Abstract
Abstract Aims
This study explored the effectiveness of a modified Lifestyle-integrated Functional Exercise program for increasing community-dwelling older adults’ lower body strength and balance to decrease fall risk.
Methods
Purposive sampling of men and women aged 65 years and older, with or without a history of falls, living at retirement communities yielded 19 older adult participants, and 16 of the participants completed the 26-week integrated exercise program. The program consisted of five-group training sessions focused on how to integrate individualized exercises into everyday activities, followed by 20 weeks of independent practice with a booster session at Week 10 and two phone calls at Week 15 and Week 20. A battery of assessments was used 3 times to measure the participants.
Results
Results demonstrated a significant improvement in lower body strength and balance, but fall risk reduction cannot be confirmed from this study.
Conclusion
Despite reduction in fall risk was inconclusive from this study, a modified Lifestyle-integrated Functional Exercise program delivered to community-dwelling older adults in a group format may be an effective intervention program to improve lower body strength and balance, while integration of exercises into daily activities may also appear to be more sustainable than traditional exercise program.
Keywords: community-dwelling, occupational based, integrated exercise, exercise adherence, healthy aging
Introduction
Advances in health care have significantly increased the average life expectancy of Americans (Centers for Disease Control and Prevention [CDC], 2013). However, this increase in life expectancy introduces a plethora of health conditions, ailments, and age-related concerns (CDC, 2013). Perhaps one of the greatest concerns facing the aging population is falls. The CDC (2016) estimated one of the four older adults falls every year, resulting in 2.8 million visits to the emergency department, and in 2014, over 80,000 older adults sustained a fall-related traumatic brain injury or hip fractures that threatened the adults’ ability to live independently. As falls can also jeopardize older adults’ ability to age-in-place or safely, independently, and comfortably live in their own home and community, occupational therapists play a pivotal role in fall prevention through the promotion of safe engagement in occupations and occupation-based fall prevention programs.
The use of exercise to maintain and improve strength and balance is effective in minimizing fall risk in older adults. The CDC (2015) identified 15 evidence-based single interventions, with the use of exercise only, as effective fall prevention programs. Many of these interventions are individual or group-based traditional exercise programs where strength and balance exercises follow a specific structure and schedule. Examples of these traditional and evidenced-based programs include Stay Safe, Stay Active, Tai Chi: Moving for Better Balance, and The Otago Exercise Program (Barnett, Smith, Lord, Williams, & Baumand, 2003; Campbell, Robertson, Gardner, Norton, & Buchner, 1999; Campbell et al., 1997; Li et al., 2005; Robertson, Devlin, Gardner, & Campbell, 2001; Robertson, Gardner, Devlin, McGee, & Campbell, 2001). Of the 15 evidence-based exercise programs listed, LiFE: Lifestyle-integrated Functional Exercise is the only exercise program where exercises are embedded into the participants’ daily life (Clemson et al., 2012).
Stay Safe, Stay Active is a group exercise program that requires older adults to meet once a week for a total of 37 sessions. The exercises were designed by a physical therapist and include balance, coordination, strength building, and aerobic exercises. Barnett et al. (2003) found that older adults who attended a median of 23 sessions, together with weekly home exercises, reduced fall rates by 40% during the 12-month trial period. Similarly, Li et al. (2005), using a randomized controlled trial, found that 26 weeks of the group Tai Chi: Moving for Better Balance Program, when compared with a stretching exercise group, could reduce the risk of multiple falls by 55% for adults aged 70 years and older. Both of these are examples of structured exercise programs when participants engaged in weekly exercise sessions.
Another exercise program with strong evidence is the Otago Exercise Program (Campbell et al., 1997, 1999; Robertson, Delvin, et al., 2001; Robertson, Gardner, et al., 2001). The Otago Exercise Program is an individualized exercise intervention delivered by either a physical therapist or a trained nurse. The exercises include lower extremity strengthening, balance, and stability; active range of motion exercises; and finally, a walking program. The participants were expected to dedicate time daily to do the exercises. Evidence showed that adults who were 80 years and older and who had had a history of a fall(s) in the previous year had the greatest benefit from the Otago Exercise Program with a 30% reduction in fall rate (Campbell et al., 1997; Robertson, Gardner, et al., 2001). Furthermore, in a 2-year extended study, the older adults complying with the Otago Exercise Program remained significantly lower in rate of falls and higher in physical level of activity (Campbell, et al., 1999).
However, the benefits of exercises can be quickly lost when the exercise is not adequate in frequency or stopped totally. Through a systematic review, Sherrington, Tiedemann, Fairhall, Close, and Lord (2011) found that to improve balance, exercise must be of high quantity, such as exercising 2 hours a week for 6 months, and that ongoing exercise was essential to bring about long-term fall prevention outcomes. Unfortunately, the traditional evidence-based exercise programs that have been proven to reduce fall risk may not be sustainable, as barriers limiting older adults’ long-term participation exist. These barriers may include decreased professional guidance, increased physical limitations, decreased access to exercise environments, increased financial and time demands, and considering exercise as an additional chore (Bethancourt, Rosenberg, Beatty, & Arterburn, 2014; Gardner et al., 2014). Hurley, Lyle, and Hyner (2014) also discovered that limited time and energy, lack of enjoyment, and motivation as the top three barriers for older adults to engage in regular physical activity. On the other hand, emerging evidence suggests that integrated exercise programs may be more effective in reducing fall risk in older adults because of the feasibility for frequent exercises throughout the day at home and sustainability over time (Burton, Lewin, Clemson, & Boldy, 2014; Clemson et al., 2012; Opdenacker, Boen, Coorevits, & Delecluse, 2008).
An integrated exercise program is an intervention where endurance, strength, flexibility, and balance exercises are incorporated into everyday activities and routines (Burton et al., 2014; Clemson et al., 2012; Opdenacker et al., 2008). In 2012, Clemson et al. developed the Lifestyle-integrated Functional Exercise (LiFE) program as a novel approach to fall prevention for community-dwelling older adults. The LiFE program consists of balance exercises such as reducing base of support and stepping over objects and incorporates lower extremity strengthening exercises such as standing on tiptoes, bending knees, and climbing stairs that can be completed throughout the day in the individual’s environment as part of his or her own routine (Clemson et al., 2012).
