to interact with (SNI-size), more satisfaction with personal image while wearing their devices (SADL-PI), and more loneliness (UCLA) relative to the Pre-COVID condition. See Appendix A for detailed statistics and Appendix B for raw data of retrospective questionnaires between Pre and During-COVID ratings.
Figure 3.
Mean scores of retrospective questionnaires. All scores have been linearly transformed so that the score ranges from 0 to 100. Top of the figure represents “more” (e.g., richer auditory lifestyle and more loneliness). Error bars = 1 SD. *: p < 0.05. ALDQ: Auditory Lifestyle and Demand Questionnaire; SNI: Social Network Index; SADL: Satisfaction with Amplification in Daily Life; PE: Positive Effect subscale of the SADL; NF: Negative Features subscale of the SADL; PI: Personal Image subscale of the SADL; BDI-II: Beck Depression Inventory—II; UCLA: UCLA Loneliness Scale; BAI: Beck Anxiety Inventory.
Discussion
The purpose of this paper was to better understand the influence of one’s auditory ecology on psychosocial well-being. We found ourselves in a unique situation where we could measure the influence of a pandemic on our CI patient’s communication, listening environments, and how those changes might explain differences in psychosocial well-being. We had hypothesized that with the guidelines for flattening the COVID-19 infection rate set forth by the CDC, which included social distancing and stay-at-home orders, would result in increased levels of anxiety, depression, and social isolation. This has also been reported in other studies (Cao et. al, 2020, Wang et. al, 2020; Hyland et. al, 2020), but the respondents in these samples were not hearing impaired. CI recipients completed daily assessments for 1 week using an APP while listening in their natural environments and through retrospective questionnaires. The response rate in this study was lower in comparison to other EMA hearing loss studies (Burke & Naylor, 2020; Galvez et al., 2012; Henry et al., 2012; Timmer, Hickson, & Launer, 2017). Nonetheless, we still feel that our outcomes are a valid representation during this pandemic.
Our results indicate that the CI recipients were staying home or spending more time outdoors During-COVID compared to Pre-COVID (Figure 1B). Additionally, they were spending significantly less time indoors in places other than their homes (Figure 1B). This is consistent with their opinion on the ALDQ where CI recipients felt that their listening experiences were less diverse During-COVID (Figure 3) than Pre-COVID. CI recipients also reported that they were less likely to be actively listening During-COVID (Figure 1A), such as paying direct attention to or providing feedback to a speaker. This perhaps indicates that CI recipients were engaged in more passive listening.
When we assessed whether the type of speech activity CI recipients were engaged in (Figure 1C), listening in live group conversations was significantly less and media listening was significantly higher During-COVID versus Pre-COVID (Figure 1C). This outcome was also corroborated by the fact that listeners reported that they viewed that the listening environments had a more favorable SNR compared to Pre-COVID (Figure 2A).
Psychosocial aspects demonstrated During-COVID that the CI listeners were more likely to report better speech understanding with less effort (Figure 2B). This makes sense as they also reported that they were listening more at home, in a quieter environment with fewer people. Furthermore, when directly asked if their hearing abilities restricted activity that they wanted to participate, they reported that they felt less restricted During-COVID than Pre-COVID. CI recipients also felt that they experienced less social isolation during listening situations (EMA results, Figure 2B) and felt more confident in themselves and as a result reported having a better personal image (Figure 2; SADL-PI). Perhaps these results make sense as to why some listeners with hearing impairment report listening effort, fatigue, and overall avoidance of challenging listening/conversational situations (Pichora-Fuller et al., 2016). By retreating to less noisy environments with fewer people to converse, perhaps these listeners do not feel so out of place or restricted. Contrary, as social network size was reportedly lower During-COVID compared to Pre-COVID (SNI-size, Figure 3), it is reasonable to understand that perhaps the individuals in this study miss being around some of their friends, family, and co-workers, as they reportedly felt lonelier (UCLA, Figure 3) During-COVID compared to Pre-COVID.
When asked about their feelings of anxiety during listening experiences as it directly related to their hearing loss, the CI recipients reported that they felt less anxious During-COVID compared to Pre-COVID (Figure 2B). In contrast, when questioned about their overall anxiety and depression, not directly related to their hearing (Figure 3), CI recipients reported no difference Pre- vs During-COVID. This is opposite of the effect that we had anticipated given the recent uptick on reported anxiety and depression that many individuals are feeling in the current pandemic climate.
A limitation to this study includes having scarce information related to job stability, monetary strains, or health status during or pre-COVID. Probing these factors could have brought more insight into the standardized global assessments of anxiety and depression.
Conclusion
We report an interesting outcome that, while might seem contrary to our original hypothesis, makes sense when putting all the assessment variables together. Having the ability to garner information from a cohort of CI recipients Pre and During-COVID allowed us to have a better understanding of the effects of forced changes in one’s auditory ecology as a result of social isolation might have on some listeners with hearing impairment. Overall, CI recipients in this study were spending more time at home in a quieter environment and as a result felt less socially isolated and with reduced anxiety During-COVID in comparison to Pre-COVID. Our results demonstrate that perhaps when our listeners with a CI can surround themselves with a more predictable listening environment (e.g.at home with fewer people) they feel more included in the conversations around them resulting in less feeling of anxiety and social isolation.
