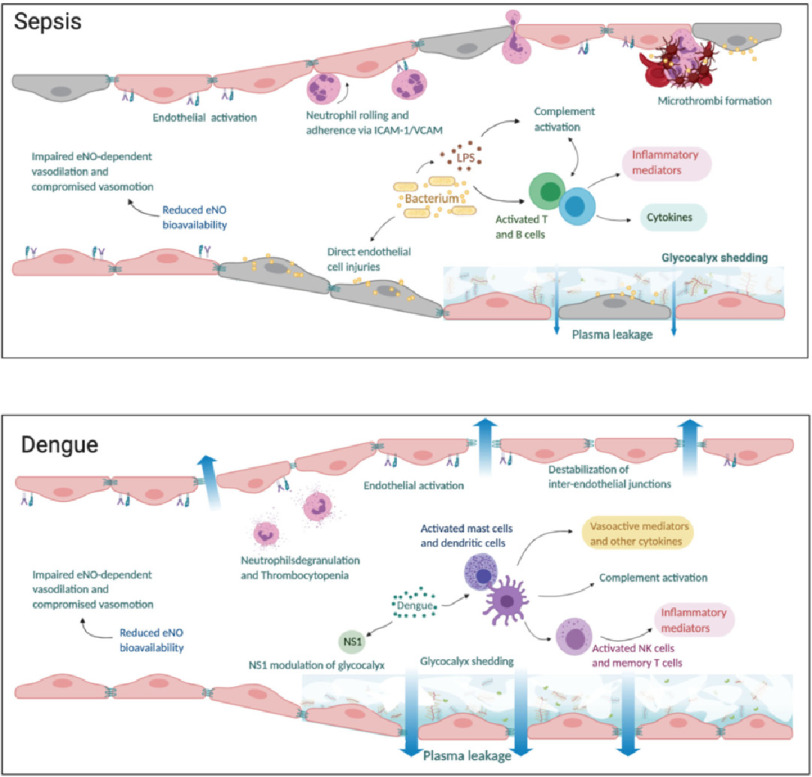
Figure 2. The microcirculation appearance in (a) sepsis and (b) dengue.
In sepsis, there is inflammation and direct injury of endothelial cells by bacterial proteins and toxins. Endothelial activation leads to neutrophil chemotaxis and adherence to intercellular adhesion molecule- 1 (ICAM-1) and vascular adhesion molecule (VCAM) expressed on endothelial cells. Concurrently, there is activation of complement, T and B immune cells leading to release of inflammatory mediators and cytokines which cause further inflammation and glycocalyx damage. Concurrently, the coagulation cascade is activated, and anticoagulant/fibrinolysis pathways are impaired leading to formation of microthrombi and compromised microvascular flow. In dengue, viral non-structural 1 (NS1) protein triggers hyperpermeability and directly alters the endothelial layer function through the activation of several enzymes responsible for glycocalyx degradation. Activation of immune cells leads to complement activation and release of inflammatory mediators. There is impaired endothelial nitric oxide (eNO) dependent vasodilation due to reduced eNO bioavailability leading to compromised microvascular flow. Plasma leakage in both sepsis and dengue occur as a result of glycocalyx shedding and disruption of tight and adherens junctions between endothelial cells.