Abstract
Knowledge transfer is recognized as a vital stage in evidence-informed nursing with several models available to guide the process. Although the main components commonly involve identification of messages, stakeholders, processes and contexts, the underpinning models remain largely unrefined and untested; and they need to be evaluated. We set out to explore the use of our “Evidence-based Model for Transfer & Exchange of Research Knowledge” (EMTReK) within palliative care research. Between January 2016 and May 2017, data were collected from five case studies which used the EMTReK model as a means to transfer knowledge relating to palliative care research, undertaken in Ireland. A qualitative approach was taken with thematic analysis of case documentation, semistructured interviews, and field notes from the case studies. Qualitative analysis supports the core components of EMTReK as a model of knowledge transfer and exchange in palliative care. Results focused upon identification of messages to be transferred to defined stakeholders through interactive processes that take account of context. Case study findings show how the model was interpreted and operationalized by participants and demonstrate its impact on knowledge transfer and exchange. Eight themes were drawn from the data: Credibility of the Model, Model Accessibility, Applicability to Palliative Care, A Matter of Timing, Positive Role of Facilitation, Required Resources, Enhancing Research Quality, Limitations or Areas for Further Consideration. Study participants found EMTReK to be a useful guide when making knowledge transfer plans. Success depended upon adequate facilitation and guidance. Further exploration of the model's utility is warranted.
Keywords: evaluation studies, knowledge transfer, knowledge exchange, stakeholder, communication
Background
One of the most common challenges of health research today is the optimal integration of new findings into routine practice (Ward, Grimshaw, & Eccles, 2013). Such integration assumes effective knowledge transfer and exchange (KTE) as a prerequisite to successful implementation. This is recognized as particularly difficult in complex clinical areas such as palliative care, where study findings from a wide range of research areas have implications across a wide range of service areas, professions, and disease states. These findings are disseminated in a range of publications without sensitive methods for effective retrieval (Tieman, Sladek, & Currow, 2009). An in-depth scoping review of KTE frameworks used in health, and analysis of the core concepts of these frameworks was undertaken (Prihodova, Guerin, Tunney, & Kernohan, 2019), over 60 different models with components relevant to health-care KTE were identified, yet most were focused on the broader issue of implementation, with specific aspects of KTE poorly defined and inadequately tested. In particular, elements of the practice and policy context were not very clear, with little to help separate and address these two influences. This led to the development of the Evidence-based Model for the Transfer & Exchange of Research Knowledge (EMTReK) and a subsequent exploration of barriers and facilitators to KTE within palliative care, undertaken with researchers (n = 9) completing funded research in palliative care (Kernohan, Brown, Payne, & Guerin, 2018).
EMTReK works by highlighting the six primary components of knowledge transfer: the message; various stakeholders; multiple processes; the local context; the wider social, cultural and economic context; and evaluation of the model. We recommend model users start by giving thought to the primary message (five subcomponents provide the optimal characteristics). Then, they should identify the stakeholder groups: researchers (knowledge producers), clinicians (knowledge users), and patients and the wider public (knowledge beneficiaries). Then, optimal processes (and six associated subcomponents) to convey the messages should be considered. The model requires the user to carefully consider two contextual layers. Its circular pattern incites rehearsal of all parts for mutual best fit. The model includes an evaluation component to encourage quality improvement in its use.
This article reports on the further exploration of the EMTReK model within palliative care settings. The objective was to explore and evaluate the process of using an evidence-based model in developing KTE plans, including identification of any barriers or enablers to the use of EMTReK.
Methods
We undertook an exploratory qualitative enquiry using case studies with lead researchers in palliative care (principle investigators [PIs]). Drawing on the modeling process and outcomes component of the Medical Research Council Guidance for Developing and Evaluating Complex Health Interventions (Craig et al., 2008), data were collected reflecting multiple perspectives arising from cases studies utilizing the EMTReK model. Appropriate ethical approvals were obtained.