Using a three-arm randomized parallel trial, Clemson et al. (2012) examined the effects of the LiFE program when compared with a structured exercise program and a flexibility exercise program. The researchers aimed to assess whether an integrated exercise program delivered individually at home was effective in reducing fall risk in community-dwelling older adults who previously experienced two or more falls or an injurious fall within a year of the study. Results of their study found that 64% of the LiFE older adults adhered to the lifestyle-integrated program, whereas only 53% of the participants adhered to the structured and control programs (Clemson et al., 2012). In addition, falls among the older adults in the LiFE and structured exercise groups decreased by the end of the study. However, the community-dwelling older adults in the LiFE program had a 31% reduction in fall rate, while the older adults involved in the traditional structured exercise group experienced no significant reduction in fall rate (Clemson et al., 2012). Therefore, the results of Clemson et al.’s study demonstrated that embedding exercises into everyday activities and routines was effective in reducing fall rate among community-dwelling older adults who had previously fallen and therefore at high fall risk.
A follow-up study conducted by Burton et al. (2014) provided further evidence that the LiFE program can improve community-dwelling older adults’ balance and strength and increase exercise adherence. Burton et al. examined the long-term effectiveness of the LiFE program when delivered as a component in a restorative home care program. Results of the LiFE group showed significant improvement in balance and lower body strength when compared with the structured exercise group immediately after intervention and at the 6-month follow-up point. Furthermore, the study showed that in a 6-month period, participants in the LiFE group exercised more than those in the structured exercise group, an average of 4.05 versus 3.66 times per week, respectively. Although the results demonstrated that the LiFE program only marginally improved adherence rate in older adults, the authors concluded that LiFE was particularly appropriate for older adults who did not like to participate in structured exercise program, who did not like to use weights or resistive exercise bands, and who had limited time to fit structured exercise program into their routine (Burton et al., 2014).
In 2016, Fleig et al. conducted a mixed study design, using both quantitative and qualitative measures, to further provide evidence of the effectiveness of the LiFE program on community-dwelling middle-aged and older adults. Fleig et al.’s (2016) study examined the possibility that the LiFE program created habit formation and promoted behavior change in inactive women. A Short Physical Performance Battery and a self-reported psychosocial measure were utilized to collect quantitative data and a semistructured interview at the final session collected qualitative data. Results indicated that the LiFE program was effective in changing exercise behavior in older inactive women. Specifically, the qualitative results illustrated improved satisfaction in the women’s experience with balance and strength exercises. The results also revealed that exercises integrated into everyday activities increased the older women’s automaticity and sustainment of physical activity (Fleig et al., 2016). Finally, a recent study on a 4-week lifestyle-integrated, home-based exercise training program also found significant improvements in lower extremity strengths in older adults (Cegielski et al., 2017). Taken together, the latest studies using lifestyle-integrated exercise approach provide crucial evidence that simple, low-intensity, short-lived activities that are easily integrated into older adults’ everyday activities are more effective in habit formation than traditional strength and balance exercises and therefore, a more sustainable fall prevention program (Burton et al, 2014; Cegielski et al., 2017; Clemson et al., 2012; Fleig et al., 2016).
As only older adults with a significant history of falls or injurious falls were recruited in the original study by Clemson et al. (2012), limited evidence exists that the LiFE program can decrease the fall risk in older adults who have minor falls or who have not previously fallen. Therefore, this study utilized a modified form of the LiFE program (modified LiFE) to explore the effectiveness of integrating strength and balance exercises into everyday activities to decrease the fall risk in older adults with (fallers) or without a recent history of falls (nonfallers). The hypothesis for this study was that the modified LiFE program would be effective in increasing lower body strength and balance, decreasing fall risk, and increasing habit formation and sustainability of exercise in older adults, fallers, and nonfallers who reside in residential retirement communities.
Methods
Design
This study utilized a single-group quasi-experimental pretest–posttest research design. Two modifications were made to the original LiFE program developed by Clemson et al. (2012), as the original LiFE program was delivered one-on-one at older adults’ homes, and herein, the LiFE program was delivered to 6 to 10 older adults in a group in the activity rooms of the residential communities. Hence, the exercises were integrated into each older adult’s everyday activities through discussion and simulated demonstration instead of actual practice in the real home environment. Furthermore, the original LiFE program included two booster sessions at Week 8 and Week 12, and herein, the administration of the booster session was modified into a single booster session at Week 10 and two follow-up phone calls at Week 15 and Week 20. Hence, a modified version of the LiFE program was applied in this study.
A battery of fall risk assessments including the 30-second Chair Stand Test (CST), the Functional Reach Test (FRT), the Timed Up and Go (TUG) manual assessment, and the One-Legged Stand (OLS) were utilized as pretest, posttest, and follow-up assessments. Results of these assessments were analyzed to explore the effectiveness of the modified LiFE program in increasing lower body strength and balance and decreasing fall risk in retirement community-dwelling older adults aged 65 years and older. To assess whether the modified LiFE program was sustainable among participants, the LiFE Activity Planner and the LiFE Activity Counter Forms, which were developed by Clemson, Munro, and Singh (2014b) and outlined in the Lifestyle-integrated Functional Exercise program to prevent falls: Trainer’s manual (Sydney: Australia), were used to track participants’ daily progress in completing the strength and balance exercises that were taught to them.
