Abstract
The collaborative care model is an effective model for improving depression symptoms in patients in a primary care (PC) setting. An essential role in this model is the care manager (CM), and nurses have been effective in this role. However, there remains a question of how to best design, train, and implement this nurse CM role in PC. The purpose of this review is to provide readers with a critical description of what processes for training and implementation of a collaborative nurse CM role have been be successful in the literature, specifically as it pertains to supporting patients with depression and chronic medical illnesses in an integrated PC setting. A literature review of PubMed, CINAHL, PsychINFO, Scopus, and the Cochrane Collaborative was conducted in October 2018. Successful nurse CM interventions have included regular patient follow-up, symptom check-in, treatment monitoring, goal setting, and education. Psychological support techniques such as Problem-Solving Therapy, behavioral activation, and motivational interviewing have been useful in supporting patient care-plan engagement and goal achievement. Nurse CM training should support the successful implementation of the designed role. Nurse CMs have an opportunity to significantly impact depressive outcomes of patients with depression and long-term health conditions. Further research is needed to explore the potential that this nursing role has as well as how to best operationalize this role.
Keywords: anxiety, business concepts, case management, chronic illnesses, depression, mental health, mental health, practice, primary care
Introduction/Background
Depression is a worldwide medical problem affecting 300 million individuals and is the leading cause of disability (World Health Organization, 2018). The National Ambulatory Medical Care Survey revealed that in 2015, 59.8 million physician visits had depression as their primary diagnosis (Rui & Okeyode, 2015). These data are important, as consequences of depression can be severe. In 2014, 1.6% of deaths were attributed to intentional self-harm (suicide), making it the 10th leading cause of death (Kochanek, Murphy, & Tejada-Vera, 2016). Furthermore, depression is more common in people with chronic medical conditions than in the general population, and depression is a risk factor for heart disease, stroke, and diabetes mellitus (Clarke & Currie, 2009). Depression and diabetes mellitus can worsen both conditions' outcomes, likely through both biological and behavioral variables (Holt et al., 2014). Depression and a comorbid chronic health condition are associated with poorer quality of life, and the combination can lead to poorer health outcomes (Naylor et al., 2012).
The integration of mental health care into primary care (PC) has been shown to be effective in improving care for depression symptoms as well as for people with chronic health conditions (Naylor et al., 2012). One of the models for integrating behavioral health into PC is the collaborative care model (CCM). Developed in 1995, the CCM has been studied over the last two decades and has shown positive outcomes and symptom improvement (American Psychological Association & Academy of Psychosomatic Medicine, 2016; Katon et al., 1995). In the CCM, the care team often consists of the PC provider (PCP), a care manager (CM), and a mental health specialist, such as a psychiatrist or a psychologist (Archer et al., 2012). Essential elements of the CCM include the interdisciplinary care team, population-based care, measurement-guided care, and evidence-based care (Advancing Integrated Mental Health Solutions Center, n.d.; American Psychological Association & Academy of Psychosomatic Medicine, 2016). A Cochrane Collaborative review demonstrated that the CCM improved depression outcomes in the CCM intervention in 0 to 6 months (standardized mean difference [SMD] = −0.34, 95% confidence interval [CI; −0.41, −0.27]; risk ratio [RR] = 1.32, 95% CI [1.22, 1.43]), 7 to 12 months (SMD = −0.28, 95% CI [−0.41, −0.15]; RR = 1.31, 95% CI [1.17, 1.48]), and 13 to 24 months (SMD = −0.35, 95% CI [−0.46, −0.24]; RR = 1.29, 95% CI [1.18, 1.41]; Archer et al., 2012). Additional improvements were also seen in medication compliance, mental health-related quality of life, and treatment satisfaction among patients (Archer et al., 2012).