Potential case studies were identified from palliative care research activity conducted within Ireland. Between January 2016 and May 2017, data were collected from four research projects. These case studies were chosen based on predetermined selection criteria, which ensured variety with regard to target audience, context, and knowledge available to provide a wide range of data for exploring EMTReK. These criteria were as follows:
Readily available evidence to be transferred from the case study to target audiences;
Willingness of the case PI to use the EMTReK model in the development or adaptation of their knowledge transfer plans; and
Feasibility of applying EMTReK within the time and resources of this project.
Only a limited number of research projects were available: All those who met the criteria were included. Written consent was obtained from each participant. In addition, the research team used EMTReK in planning their own dissemination of the model to the community of researchers from which the case studies were drawn. The research team then reflected on this process through interviews. The dissemination development of the EMTReK model itself was determined to be a valuable case study, as it provided an insight into the use of the model as a means to transfer knowledge to researchers as a primary user group of research findings. Thus, this article considers the experience from five Case Studies (CS1–CS5). The intention was that the range of cases allowed for testing of all the dimensions and assumptions of the KTE model, with the exception of evaluation, which was undertaken by the EMTRek team. The research knowledge to be disseminated from each case study was identified in the context of the focus of the respective research studies:
CS1: Development and implementation of a KTE model suitable for use within palliative care
CS2: Launch of national palliative care guidelines for Parkinson's disease in the Republic of Ireland
CS3: Results from a survey of General Practitioners on palliative care provision for patients with existing mental illness across the island of Ireland
CS4: Exploration of the role of palliative rehabilitation within advanced lung cancer management
CS5: Findings from an online survey of lay experience of palliative care across the island of Ireland.
For each of the case studies, PIs developed and revised knowledge transfer plans based on the six core components of the EMTReK model (Table 1).
Table 1.
The Six Components of the EMTReK Model That Are Necessary to Ensure Effective KTE.
| Component | Description and subcomponents |
|---|---|
| Social, cultural, and economic context | The impact and influence that wider social, cultural, and economic factors in the research and practice environment |
| The message | The relevance, usability, and quality of the knowledge to be transferred. – Knowledge meets a user need; – Knowledge is accessible; – Multiple types of knowledge are valid; – Knowledge is credible; – Knowledge is actionable |
| The process | Identify appropriate processes or strategies to implement the transfer. This is a “push–pull” process influenced by both the researcher's actions and the needs of other stakeholders. – Interactive exchange; – Skilled facilitation; – Opinion leaders/champions; – Marketing knowledge; – Diverse activities; – Targeted, timely activities |
| The stakeholders | Identify appropriate stakeholders (either and both sides of the exchange process) to be involved in the transfer activities. – Involves multiple stakeholders; – Knowledge partners; – Knowledge users; – Knowledge beneficiaries |
| The local context | Consider the impact and influence that relevant local settings in which the transfer will occur can have on the process. Can include organizational settings. – Organizational influence; – Organizational culture; – Readiness is key; – Resourcing KTE |
| Efficacy/outcomes | KTE must include a mechanism for evaluation of the success of the process |
Note. KTE = knowledge transfer and exchange.
This process was facilitated by members of the EMTReK study team who have a wide and varied expertise of palliative care and health-care research and practice. A nominal fund was available to support outputs arising from the activities planned. As part of this process, one-to-one semistructured discussions took place, which were audio recorded, each taking up to one hour to complete. KTE plans were scrutinized to ensure feasibility and appropriateness in relation to the EMTReK model and resources available, for example, time/cost/acceptability. Following the interview, participants were asked to provide a one-page summary of their KTE plans, giving examples of how they had considered the key components of EMTReK and providing a brief timeline of activities. To evaluate the process and experience, three approaches to data collection were carried out across the case studies.
Case Documentation: Each PI from the five case studies completed a one-page KTE plan explaining how they planned to use EMTReK for knowledge transfer. This was subsequently mapped to a matrix of key components of the EMTReK model. In addition, PIs were asked to record details of KTE activities, as they occurred, through an online activity log. This logged dates and times, factors that supported KTE, barriers/challenges encountered, the role of EMTReK in informing KTE, and any other comments. Despite regular encouragement, this process was only actioned by two PIs with a total of three online entries submitted.