Participants
Participants were recruited through purposive sampling of men and women aged 65 years and older, living in Aldersly and The Redwoods retirement communities in California, with or without a recent history of falls. Once approval was obtained from the Institutional Research Board for Protection of Human Subjects from Dominican University of California, recruitment efforts began with a write up in The Redwoods Newsletter, flyer distribution, and informational tabling sessions at both facilities. No gender-, racial-, or ethnic-based enrollment restrictions were included. To be included in the study, participants had to be fluent in English. Both fallers and nonfallers were included, and a faller was defined as having a history of fall in the previous 6 months prior to the start of the study. Participants also had to be able to ambulate independently, with or without the use of a cane. However, any observed instability in mobility with or without the use of a cane, and per staff report at Aldersly and The Redwoods retirement communities were taken into consideration for exclusion from the study. Cognition was screened using the Montreal Cognitive Assessment (MoCA©), a valid and sensitive screen for mild cognitive impairment (Nasreddine et al., 2005). Authorization to use MoCA© was obtained for this study. Older adults who had scored less than 18 of the 30 in the MoCA© were excluded from the study, as they would not be able to safely complete the modified LiFE program without supervision. Finally, older adults were asked to continue with their regular physical activities while participating in the modified LiFE program. Physical Activity Forms were used during the pretest, posttest, and follow-up assessments to monitor participants’ physical activities. Therefore, information about participants who altered their engagement in their preintervention physical activities during the 6-month intervention period was taken into consideration during data analysis.
Intervention
The LiFE program is a client-centered approach that incorporates balance and lower extremity strengthening exercises into participants’ everyday activities and routines. By integrating the exercises into everyday activities, the emphasis is on performing the exercises frequently and regularly, in the participant’s own environment when opportunity arises throughout the day. The LiFE program consists of seven strength and seven balance exercises. Strength exercises include standing on tiptoes, standing on heels, bending knees, siting-to-stands, tightening muscles, walking sideways, and climbing stairs. Balance exercises include standing with feet together, tandem standing, standing on one leg, shifting weight, moving to limits of sway, stepping over objects, and turning and changing directions. Examples of the LiFE integrated into everyday activities exercises include standing on one leg while brushing teeth, tandem standing while waiting in line, or bending knees while putting dishes into the dishwasher.
Participants in both residential communities attended five group sessions to learn the LiFE program exercises. Each participant received a copy of the original LiFE Participant’s Manual (Clemson, Munro, & Singh, 2014a), which contained images and written descriptions of the strength and balance exercises. Each exercise, however, was further individualized and graded to match each participant’s needs and ability during the group sessions. In addition to the LiFE Participant’s Manual, participants were given a Daily Routine Chart to help identify opportunities to perform the exercises during everyday activities and routines. The Daily Routine Chart was used to facilitate discussion during each group session to further help shape the participants’ integration of the exercises into everyday activities.
The LiFE Activity Planner and the LiFE Activity Counter Forms were used to track participants’ daily exercise frequency and adherence with each of the prescribed exercises. The LiFE Activity Planner and the LiFE Activity Counter Forms were collected regularly throughout the 6-month intervention. Initially, the completed forms were collected weekly during Week 2 to Week 6 group sessions. Then, following the posttest at Week 7, participants continued to use the LiFE Activity Planner and the LiFE Activity Counter Forms to record their exercises on their own, and the completed forms were collected during the booster session at Week 10. Finally, a binder containing the two forms was given to each participant for recording from Week 11 to Week 26.
Two follow-up phone calls were made at Week 15 and Week 20 to provide support and encouragement and to facilitate problem-solving for the participants on how to integrate exercises into everyday activities. Finally, the participants were reassessed during the follow-up session at Week 26. Four investigators, occupational therapy graduate students, conducted the modified LiFE group program and completed all assessments per the outlined time frame (Table 1). To ensure consistency and continuity, the same two investigators met with the same group of participants in each retirement community throughout the intervention. In addition, and perhaps most importantly, the four investigators, guided by the first author who has extensive experience in fall prevention interventions, met weekly to discuss individual grading and daily integration strategies to maximize participants’ benefit.
Table 1.
Overview of the LiFE Program.
| Week number | Participant procedures timeline |
|---|---|
| Week 1 | Formal screening session and pretest assessment |
| Week 2 | 1.5 Hour face-to-face session to learn balance and strength exercises |
| Week 3 to Week 6 | 1 Hour sessions to learn balance and strength exercises |
| Week 7 | Posttest assessment conducted |
| Week 10 | 1 Hour booster session to review balance and strength exercises and prepare for individual participation continuation of the LiFE program from Week 11 to Week 26 |
| Week 15 and Week 20 | 15 Minute follow-up phone calls to check on status and address any questions |
| Week 26 | Follow-up assessment |
Note. LiFE = Lifestyle-Integrated Functional Exercise. Adapted from Clemson et al. (2014b). Copyright 2014 by the Sydney University Press.
Data Collection
A battery of fall risk assessments was used to compare pretest, posttest, and follow-up scores for each participant. The 30-second CST was used to assess the participants’ lower body strength by counting the number of times a participant can rise to a full stand from a seated position within 30 seconds, without pushing from the armrests (Jones, Rikli, & Beam, 1999). The 30-second CST has good test–retest reliability (intraclass correlation coefficient [ICC] = .84–.92) and good construct and criterion validity for measuring lower body strength in older adults (Jones et al., 1999). The FRT yardstick method and TUG manual assessment were used to assess the participants’ fall risk. The FRT measures the distance between the participants’ arms’ lengths to their maximal forward reach, using a yardstick, while standing with a fixed base of support in which legs were positioned shoulder width apart (Duncan, Studenski, Chandler, & Prescott, 1992). The FRT has good to excellent reliability (ICC = .75–.99) and good concurrent validity for use as a functional balance assessment in community-dwelling older adults (Langley & Mackintosh, 2007). The TUG assessment has three versions: original, manual, and cognitive. Both TUG manual and TUG cognitive are in dual-task context, and the TUG manual requires participants to hold a cup of water while getting up from a chair, walking 10 feet at their regular pace safely to a line marked on the floor, crossing it, turning around, walking back, and sitting back down on the chair (Shumway-Cook, Brauer, & Woollacott, 2000). The TUG manual assessment was chosen because of its similarity to the LiFE program exercises in which the participants were to perform concurrent manual tasks while maintaining balance. For example, participant may choose to brush teeth while standing on tiptoes or walking sideway when bringing coffee to the table. The TUG manual assessment was found to have good validity and excellent interrater (ICC = .98–.99) and intrarater reliability (ICC = .97–.98) for community-dwelling older adults (Langley & Mackintosh, 2007). The cutoff point of reaching less than 10 in. in the FRT and walking slower than 14.5 seconds in TUG manual assessment were used to determine the risk of fall in older adult population (Duncan et al., 1992; Shumway-Cook et al., 2000). Finally, the OLS was used to assess participants’ balance over a reduced base of support. The OLS requires participants to choose their most comfortable leg to stand on, flex the opposite knee allowing the foot to clear the floor, and balance on one leg for as long as possible, up to a maximum of 30 seconds (Vellas et al., 1997). The OLS has good discriminant validity and good interrater and intrarater reliability (ICC = .93–.99) for assessing static balance in older adults aged 65 years and older (Lin et al., 2004).