As a part of the CCM, the CM often has regular contact with the patient and helps coordinate care between the patient and other members of the care team (Archer et al., 2012). Although these themes are clear, the background and training of the CM and how the CM executes the CCM CM principles vary across different studies and practices. Richards et al. (2013) designed a CM intervention that utilized mental health workers. Training consisted of a 5-day training course, the content of which was not discussed (Richards et al., 2013). The Patient Health Questionnaire-Nine Item (PHQ-9) mean depression score was 1.33 points lower in the intervention group compared with the usual care group at 4 months (95% CI [0.35, 2.31], p = .009), with a standard effect size of 0.26 (95% CI [0.07, 0.46]; Richards et al., 2013). Björkelund et al. (2018) used a nurse in the CM role, and that the intervention group's Montgomery-Asberg Depression Score-Self depression scores were significantly lower than those of the control group at both 3 (−2.17, 95% CI [0.56, 3.79], p = .009) and 6 (−2.27, 95% CI [0.59, 3.95], p = .008) months. Training for their nurse CMs included one 3-day training before the intervention, and two 3-day trainings during the intervention, though specifics of the training were not reviewed (Björkelund et al., 2018). Thota et al. (2012) reviewed 37 randomized control trials for collaborative care through 2004. Studies employed CMs with professional backgrounds as nurses, master's level mental health workers, and social workers (Thota et al., 2012). The effect estimates were largest for registered nurses (Thota et al., 2012). Furthermore, given their background in the medical field, registered nurses are well suited to support patients with complex medical care needs and depression. Nurse CMs can help patients build confidence in themselves for managing long-term conditions and improve patient quality of life (Askerud & Conder, 2017).
Objectives
Although evidence demonstrates that the CCM is effective with nurses in the integrated care CM role, there is a need to review how this intervention is operationalized when caring for patients with depression and a long-term or chronic medical condition in an integrated PC setting. The purpose of this review is to provide readers with a critical review of the evidence for what elements of a collaborative nurse CM role have been be successful in supporting patients with depression and chronic medical illnesses in an integrated PC setting.
Methods
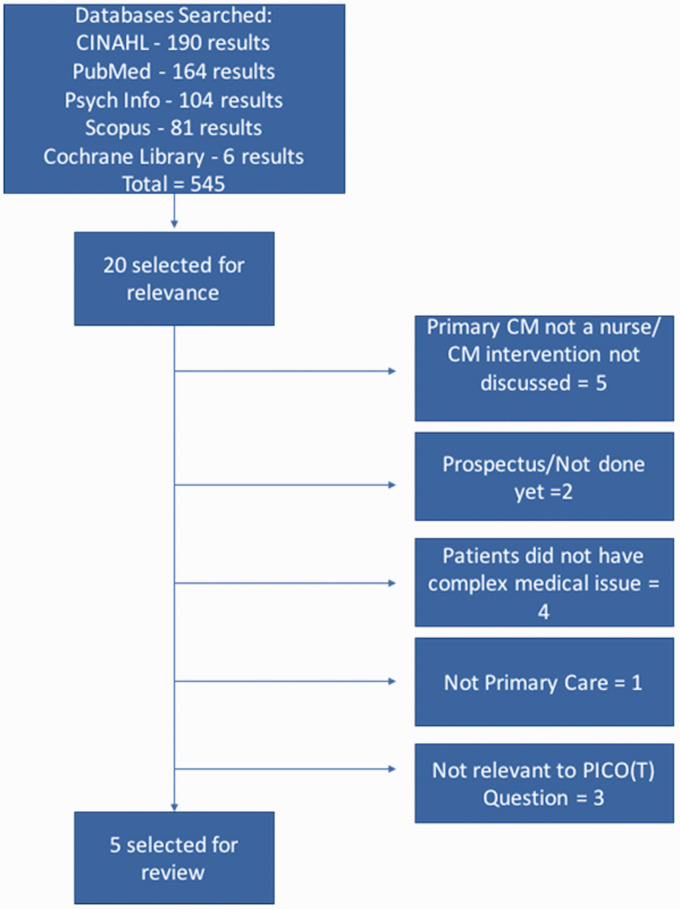
The process used for this evidenced-based search strategy was the PICO(T) format: Patient population; intervention or issue of interest; comparison intervention; outcome; time frame (Melnyk & Fineout-Overholt, 2015). The PICO(T) question that guided the review of the evidence was, “In a collaborative PC setting, what designs for a nurse-led CM intervention have been successful in improving depressive symptoms in adults with depression and a chronic health condition over 3 to 12 months?” In October 2018, the Cumulative Index of Nursing and Allied Health Literature(CINAHL), PubMed, PsychINFO, Scopus, and the Cochrane Library were searched using the following key search terms: collaborative care, care manage*, nurs*, depress*, care, manage*, and primary care. The search of CINAHL yielded 190 results, PubMed yielded 164 results, PsychINFO yielded 104 results, Scopus yielded 81 results, and the Cochrane Library yielded 6 results. Articles were