- Interviews With Case Study PIs: At the end of the specified knowledge transfer process, PIs (n = 6, one case study was led by two co-PIs) were invited to participate in a final semistructured interview, lasting up to 80 minutes, on their experiences of using the EMTReK model. The semistructured interviews, which were digitally recorded and transcribed, were guided by a topic guide that focused on pros and cons of the model and included:
- reasons for participating in the EMTReK study (by way of introduction),
- the extent to which the EMTReK approach to KTE was new or familiar,
- the role of facilitation and funding*
- timing of model use*
- value of components and overall design of the model
- benefits/burdens of using EMTReK
- future use of EMTReK (by way of closure).
Attendance at KTE Events: In all cases, knowledge transfer activities included organized events. Multidisciplinary audiences included doctors, nurses, allied health professionals, psychologists, health economists, academics, researchers, representatives from patient and public involvement groups, and funding bodies. Where possible, members of the EMTReK project team attended and observed these events and field notes were taken (n = 3). In addition, for Case Study 1, data were collected through notes compiled by an independent stenographer and through the collection of group and individual worksheets.
Data Analysis
Thematic analysis was undertaken on all the data collected across the case studies, including transcribed workshop feedback, case documentation, interview transcripts, and field notes. A pragmatic approach to qualitative analysis was undertaken using the stages outlined by Braun and Clarke (2006) as follows:
Immersion in the data, reflecting on the study objective
Generation on initial codes
Searching for evidence of themes
Reviewing themes across cases
Defining and naming themes
Producing the report
Although we sought support for a highly structured model for KTE, we adopted an open inductive coding strategy, to elicit an understanding of how the model was used in practice.
A qualitative package (QSR International's NVivo 10 software) was used to organize and analyze the data. The weighting of the analysis was toward the interviews; however, the credibility of the themes was tested by ensuring that the themes resonated with the data arising from the other data sources. Study design was devised by two experienced researchers, in partnership (W. G. K., S. G.); as was data collection, which included interview data, documentation about each research project and field notes (by M. J. B., C. P.). Initial data analyses were shared (between C. P. and S. G.) and were contextualized in the style of case conference. In this way, findings were discussed at research meetings, verified, and confirmed by all authors.
Findings
The eight main themes, which arose during analysis of the interview data, corroborated by documentary evidence and researcher observations, were as follows: Credibility of the Model, Model Accessibility, Applicability to Palliative Care, A Matter of Timing, Positive Role of Facilitation, Resources for KTE, Enhancing Research Quality, Limitations, or Areas for Further Consideration.
Theme 1 —
Credibility of the Model was assured by the iterative development process of systematic review and stakeholder feedback that was undertaken.
Comprehensive systematic review, a rigorous analysis of the data with credibility checks built in … I think we have a right to be confident in the product but that obviously there will constantly be lessons to be learned about it as a product as it gets used. (CS1 PI1)
In addition, the credibility of the model was further tested through the use of the model by the EMTReK development team to disseminate the findings from the development and testing of the model itself.
Theme 2 —
Model Accessibility captured the idea of reaching out to users. EMTReK was determined to be simple and therefore accessible to a wide range of potential users, including clinicians with little prior research experience or training in KTE.
To me it did represent what we know influences knowledge exchange well. (CS2)
Participants commented on the value of EMTReK as a way of maintaining a focus on KTE throughout the research process.
The model has been very useful in helping us as an organization to think through the process of disseminating this information. It has also been a driver in keeping a sustained ongoing effort to disseminate the information … to make this valuable resource come alive. (CS5)
[the model] made me really think about who do I need to influence more. And because I have worked with the same collaborator for a long time who thinks in a clinical way, and I think in a research way, it helped me to bring us together to influence more strategically, rather than more academically. (CS4)
All of the individual component parts of the model were perceived to have value in shaping better KTE practices.