The pretest data were collected before the start of the study at Week 1. The posttest and follow-up data were collected at Week 7 and Week 26, respectively. While the pretest data provided baseline information of the participants, the posttest and follow-up data provided information on the effect the modified LiFE program had on the participants’ lower body strength, balance, and fall risk since the start of the program. The binders containing the LiFE Activity Forms and LiFE Counter Forms provided information on how sustainable the modified LiFE program was for the participants when they were left to complete the program on their own during Week 11 to Week 26.
Data Analysis
Descriptive statistics were used to examine the demographics of the participants, including age, gender, fallers versus nonfallers, and use of mobility devices. For statistical analysis, the p was set at .05, indicating a 5% chance that results were not due to the modified LiFE program. Data obtained from the pretest, posttest, and follow-up were transferred from an excel spreadsheet to Statistical Package for Social Science® (SPSS®version 22). Data were compared at pretest, posttest, and follow-up using a repeated measure analysis of variance and paired t tests. A post hoc test was used to indicate any significant differences between data. Eta squared (η2) was applied to identify the effect size of the modified LiFE program. Attendance and participation were taken into consideration in this study; any participant who missed more than two of the five training sessions would be excluded from the final data analysis. However, for those participants who had completed all five group training sessions and participated in the posttest assessment, missing data due to attrition at the follow-up assessment were handled with the assumption that the program had no effect and that the participant was at his or her pretest level at Week 26 (i.e., change score was 0).
Results
A total of 19 participants were recruited from the independent living units in the retirement communities. Prior to completion of the study, three participants discontinued the study for personal reasons. The remaining 16 participants completed the training sessions in entirety and completed the posttest assessments, and thus, they were all included in the final data analysis. Participant demographics and fall history are listed in Table 2. Of the 16 participants, 15 (94%) reported prior engagement in traditional exercises, such as walking, strengthening and balancing exercises, or classes. Throughout the study, all participants agreed to maintain the same level of physical activity and to not begin any new exercise program, and the investigators reminded the participants regularly during the group training sessions and phone follow-up calls. Participant who reported new exercise routine or program within the 26-week program would be disqualified and removed from the data analysis. At Week 15 and Week 20, the investigators successfully connected with 53% and 40% of the participants, respectively, via phone follow-up. At the end of Week 26, follow-up data were collected for 13 participants (81%). Three participants (19%) were lost to the follow-up assessment as one was absent at the follow-up meeting, another participant discontinued the exercise program on her own due to medical reason, and one other participant was disqualified as she started new exercise program with physical therapy just 2 weeks prior to the follow-up meeting. Hence, missing follow-up data from these three participants were assigned the pretest scores (i.e., change score was 0) during data analysis.
Table 2.
Participants Demographics.
| Participant | Age | Gender | Assistive device | Pretest falls | Posttest falls | Follow-up falls |
|---|---|---|---|---|---|---|
| A | 97 | M | No | 0 | 0 | 0 |
| B | 91 | F | No | 0 | 0 | 1 |
| C | 87 | F | No | NR | 0 | 0 |
| D | 93 | F | Cane | NR | 0 | 0 |
| E | 85 | F | No | 1 | 0 | 0 |
| F | 94 | F | Cane | 0 | 0 | 0 |
| G | 78 | F | No | 0 | 1 | 0 |
| H | 85 | M | Cane | 1 | 0 | 0 |
| I | 94 | F | No | 0 | 0 | 0 |
| J | 86 | F | Cane | 2 | 0 | 0 |
| K | 84 | F | Cane | 3 | 0 | 0 |
| L | 88 | F | No | 0 | 0 | 1 |
| M | 91 | F | Cane | 1 | 0 | 0 |
| N | 83 | F | No | 0 | 1 | 0 |
| O | 87 | F | No | 0 | 0 | 0 |
| P | 84 | F | No | 0 | 0 | 0 |
| Mean (SD) | 87.94 (4.75) |
Note. NR = Participant left question blank, interpreted as zero falls; SD = standard deviation; M = male; F = female.