Supplementary Material
Acknowledgement:
This research was supported in part by research grant 2P50DC000242 from the National Institutes on Deafness and Other Communication Disorders, National Institutes of Health; the Lions Clubs International Foundation; the Iowa Lions Foundation. All authors contributed equally to this work. C.D., Y.H.W., and E.S. wrote the main paper, O.C. and Y.H.W. created the EMA app; J.O. and M.S. provided statistical analysis. Y.H.W. provided the Supplementary Digital Content. All authors discussed the results and implications and commented on the manuscript at all stages.
Footnotes
Disclosures/conflicts of interest: Camille Dunn serves on the advisory board for Med-EL and Earlens Corporation; consultant for Advanced Bionics, Cochlear Americas and iotaMotion; received grant funding from Med-EL Corp and Advanced Bionics.
References
- Association, American Medical. (2020, May 21, 2020). Helping private practices navigate non-essential care during COVID-19. Retrieved from https://www.ama-assn.org/delivering-care/public-health/helping-private-practices-navigate-non-essential-care-during-covid-19
- Association, American Psychiatric. (2000). Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition Text Revision ed.). Washington D.C.: Amerian Psychiatric Press. [Google Scholar]
- Bates D, Machler M, Bolker BM, & Walker SC (2015). Fitting Linear Mixed-Effects Models Using lme4. Journal of Statistical Software, 67(1), 1–48. doi:DOI 10.18637/jss.v067.i01 [DOI] [Google Scholar]
- Beck AT, Brown G, Epstein N, & Steer RA. (1988). An Inventory for Measuring Clinical Anxiety - Psychometric Properties. Journal of consulting and clinical psychology, 56(6), 893–897. doi:Doi 10.1037/0022-006x.56.6.893 [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown GK. (1996). Manual for the Beck Depression Inventory–II. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Bigelow RT, Reed NS, Brewster KK, Huang A, Rebok G, Rutherford BR, & Lin FR (2020). Association of Hearing Loss With Psychological Distress and Utilization of Mental Health Services Among Adults in the United States. JAMA Netw Open, 3(7), e2010986. doi: 10.1001/jamanetworkopen.2020.10986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blau Francine D., Koebe Josefine, & Meyerhofer Pamela A. (2020, April 30, 2020). Essential and Frontline Workers in the COVID-19 Crisis. Retrieved from https://econofact.org/essential-and-frontline-workers-in-the-covid-19-crisis [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke LA, & Naylor G (2020). Daily-Life Fatigue in Mild to Moderate Hearing Impairment: An Ecological Momentary Assessment Study. Ear Hear. doi: 10.1097/aud.0000000000000888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, & Zheng J (2020). The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry research, 287, 112934. doi: 10.1016/j.psychres.2020.112934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlsson PI, Hjaldahl J, Magnuson A, Ternevall E, Eden M, Skagerstrand A, & Jonsson R (2015). Severe to profound hearing impairment: quality of life, psychosocial consequences and audiological rehabilitation. Disability and rehabilitation, 37(20), 1849–1856. doi: 10.3109/09638288.2014.982833 [DOI] [PubMed] [Google Scholar]
- CDC, Centers for Disease Control and Prevention. (2020, June 24, 2020). Coronavirus Disease 2019 (COVID-19). Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/your-health/index.html
- Christianson S, & Marren J (2012). The Impact of Event Scale - Revised (IES-R). Medsurg nursing : official journal of the Academy of Medical-Surgical Nurses, 21(5), 321–322. [PubMed] [Google Scholar]
- Cohen S, Doyle WJ, Skoner DP, Rabin BS, & Gwaltney JM Jr. (1997). Social ties and susceptibility to the common cold. JAMA, 277(24), 1940–1944. [PubMed] [Google Scholar]
- Cosh S, Helmer C, Delcourt C, Robins TG, & Tully PJ (2019). Depression in elderly patients with hearing loss: current perspectives. Clin Interv Aging, 14, 1471–1480. doi: 10.2147/CIA.S195824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox RM, & Alexander GC (1999). Measuring Satisfaction with Amplification in Daily Life: the SADL scale. Ear Hear, 20(4), 306–320. [DOI] [PubMed] [Google Scholar]
- Galvez G, Turbin MB, Thielman EJ, Istvan JA, Andrews JA, & Henry JA (2012). Feasibility of ecological momentary assessment of hearing difficulties encountered by hearing aid users. Ear Hear, 33(4), 497–507. doi: 10.1097/AUD.0b013e3182498c41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gatehouse S, Elberling C, & Naylor G. (1999). Aspects of auditory ecology and psychoacoustic function as determinants of benefits from and candidature for non-linear processing in hearing aids In Rasmussen AN, Osterhammel PA, Andersen T, & Poulsen T (Eds.), Auditory Models and Non-Linear Hearing Instruments (pp. 221–233). Denmark: The Danavox Jubilee Foundation. [Google Scholar]