Theme 3 —
Applicability to Palliative Care was drawn from the general agreement that while the model had been developed based on the systematic review and synthesis of wider health sciences research, the model was applicable within palliative care research settings.
I can't think of another scenario where you'd say oh no that just would not apply, wouldn't fit, or some of the language would be wrong. (CS2)
Some also commented that the holistic nature of palliative care made for easier adoption of the principles of KTE using the model:
the multidisciplinary nature of what palliative care is about … there's an awareness of researchers coming from different disciplines and talking different ways and having different standards. (CS1 PI1)
Respondents mentioned the particular ethics and governance issues that could occur when KTE related to difficult or emotive messages.
you certainly don't want to feel as if you're lying to people … and yet people are not ready to hear everything maybe at the same time … It's a more complex, more emotive message … something that you wouldn't have in other things that are very straightforward. (CS2)
Theme 4 —
A Matter of Timing of the use of the model for KTE was seen as an important consideration.
The easier solution, the line of least resistance … wait until you do have a message and you're ready to identify stakeholders and you're at the point of identifying how we might get this message out. But I think we could do with having it a little earlier. (CS1 PI2)
Many of the respondents felt that in hindsight their own KTE activities would have been enhanced through earlier engagement with the model.
what we have learnt, is that you would start looking at this at a much earlier point … that you would actually put specific milestones and achievable goals in. (CS3)
Timely KTE activities were recognized as a key.
Theme 5 —
The Positive Role of Facilitation was recorded as a highly valued activity, in providing KTE opportunities, in this case provided to case study participants by members of the EMTReK team.
[facilitation] assisted with the refining, the scaling down, the making [the KTE plan] more realistic and in that way maybe making it more achievable. (CS3)
Familiarization with the model was considered to be essential for its faithful application by new users.
somebody who is focused on that particular model, who has seen it implemented maybe in a range of different contexts and they can pick up maybe the gaps that you have much more quickly, or they can help you to put a different lens on something … not to feel that you have to do it all by yourself. (CS3)
There was also a recognition of value in using EMTReK without requiring an appreciation of its theoretical underpinning theory; for such users having the ongoing support of an experienced facilitator or support team was felt to be crucial.
there'd be different rules for different people and that comes back to a kind of a spectrum from the original thought right through to the end product and not everybody needs to be working at all of it … there's help in the framework to guide the thinking, the role of a facilitator in understanding the whole journey. (CS1 PI2)
Proposed forms of facilitation included the development of accompanying guidance documentation, a searchable database of EMTReK case studies, or the development of a network of experienced mentors or champions.
Theme 6 —
Resources for KTE and funding to support effective KTE was recognized as necessary right from the beginning of a research project and beyond.
even something like open access publications which we are much better at now, but for infographics, videos, there is that opportunity to do that type of dissemination and make sure that they are building in realistic costs for that. (CS1 PI1)
The offer of a small amount of funding was recognized as an element which affected the decision for respondents to participate as a case study.
It can't be overlooked that there was some support for some of the resources which was good … So there was an incentive there. (CS5)
While the funding received was small respondents commented on the effect that it had on highlighting KTE as a valuable component of the whole research process.
I felt we got the money to develop the [KTE plan] which was so helpful at that time because it gave it the level of impact. (CS4)
Researchers recognized that failure to include sufficient resources early in the planning of research limited the scope of KTE.
Theme 7 —
Enhancing Research Quality through engaging with EMTReK was identified as an unexpected outcome.
