Central Illustration: Quality Metrics in Pediatric/Congenital Catheterization.
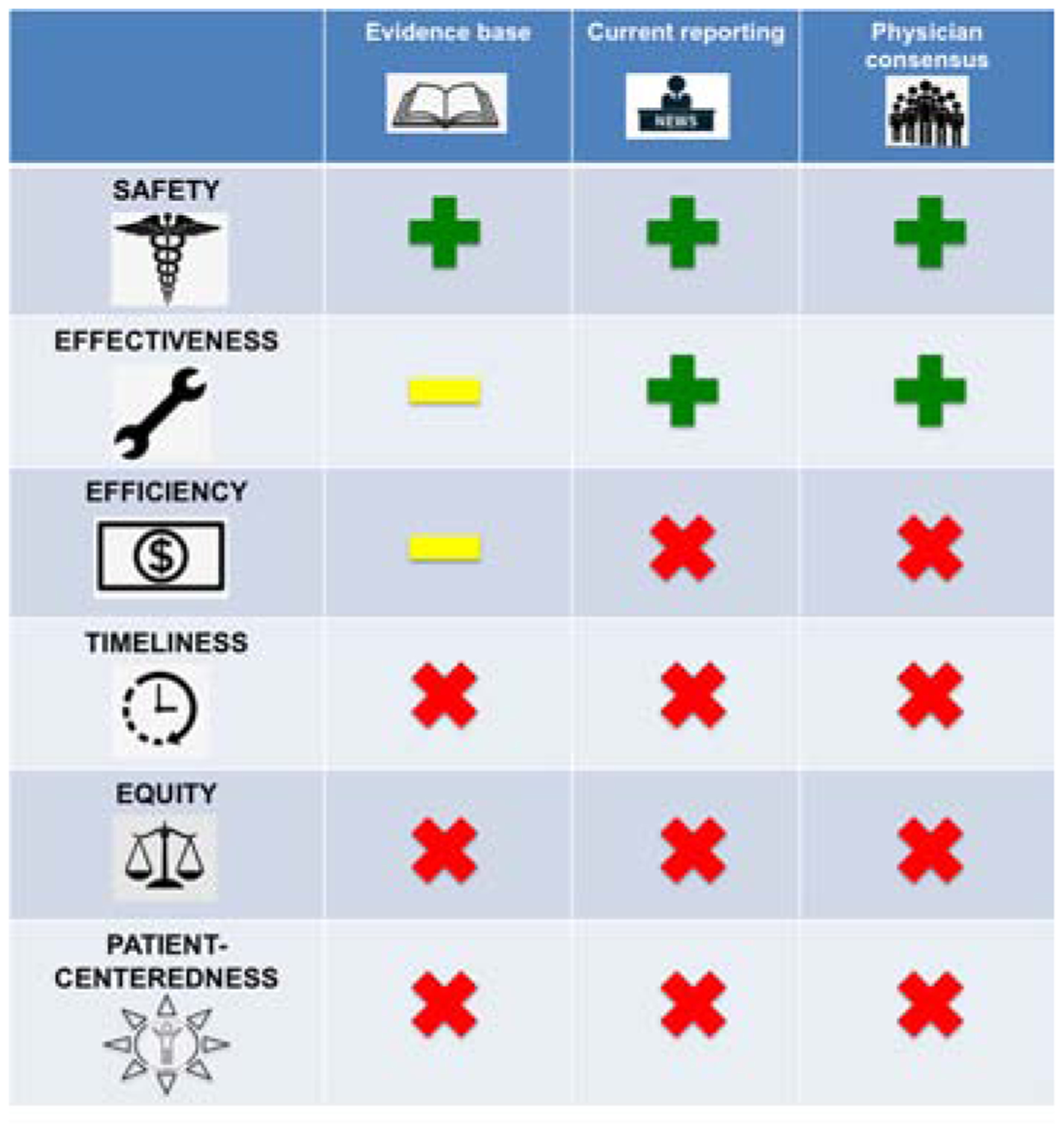
Results from systematic review of the medical literature, review of organizations reporting quality, and a survey of US pediatric/congenital interventional cardiologists are presented. Quality metrics are divided into the six domains (rows) identified by the US Institute of Medicine. The scientific literature about quality metrics is focused almost entirely on safety metrics. Pooled adverse events (AE) and failure to rescue have been studied, but further research is necessary to determine the optimal measure of safety. IMPACT®, CCISC, and C3PO registries report raw and risk adjusted AE to members. Survey data demonstrates high-levels of interest in safety metrics with particular interest in procedure-specific AE as a possible metric. At the same time confidence in current risk-adjustment models is low. For effectiveness, technical success has been reported for individual procedures, but their use as quality metrics has not been evaluated. Development of risk adjustment models specifically for each procedure-specific metric of technical success is necessary. IMPACT® reports measures of technical success for a subset of procedures, and survey data demonstrate that there is interest in procedure-specific technical success as a metric for procedural success. In terms of efficiency, economic cost of procedures has been studied as an outcome, with large magnitude variation demonstrated between centers. However, it has not been evaluated as a quality metric. Metrics combining efficacy and cost (i.e. value) are more complete measures of efficiency but have not been studied. There remain significant knowledge gaps and lack of consensus about measures of timeliness, equity, and patient-centeredness. These can only be addressed by additional research.