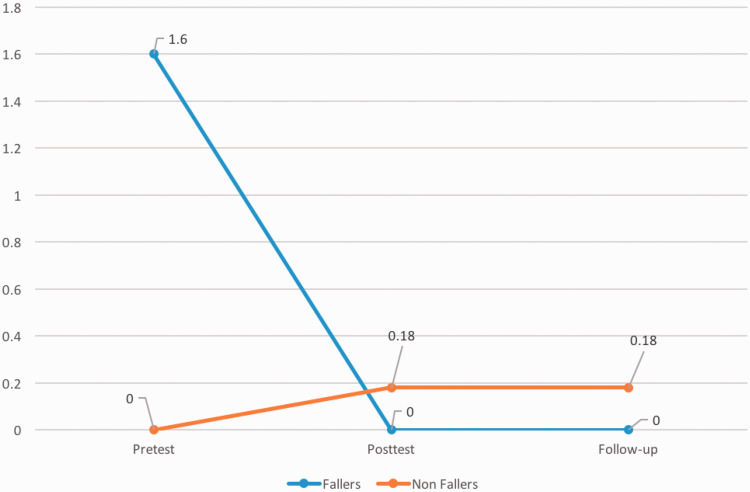
A comparison of the participants’ assessment mean scores for pretest, posttest, and follow-up are summarized in Table 3. The significance, F value, and effect size of these results are provided in Table 4. Although it was not the intention of this study to compare the faller versus the nonfaller groups, data collected between these two groups yielded secondary results. Prior to participation in the program, five participants reported a recent history of one to three falls (M = 1.60, standard deviation = 0.89) within 6 months of starting the program. At the follow-up assessment, all fallers reported no incidence of fall within the 26-week program. On the other hand, 11 participants did not have a history of fall when joining the program. At posttest time, two of the participants reported one fall incident each, and two different participants also reported one fall each between Week 7 and Week 26, resulting in an average of 0.18 (standard deviation = 0.4) fall for the nonfaller group in both posttest and follow-up periods (Table 2 and Figure 1).
Table 3.
Means (Standard Deviation) of Outcome Measures.
| Pretest | Posttest | Follow-up | |
|---|---|---|---|
| FRT | 8.5 (1.55) | 10.34 (1.72) | 9.56 (1.46) |
| TUG manual | 18.95 (4.23) | 17.11 (4.68) | 16.11 (3.86) |
| 30-second CST | 7.31 (4.21) | 9.25 (4.40) | 10 (4.84) |
| OLS | 3.47 (4.63) | 3.47 (3.86) | 7.90 (13.73) |
Note. Mean values of FRT measured in inches and mean values of TUG manual, 30-second CST, and OLS measured in seconds. FRT = Functional Reach Test; TUG = Timed Up and Go; CST = Chair Stand Test; OLS = One-Legged Stand.
Table 4.
Pairwise Comparisons p Values, ANOVA F Values, and Effect Size of Outcome Measures.
| Assessment | p (pretest– posttest) | p (posttest–follow-up) | p (pretest–follow-up) | ANOVA F value | η2 |
|---|---|---|---|---|---|
| 30-second CST | .006* | .287 | .001* | 8.952* | .374 |
| FRT | .001* | .080 | .014* | 10.169* | .404 |
| TUG manual | .018* | .228 | .002* | 7.417* | .331 |
| OLS | .997 | .167 | .151 | 2.157 | .126 |
Note. η2 = eta squared, effect size; CST = Chair Stand Test; FRT = Functional Reach Test; TUG manual = Timed Up and Go manual; OLS = One-Legged Stand; ANOVA = analysis of variance.
p < .05.
Figure 1.
Mean number of falls in fallers and nonfallers.
Summation of the total frequency of exercise participation from the weekly LiFE Activity Counter Forms at Week 11 to Week 26 determined the sustainability of the modified LiFE program during the time period the participants had no face-to-face contact with the investigators. The results were then graphed to determine trends. The curve of the graph was used to indicate trends such as an upward trend of improvement, a plateau trend of maintenance, a downward trend of decline, or total cessation of exercises. Of the 16 binders handed out, 8 (50%) were returned, and only 6 (38%) contained the requested information. Of the six binders completed, five revealed a trend toward maintenance of the LiFE program, and one indicated total cessation.
Discussion
The purpose of this study was to examine the effectiveness of the modified LiFE program in increasing lower body strength and balance and decreasing fall risk in community-dwelling older adults, both fallers and nonfallers. A battery of assessments was used to measure participants’ lower body strength and balance and risk of fall. From the pretest scores of both the FRT and the TUG manual assessments, most of the participants were at high risk for a fall prior to the start of the study. Similar to Clemson et al.’s (2012) original study on the LiFE program and Burton et al.’s (2014) study on older adults in home care service, the follow-up assessments at Week 26 revealed that the modified LiFE program was effective in increasing lower body strength and improving balance. However, fall risk reduction as revealed by FRT and TUG manual assessments could not be determined from the results.
The 30-second CST assessment was used to measure participants’ lower body strength. After participating in the 26-week modified LiFE program, the participants showed a steady and statistically significant improvement from pretest to the follow-up assessment with a moderate effect size. Hence, based on the significant increase in the group means for the number of chair stands completed in 30 seconds, the modified LiFE program had a positive effect on participants’ lower body strength, both immediately after the training at Week 7 and at the end of the program at Week 26. These results support the hypothesis that integrated exercise programs can be effective in increasing lower body strength in community-dwelling older adults who reside in retirement communities.
Likewise, as to the results in the 30-second CST, moderate effect sizes were found in both the FRT and the TUG manual assessments. The FRT is a measure of static balance when reaching over a stable base of support, and the TUG manual assessment measures both walking speed and dynamic balance. The findings also indicate that the modified LiFE program can improve static and dynamic balances in older adults and thereby may be effective in decreasing fall risk. Using a cutoff point of 10 in. (Duncan et al., 1992), results from the FRT showed that 76.9% of participants who completed the program changed their fall risk status from at risk for a fall to not at risk for a fall. Similarly, 84% of the participants decreased their times on the TUG manual assessment. However, using a cutoff time of 14.5 seconds (Shumway-Cook et al., 2000) in the TUG manual assessment, a reduction of 11 potential fallers at pretest to 9 at follow-up assessments was evident.
Both the FRT and the TUG manual assessments were found to have high sensitivity, 73% and 86.7%, respectively, and high specificity, 88% and 93.3%, respectively, in determining older adults who are fallers versus nonfallers (Murphy, Olson, Protas, & Overby, 2003; Shumway-Cook et al., 2000). In fact, the agreement between the FRT and the TUG manual assessment in determining fall risk in the participants was 88% in the pretest but dropped to 56% in the follow-up assessments. There are two possible explanations to the contradictory findings between the FRT and the TUG manual assessment: (a) a limitation of the TUG assessment and (b) the baseline discrepancy of the participants.