I have never historically, particularly let people know as I was doing a project … I think maybe I've been worried before that somebody would say well why didn't you do such and such and I'd have to change my project but actually that's probably the best thing that could happen, you know? (CS2)
Some participants had already used the model in guiding the development of new research and had shared the model with colleagues to guide their KTE plans.
it's going to make your proposal a little bit stronger and a little bit more robust because you'll have thought through the issues with a bit more depth. (CS3)
Theme 8 —
Limitations or Areas for Further Consideration were identified. There were perceived risks of the model being perceived as overly complex by those unfamiliar with using models or else too simplistic at face value to account for KTE complexity.
there's a certain anxiety in presenting the whole thing … at one go. It's a guide to a working process … it's going to need a bit of working through to identify the meaning for any particular project. (CS1 PI2)
Terminology used was considered to be off-putting for some.
some of the language in it initially I wasn't sure what was being asked for. (CS5)
Evaluation of the KTE process for each of the case studies was conducted by the EMTReK team and this was recognized as a weakness.
The component that I think that they will be least familiar with is the evaluation, the idea of actually assessing how well you did. (CS1 PI1)
we haven't yet really embraced evaluation of the process, so that's there to be thought about. (CS1 PI2)
Lack of specificity of the model to palliative care and its perceived applicability to wider health-care research were seen as both as strength and a weakness.
Discussion
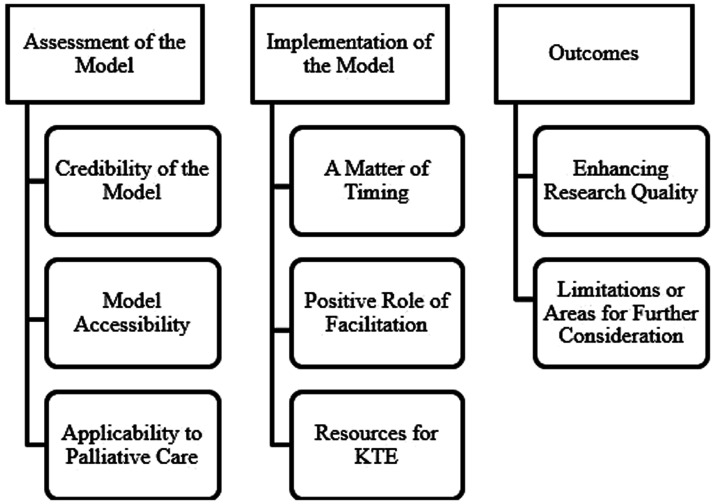
This study considered the use of the newly developed EMTReK model to support the transfer and exchange knowledge emerging from palliative care research. Researchers who were interviewed for this study held generally positive views regarding the use of EMTReK for their KTE activities. Case study findings related to how the model was interpreted (assessment of the model) operationalized by participants (implementation of the model) and its impact on KTE (outcomes) as depicted in Figure 1.
Figure 1.
Alignment of themes to the interpretation, operationalization, and impact of EMTReK.
KTE plans did not remain static, instead developing and changing as research progressed, and were influenced by stakeholders, funders, organizational influences, and external factors as previously described (Brereton et al., 2017). Prior to engaging in the case study, PIs did not report using guidelines or frameworks as a core component of their KTE strategy. An ad hoc and opportunistic time and resource bound approach was often adopted which failed to ensure that all stakeholders were adequately targeted in KTE activities, especially potential stakeholders from difficult to access groups. Understanding the different personal internal and external drivers which affect stakeholder engagement in KTE is a key to this process (Brereton et al., 2017; Daveson et al., 2015).
Strengths and Limitations
This study draws on a small sample of researchers, which may limit the generalizability of the findings; however, the dynamic engagement with the participants while they used the model is a strength of the study. Also, the case studies were selected to ensure diversity in both the experience of the researchers and the focus of their research. As a series of case studies set to support the use of an existing KTE model, the full rigors of qualitative methods were not deemed appropriate: We did not seek thematic saturation, nor systematically verify findings with participants. Rather we applied a pragmatic approach to address the study objective and gather support for specific components and subcomponents identified in previous work.
While evaluation of KTE was identified as a novel and interesting component of EMTReK, many of the researchers involved in the case studies reported that a formal process surrounding KTE was a quite new and potentially daunting concept and a decision was therefore made by the EMTReK team to centralize evaluation for pragmatic reasons. It remains to be determined how practical the process of evaluation is for all those who would seek to use EMTReK and what support may be required to ensure the utility of this particular model component.