- Gomaa MA, Elmagd MH, Elbadry MM, & Kader RM (2014). Depression, Anxiety and Stress Scale in patients with tinnitus and hearing loss. Eur Arch Otorhinolaryngol, 271(8), 2177–2184. doi: 10.1007/s00405-013-2715-6 [DOI] [PubMed] [Google Scholar]
- Hasan SS, Chipara O, Wu YH, & Aksan N (2014). Evaluating auditory contexts and their impacts on hearing aid outcomes with mobile phones. Paper presented at the 8th International Conference on Pervasive Computing Technologies for Healthcare, Oldenburg, Germany. [Google Scholar]
- Hasan SS, Lai F, Chipara O, & Wu YH. (2013). AudioSense: Enabling real-time evaluation of hearing aid technology in-situ. Paper presented at the 26th IEEE International Symposium on Computer-Based Medical Systems, Porto, Portugal. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hektner JM, Schmidt JA, & Csikszentmihalyi M (2007). Experience sampling method: Measuring the quality of everyday life: Sage. [Google Scholar]
- Henry JA, Galvez G, Turbin MB, Thielman EJ, McMillan GP, & Istvan JA (2012). Pilot study to evaluate ecological momentary assessment of tinnitus. Ear Hear, 33(2), 179–290. doi: 10.1097/AUD.0b013e31822f6740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland P, Shevlin M, McBride O, Murphy J, Karatzias T, Bentall RP, … Vallieres F (2020). Anxiety and depression in the Republic of Ireland during the COVID-19 pandemic. Acta psychiatrica Scandinavica. doi: 10.1111/acps.13219 [DOI] [PubMed] [Google Scholar]
- Jayakody DMP, Almeida OP, Speelman CP, Bennett RJ, Moyle TC, Yiannos JM, & Friedland PL (2018). Association between speech and high-frequency hearing loss and depression, anxiety and stress in older adults. Maturitas, 110, 86–91. doi: 10.1016/j.maturitas.2018.02.002 [DOI] [PubMed] [Google Scholar]
- Keesom SM, & Hurley LM (2020). Silence, Solitude, and Serotonin: Neural Mechanisms Linking Hearing Loss and Social Isolation. Brain Sci, 10(6). doi: 10.3390/brainsci10060367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuznetsova A, Brockhoff PB, & Christensen RHB (2017). lmerTest Package: Tests in Linear Mixed Effects Models. Journal of Statistical Software, 82(13), 1–26. doi:DOI 10.18637/jss.v082.i13 [DOI] [Google Scholar]
- Norton Peter J. (2007). Depression Anxiety and Stress Scales (DASS-21): Psychometric analysis across four racial groups. Anxiety, Stress, & Coping, 20(3), 253–265. doi: 10.1080/10615800701309279 [DOI] [PubMed] [Google Scholar]
- Pichora-Fuller MK, Kramer SE, Eckert MA, Edwards B, Hornsby BW, Humes LE, … Wingfield A (2016). Hearing Impairment and Cognitive Energy: The Framework for Understanding Effortful Listening (FUEL). Ear Hear, 37 Suppl 1, 5S–27S. doi: 10.1097/AUD.0000000000000312 [DOI] [PubMed] [Google Scholar]
- Russell DW (1996). UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. Journal of personality assessment, 66(1), 20–40. doi:DOI 10.1207/s15327752jpa6601_2 [DOI] [PubMed] [Google Scholar]
- Sarner Moya. (2020). Maintiaining Mental health in the Time of Coronavirus. New Scientist, 41–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, & Hufford MR (2008). Ecological momentary assessment. Annu Rev Clin Psychol, 4, 1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415 [DOI] [PubMed] [Google Scholar]
- Team, R Core. (2020). R: A language and environment for statistical computing. Retrieved from URL https://www.R-project.org/
- Timmer BHB, Hickson L, & Launer S (2017). Ecological Momentary Assessment: Feasibility, Construct Validity, and Future Applications. Am J Audiol, 26(3s), 436–442. doi: 10.1044/2017_aja-16-0126 [DOI] [PubMed] [Google Scholar]
- Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, … Ho C (2020). A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun, 87, 40–48. doi: 10.1016/j.bbi.2020.04.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wie OB, Pripp AH, & Tvete O (2010). Unilateral deafness in adults: effects on communication and social interaction. Ann Otol Rhinol Laryngol, 119(11), 772–781. [PubMed] [Google Scholar]
- Wu YH, Stangl E, Zhang X, & Bentler RA (2015). Construct Validity of the Ecological Momentary Assessment in Audiology Research. J Am Acad Audiol, 26(10), 872–884. doi: 10.3766/jaaa.15034 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.