Literature reveals that one of the limitations of the TUG assessment is its inability to differentiate between dynamic balance versus walking subcomponents (Macini & Horak, 2010; Zampieri et al., 2010). Thus, even though participants showed decreased times in the TUG manual assessment in the 26-week follow-up when compared with pretest, there is no way to determine whether the improvement was due to the improvement in dynamic balance versus walking. In the LiFE exercise program, components of the TUG manual assessment that were practiced include sitting-to-stands, shifting weights, turning, and changing. Practicing walking or walking speed is not part of the program. On the other hand, the FRT is a simple test of static balance, and moving to limits of sway is one of the exercises in the LiFE exercise program that could have resulted in improvement in functional reach.
For baseline discrepancy, the participants had an average reach of 8.5 in. at pretest and therefore 15% short of the cutoff point of 10 in. On the other hand, at pretest baseline, the participants took an average of 18.95 seconds to complete the TUG manual assessment, which was nearly 31% over the cutoff time of 14.5 seconds. This may have indicated that the participants overall were better with their static balance when reaching to the limit of stability as compared with their dynamic balance in sitting-to-standing transition, walking, and turning. Hence, even though there were significant changes in both outcome measurements from pretest to follow-up assessments, the changes in the TUG manual assessment may not have been enough to cover the larger discrepancy toward the cutoff point. Therefore, taking the results from the FRT and the TUG manual assessment together, the effectiveness of the modified LiFE program in reducing fall risk in older adults residing in the retirement communities could not be confirmed in this study.
The OLS assessment was used to measure participants’ static balance over a very small base of support as well as lower extremity strength to hold the single-leg stance position for up to 30 seconds. While group means on the OLS increased from pretest to posttest to follow-up, the results did not change significantly after participating in the modified LiFE program. The nonsignificant results may be due to the low predictive validity or external variables of the OLS assessment (Lin et al., 2004). External variables affecting participants’ performance on the OLS may have included fatigue due to the order in which the OLS was completed with relation to the other fall risk assessments, and participants perceived self-efficacy on the day of the assessment. For consistency, the same leg that yielded the highest OLS score during pretest in each participant was used again in both posttest and follow-up. The decision to use a consistent leg in the repeated measurements may also have contributed to the nonsignificant results. As most of the participants were not aware they would have better performance standing on one leg over the other, both legs were assessed throughout the study. Although during the follow-up assessment, two participants demonstrated that significant improvement in standing and balancing on the leg opposite to the leg used in the pretest assessment, the data were not used in the analysis. Nonetheless, it is important to note that seven of the participants’ OLS times increased, five remained the same, and only four decreased, as compared with the pretest baseline data.
A comparison between the average number of falls between fallers and nonfallers at pretest, posttest, and follow-up sessions yielded significant incidental results. Data indicated that participants who were fallers at the start of the study, that is, with a history of fall in the prior 6 months, had significantly decreased their number of falls to zero by the end of the study at Week 26. Although participants who were nonfallers at the start of the study demonstrated a slight increase in the average number of falls, but the data did not reach statistical significance. Yet, this finding is congruent with the finding from the original study by Clemson et al.’s (2012) where fallers had significant decrease in the fall rate. The finding is also different in the sense that here only two of the five self-identified fallers had a history of multiple falls in the prior 6 months and none had a previous injurious fall, whereas in the Clemson et al.’s study, participants with multiple and self injurious falls were recruited. Several possible reasons explain this finding. One plausible reason was the investigators’ guidance and individualization of the exercises in the LiFE program allowed participants who had a fall history to participate in the exercises at their best ability and in a safe environment. Another possibility was participants’ increased effort to perform the exercises diligently in their own environment to avoid another fall. However, given the small number of fallers in this study, the results should be interpreted with caution. Nonetheless, this study may have lent further support to the LiFE program’s effectiveness, even in its modified format, as a beneficial program for those with a history of fall regardless of the number or seriousness of the falls.
It is important to point out that this study employed a modification in that the exercise instructions were delivered in a group format instead of individually delivered in the older adults’ home, as in the original study by Clemson et al. (2012), and had a focus on guidance from the investigators and individual participant needs. Although each participant followed the illustrated exercises in the LiFE Participant’s Manual for accuracy of the exercises, the success of the program could not be achieved without proper guidance, activity grading, and modification. Despite the group instructions, each exercise was individually graded up and down to match with the participants’ physical and mental abilities. In addition, personal routines and environments were taken into consideration during discussions in the five group meetings, the booster session, and the two telephone follow-up calls. More importantly, through activity analysis and the Daily Routine Chart, each participant received individualized strategies on how to integrate the exercises into his or her routine. Hence, the success of the program relies on proper guidance from trained personnel, such as occupational therapists, who have in-depth understanding of activity analysis and clients’ routines, habits, and environment.
Finally, as to the sustainability and program adherence of the lifestyle integrative approach to exercises, of the six returned and completed binders, 83% of the participants demonstrated a trend toward maintaining the established habits and routines of incorporating exercises into everyday activities. Although the result was drawn from a small number of participants who returned their binders, similar to the results from Opdenacker et al.’s (2008) and Fleig et al.’s (2016) studies, this study provides additional support that exercises integrated into everyday activities may be more sustainable than traditional exercise programs. However, the tedious process of logging in the exercises daily onto both the LiFE Activity Planner and the LiFE Activity Counter Forms may have prohibited the participants from recording their diligent efforts to comply with the program. In addition, the complexity of writing down information on two different forms increased the chance for self-reported and recall biases. Hence, other means of measurement, such as a simple checklist, may be more appropriate for older adults when assessing program adherence. Nevertheless, through personal testimonies in the follow-up sessions, many participants indicated their continuing participation in the LiFE program.
Limitations and Recommendations
A few limitations impact the results of the pilot study. Due to the limited number of participants recruited and attrition of three participants, the number of participants remaining at the end of the study was small. Hence, the results of the study have low power. Convenience sampling of participants only included community-dwelling older adults from two retirement residential communities, both in the same geographical area. Having a limited sample size and a narrow demographic limit the generalizability of the findings to a larger population, therefore, resulting in low external validity.