Implications for Practice
A vital component of the EMTReK model appears to be the appropriate support and guidance to researchers to produce a KTE strategy considerate of the complexity of disseminating new knowledge to and about vulnerable groups, such as those in receipt of, or requiring, palliative care services (Gysels et al., 2013). Meyer (2010) contests that support with knowledge transfer through knowledge brokering is recognized as key “to move knowledge around and create connections between researchers and their various audiences” (p118). A collaborative, iterative, and mixed methods approach to the development of an appropriate evidence base for palliative care practice has been championed by experts in the field (Aoun & Nekolaichuk, 2014; Visser, Hadley, & Wee, 2015). Our recognition of the local and wider context encouraged palliative care researchers to be considerate of the specific challenges and supports for KTE in their own settings.
The original aims of the EMTReK project were to adapt and validate a specific model of KTE for use within palliative care settings. Following systematic review, expert consensus, and iterative refinement, a model was produced which has the potential for broader application to health-care research. While EMTReK has potential for broad application to health research, the exploratory case studies were conducted within palliative care settings. The credibility, accessibility, and applicability of EMTReK within other health-care settings remain to be established. In addition, though findings from the case studies suggested great utility for the model within palliative care contexts, the potential added contribution of a palliative care specific model would require further exploration.
Conclusions
This study has explored the utility of EMTReK to enable the optimal transfer and exchange of key messages arising from a range of studies conducted within palliative care settings. The initial assessment of the model through the case studies highlights the key strengths of the model in terms of its credibility, its accessibility, and most importantly its applicability to palliative care. The findings would indicate that the study participants found the model useful as a guide to the creation of better KTE plans that depended upon adequate facilitation and guidance on its use.
The team are currently seeking expressions of interest from palliative care researchers internationally to evaluate the model for their own KTE practices. As the model was derived from wider health-care research, the team are also exploring its utility within other nursing and health-care settings. More detailed guidance is needed to support researchers to achieve optimal KTE outcomes, and these are currently being produced in collaboration with the All Ireland Institute of Hospice and Palliative Care, to support the faithful application of the model concepts for those who are unfamiliar with it. In addition, the team are developing online support materials in the form of case studies and other examples of application of the key concepts from the model. Workshops on the use of the model are currently in the development with the potential to access individual facilitation for research teams who require this. Information on EMTReK is available at www.knowledgetransfer.ie. The EMTReK team invite researchers to use the model and input into its further development through reflection on its application to practice.
Key Statements
What is already known about this topic? • Practical models are needed to guide and facilitate knowledge transfer and exchange (KTE) to positively influence palliative care research, training, and practice. What does this paper add? • This study demonstrates that an Evidence-based Model for the Transfer and Exchange of Research Knowledge can guide the creation of better KTE plans in palliative care when combined with adequate facilitation. • When developing a KTE plan, a range of components are necessary for effective KTE. • Timeliness, appropriate guidance, and resourcing are recognized as important facilitators to optimal KTE. Implications for practice, theory or policy? • This study highlights the potential impact of a facilitated model to optimize KTE plans within palliative care. • Further research is needed to evaluate the model and develop facilitation guidance and support within different settings.