Limitations concerning the participants who threatened the internal validity of the study included the Hawthorne effect and the possibility of competition between participants. For Hawthorne effect, participants could have logged in more frequency and repetitions of the daily exercises on the LiFE Activity Counter Form in hope of pleasing the investigators. Even though there was no way for the investigators to verify the accuracy of the information, the investigators made every attempt to ensure that the participants had good understanding on how to record their exercise frequency and repetitions correctly on the LiFE Activity Counter Form. The investigators reviewed and discussed the results on both the LiFE Activity Planner Form and the LiFE Activity Counter Form with each participant weekly during Week 2 to Week 6 and then again at Week 10 of the program. Hence, the participants were not asked to independently record during the nontraining time of Week 11 to Week 26 until they have received adequate guidance on accurate recording on both tracking forms.
Without a control group to compare the results, participants in this study could have possibly exercised more than normal to please the investigators. Furthermore, as the program was conducted in a group setting, competition between participants was also a concern. To minimize these limitations, the investigators encouraged participants to engage in their LiFE program exercises for an amount of time appropriate for their own physical abilities, reminded them that the objective was not to be competitive, and emphasized that safety was the utmost priority.
An assessment-specific limitation worth considering is that of the practice effect. As the one-leg stand and sit-to-stand were also exercises assigned in the LiFE program, there may have been a practice effect associated with the assessment results. In particular, the OLS assessment and the one-leg stand exercise are identical, and a practice effect was expected to be most prominent with the OLS assessment. However, despite practice, the overall group means did not demonstrate a significant improvement in OLS at the end of the study. Similarly, the 30-second CST and the sit-to-stand exercise are alike. However, in the 30-second CST, participants were expected to complete continuous sit-to-stand for 30 seconds, and therefore it does not only measure lower body strength but also endurance within 30 seconds. As the sit-to-stand exercise in everyday activities are practiced in isolated incidences throughout the day without continuous repeated performance as in the 30-second CST assessment, the likelihood that there was a practice effect is minimized.
As demonstrated in this study, the LiFE program may be as effective when delivered in a group format in retirement communities, as it has been found to be individually at older adults’ homes in Clemson et al.’s study (2012). Hence, future research on group programs using the concept of integrated exercises with a larger sample size of older adults in a more diverse population, such as those residing in assistive living environment, may be warranted. In addition, it would be beneficial to have studies with a control group and of longer duration to investigate the possibility of long-term sustainability of integrated exercises as a single-intervention fall prevention program.
Conclusion
To sum, despite the limitations of a small convenient sample, this study adds to the evidence that exercises that are done frequently and regularly integrated into daily tasks throughout the day may be effective in increasing lower body strength and balance in older adults who reside in retirement communities with or without a recent history of falls. An incidental finding from this study also reveals that the LiFE program, in its modified format as delivered in a group setting, may be as effective as individual delivery in private homes to reduce falls in older adults with a history of fall(s). Most importantly, this study supports the benefits of utilizing a client-centered exercise program, where the focus is on each participant’s unique physical and mental abilities, personal routines, and environments. Therefore, occupational therapists may benefit from the use of integrated exercise programs to prevent falls and promote independence in meaningful occupations and ultimately assure successful aging in place in community-dwelling older adults.
Acknowledgments
The researchers would like to thank both Aldersly and The Redwood retirement communities in Marin County, CA, for agreeing to host them in their facilities for this study. The researchers would also like to give special thanks to all the participants of the study for their hard work and dedication to learning, practicing, and giving feedback to the strength and balance exercises that were taught to them.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This pilot study received Seed Money Grant from California Foundation of Occupational Therapy.
References
- Barnett A., Smith B., Lord S. R., Williams M., Baumand A. (2003) Community-based group exercise improves balance and reduces falls in at-risk older people: A randomized controlled trial. Age and Ageing 32(4): 407–414. doi:10.1093/ageing/32.4.407. [DOI] [PubMed] [Google Scholar]
- Bethancourt H. J., Rosenberg D. E., Beatty T., Arterburn D. E. (2014) Barriers to and facilitators of physical activity program use among older adults. Clinical Medicine & Research 12(1): 10–20. doi:10.3121/cmr.2013.1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton E., Lewin G., Clemson L., Boldy D. (2014) Long-term benefits of a lifestyle exercise program for older people receiving a restorative home care service: A pragmatic randomized controlled trial. Healthy Aging & Clinical Care in the Elderly 6: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell A. J., Robertson M. C., Gardner M. M., Norton R. N., Buchner D. M. (1999) Falls prevention over 2 years: A randomized controlled trial in women 80 years and older. Age and Ageing 28: 513–518. [DOI] [PubMed] [Google Scholar]
- Campbell A. J., Robertson M. C., Gardner M. M., Norton R. N., Tilyard M. W., Buchner D. M. (1997) Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. British Medical Journal 315(7115): 1065–1069. doi:10.1136/bmj.315.7115.1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cegielski, J., Brook, M. S., Quinlan, J. I., Wilkinson, D. J., Smith, K., Atherton, P. J., & Phillips, B. E. (2017). A 4- week, lifestyle-integrated, home-based exercise training programme elicits improvements in physical function and lean mass in older men and women: A pilot study. F1000Research, 6, 1235. doi:10.12688/f1000research.11894.2. [DOI] [PMC free article] [PubMed]
- Centers for Disease Control and Prevention. (2013). The state of aging and health in America 2013. Retrieved from https://www.cdc.gov/aging/pdf/State-Aging-Health-in-America-2013.pdf.
- Center for Disease Control and Prevention. (2015). A CDC compendium of effective fall preventions: What works for community-dwelling older adults. Retrieved from http://www.cdc.gov/homeandrecreationalsafety/pdf/falls/CDC_Falls_Compendium-2015-a.pdf#nameddest=single-interventions-exercise.
- Center for Disease Control and Prevention. (2016). Important facts about falls. Retrieved from http://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html.
- Clemson L., Munro J., Singh M. F. (2014. a) Lifestyle-integrated functional exercise (LiFE) program to prevent falls: Participant’s manual, Sydney, Australia: Sydney University Press. [Google Scholar]
- Clemson L., Munro J., Singh M. F. (2014. b) Lifestyle-integrated functional exercise (LiFE) program to prevent falls: Trainer’s manual, Sydney, Australia: Sydney University Press. [Google Scholar]
- Clemson, L., Singh, M. A. F., Bundy, A., Cumming, R. G., Manollaras, K., O Loughlin, P., & Black, D. (2012). Integration of balance and strength training into daily life activity to reduce rate of falls in older people (the LiFE study): Randomized parallel trial. British Medical Journal, 345, e4547. [DOI] [PMC free article] [PubMed]
- Duncan P. W., Studenski S., Chandler J., Prescott B. (1992) Functional reach: Predictive validity in a sample of elderly male veterans. Journal of Gerontology 47(3): M93–M98. [DOI] [PubMed] [Google Scholar]
- Fleig L., McAllister M. M., Chen P., Iverson J., Milne K., McKay H. A., Ashe M. C. (2016) Health behaviour change theory meets falls prevention: Feasibility of a habit-based balance and strength exercise intervention for older adults. Psychology of Sport and Exercise 22: 114–122. [Google Scholar]
- Gardner B., Thuné-Boyle I., Lliffe S., Fox K. R., Jefferis B. J., Hamer M., Wardle J. (2014) ‘On your feet to earn your seat’, a habit-based intervention to reduce sedentary behaviour in older adults: Study protocol for a randomized controlled trial. Trials 15(1): 368–380. doi:10/1186/1745-6215-15-368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurley K. S., Lyle R. M., Hyner G. C. (2014) Physical activity attitudes, beliefs, and practices among adults 50 and older: Baseline community assessment. Quarterly of Community Health Education 34(3): 235–254. doi:10.2190/IQ.34.3.c. [DOI] [PubMed] [Google Scholar]
- Jones C. J., Rikli R. E., Beam W. C. (1999) A 30-s Chair-Stand Test as a measure of lower body strength in community-residing older adults. Research Quarterly for Exercise and Sport 70(2): 113–119. [DOI] [PubMed] [Google Scholar]
- Langley F., Mackintosh S. F. (2007) Functional balance assessment of older community dwelling adults: A systematic review of the literature. The Internet Journal of Allied Health Sciences and Practice 5(4): Article 13. [Google Scholar]
- Li, F., Harmer, P., Fisher, K. J., McAuley, E., Chaumeton, N., Eckstrom, E., & Wilson, N. L. (2005). Tai chi and fall reductions in older adults: A randomized controlled trial. Journal of Gerontology: Medical Sciences, 60A(2), 187194.doi:10.1093/gerona/60.2.187. [DOI] [PubMed]
- Lin M. R., Hwang H. F., Hu M. H., Wu H. D. I., Wang Y. W., Huang F. C. (2004) Psychometric comparisons of the timed up and go, one-leg stand, functional reach, and Tinetti balance measures in community-dwelling older people. Journal of the American Geriatrics Society 52(8): 1343–1348. [DOI] [PubMed] [Google Scholar]
- Macini M., Horak F. B. (2010) The relevance of clinical balance assessment tools to differentiate balance deficits. European Journal of Physical Rehabilitation Medicine 46(2): 239–248. [PMC free article] [PubMed] [Google Scholar]
- Murphy M. A., Olson S. L., Protas E. J., Overby A. R. (2003) Screening for falls in community-dwelling elderly. Journal of Aging and Physical Activity 11(1): 66–81. [Google Scholar]
- Nasreddine Z. S., Phillips N. A., Bédirian V., Charbonneau S., Whitehead V., Collin I., Chertkow H. (2005) The Montreal Cognitive Assessment, MoCA©: A brief screening tool for mild cognitive impairment. Journal of the American Geriatrics Society 53(4): 695–699. [DOI] [PubMed] [Google Scholar]
- Opdenacker J., Boen F., Coorevits N., Delecluse C. (2008) Effectiveness of a lifestyle intervention and a structured exercise intervention in older adults. Preventive Medicine 46(6): 518–524. [DOI] [PubMed] [Google Scholar]
- Robertson M. C., Devlin N., Gardner M. M., Campbell A. J. (2001) Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls. 1: Randomised controlled trial. British Medical Journal 322(7288): 697–700. doi:10.1136/bmj.322.7288.697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson M. C., Gardner M. M., Devlin N., McGee R., Campbell A. J. (2001) Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls. 2: Controlled trial in multiple centres. British Medical Journal 322(7288): 701–704. doi:10.1136/bmj.322.7288.701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherrington C., Tiedemann A., Fairhall N., Close J., Lord S. (2011) Exercise to prevent falls in older adults: An updated meta-analysis and best practice recommendations. New South Wales Public Health Bulletin 22(3-4): 78–83. doi:10.1071/NB10056. [DOI] [PubMed] [Google Scholar]
- Shumway-Cook A., Brauer S., Woollacott M. (2000) Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go test. Physical Therapy 80(9): 896–903. [PubMed] [Google Scholar]
- Vellas B. J., Wayne S. J., Romero L., Baumgartner R. N., Rubenstein L. Z., Garry P. J. (1997) One-leg balance is an important predictor of injurious falls in older persons. Journal of the American Geriatrics Society 45(6): 735–738. [DOI] [PubMed] [Google Scholar]
- Zampieri C., Salarian A., Carlson-Kuhta P., Aminian K., Nutt J. G., Horak F. B. (2010) The instrumented Timed Up and Go test: Potential outcome measure for disease modifying therapies in Parkinson’s disease. Journal of Neurology, Neurosurgery & Psychiatry 81(2): 171–176. [DOI] [PMC free article] [PubMed] [Google Scholar]