| What is already known about this topic? • Practical models are needed to guide and facilitate knowledge transfer and exchange (KTE) to positively influence palliative care research, training, and practice. |
| What does this paper add? • This study demonstrates that an Evidence-based Model for the Transfer and Exchange of Research Knowledge can guide the creation of better KTE plans in palliative care when combined with adequate facilitation. • When developing a KTE plan, a range of components are necessary for effective KTE. • Timeliness, appropriate guidance, and resourcing are recognized as important facilitators to optimal KTE. |
| Implications for practice, theory or policy? • This study highlights the potential impact of a facilitated model to optimize KTE plans within palliative care. • Further research is needed to evaluate the model and develop facilitation guidance and support within different settings. |
Supplemental Material
Supplemental Material for EMTReK: An Evidence-based Model for the Transfer & Exchange of Research Knowledge—Five Case Studies in Palliative Care by Cathy Payne BSc, PgD, MSc, PhD, RD Mary J. Brown BSc, PgD, PhD, RD Suzanne Guerin BA, PhD W. George Kernohan BSc, PhD, FHEA, FNCUP in SAGE Open Nursing
Authors’ Contributions
All authors have agreed on the final version and meet the criteria as specified.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval
Ethical approval was obtained from the Ulster University: Nursing and Health Research Governance Filter Committee and University College Dublin: Human Research Ethics Committee, Humanities Subcommittee.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by All Ireland Institute of Hospice and Palliative Care (Contract WP-8).
References
- Aoun S. M., Nekolaichuk C. (2014) Improving the evidence base in palliative care to inform practice and policy: Thinking outside the box. Journal of Pain and Symptom Management 48(6): 1222–1235. [DOI] [PubMed] [Google Scholar]
- Braun V., Clarke V. (2006) Using thematic analysis in psychology. Qualitative Research in Psychology 3(2): 77–101. [Google Scholar]
- Brereton L., Ingleton C., Gardiner C., Goyder E., Mozygemba K., Lysdahl K. B., Oortwijn W. (2017) Lay and professional stakeholder involvement in scoping palliative care issues: Methods used in seven European countries. Palliative Medicine 31(2): 181–192. [DOI] [PubMed] [Google Scholar]
- Craig P., Dieppe P., Macintyre S., Michie S., Nazareth I., Petticrew M. (2008) Developing and evaluating complex interventions: The new Medical Research Council guidance. British Medical Journal 337: a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daveson B. A., de Wolf-Linder S., Witt J., Newson K., Morris C., Higginson I. J., Evans C. J. (2015) Results of a transparent expert consultation on patient and public involvement in palliative care research. Palliative Medicine 29(10): 939–949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gysels M., Evans C. J., Lewis P., Speck P., Benalia H., Preston N. J., Higginson I. J. (2013) MORECare research methods guidance development: Recommendations for ethical issues in palliative and end-of-life care research. Palliative Medicine 27(10): 908–917. [DOI] [PubMed] [Google Scholar]
- Kernohan, W.G., Brown, M.J., Payne, C., & Guerin, S. (2018). Barriers and facilitators to knowledge transfer and exchange in palliative care research. BMJ Evidence-Based Medicine, 23, 131–136. [DOI] [PubMed]
- Meyer M. (2010) The rise of the knowledge broker. Science Communication 32(1): 118–127. [Google Scholar]
- Prihodova, L., Guerin, S., Tunney C., & Kernohan, W.G. (2019). Key Components of Knowledge Transfer & Exchange in Health Services Research: Findings from a Systematic Scoping Review. Journal of Advanced Nursing, 75, 313–326. [DOI] [PMC free article] [PubMed]
- Tieman J. J., Sladek R. M., Currow D. C. (2009) Multiple sources: Mapping the literature of palliative care. Palliative Medicine 23(5): 425–431. [DOI] [PubMed] [Google Scholar]
- Visser C., Hadley G., Wee B. (2015) Reality of evidence-based practice in palliative care. Cancer Biology & Medicine 12(3): 193–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward, J., Grimshaw, J., & Eccles, M. (2013). Knowledge transfer. In C. Guest, W. Ricciardi, I. Kawachi, & I. Lang (Eds.), Oxford handbook of public health practice (3rd ed., pp. 540–547). Oxford, England: Oxford University Press.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for EMTReK: An Evidence-based Model for the Transfer & Exchange of Research Knowledge—Five Case Studies in Palliative Care by Cathy Payne BSc, PgD, MSc, PhD, RD Mary J. Brown BSc, PgD, PhD, RD Suzanne Guerin BA, PhD W. George Kernohan BSc, PhD, FHEA, FNCUP in SAGE Open Nursing