considered if they were published within the last 10 years, were published in English, were based in a PC setting, evaluated depressive symptoms with a validated tool, included patients with a diagnosis of a chronic medical condition in addition to one of depression, and involved a nurse-led CM intervention. Articles that outlined a study prospectus were not included, though their final reports were searched for. Studies also had to clearly define what their nurse CM intervention included and were excluded if they did not. Five articles were selected for appraisal based on relevance to the PICO(T) question and meeting all inclusion criteria (see Figure 1). The Johns Hopkins Research Evidence Appraisal Tool was used to evaluate the selected articles (Dang & Dearholt, 2018). Three of the articles in this review were rated as Level I, Grade A; one was Level I, Grade B; and one was Level II, Grade A (see Table 1).
Figure 1.
Search results. The search was conducted in October 2018, using search terms collaborative care, care manage*, nurs*, depress*, care, manage*, and primary care. CINAHL = Cumulative Index of Nursing and Allied Health Literature; CM = care manager; PICO(T) = Patient population; Intervention; Comparison intervention; Outcome; Time frame (Melnyk & Fineout-Overholt, 2015).
Table 1.
Evidence Table.
| Citation | Study design/ method | Sample/setting | CM design | CM training | Contact with patient | Team interaction | Outcomes | Findings | Appraisal worth to practice |
|---|---|---|---|---|---|---|---|---|---|
| Ekers et al. (2013) | Systematic review with meta-analysis | Randomized-controlled trials, databases searched December 2011–May 2012; All points with primary diagnosis of depression and one or more long-term physical health problem; included 14 studies, 4,440 participants; all treated in outpatient settings (not all integrated and not all primary care) | All studies had to have at least two or more of the following elements in their intervention: -Proactive follow-up of participants -Assess adherence to psychological and pharmacological treatments -Monitor patient progress using validated measure, take action when treatment unsuccessful -Provision of psychological support -Regular communication and supervision with mental health specialist and PCP Psychological support interventions included problem-solving therapy, psychoeducation, behavioral activation, and cognitive behavioral therapy | Length varied. None exceeded 7 days. Only five studies discussed their training in detail. Common components of training included training on monitoring depression, delivering psychological support, and training regarding the physical health issues they would support | Differences between number of clinical contacts—no significantly different outcomes. Ranged from 4 to 12 across studies. Metaregression slope 0.0004 (95% CI [−0.028, 0.029], Qtotal 20.53, p = .08, Qsession number 0.0008, p = .98). | Not discussed | Change in depression symptom level (self-rated or clinician rated) Depression severity, most studies used PHQ-9 | Nurse-led CC intervention helped improve depression symptoms. Mean effect size at follow-up was d = 0.43, 95% CI [0.34, 0.52], p < .001, Number needed to treat = 4.23. However, moderate between-study heterogeneity (I2) 36.68%. No statistically significant difference in outcomes between telephone only and face-to-face intervention, nor with length of contact with nurse, nor with frequency of interactions | Level I, A |
| Johnson et al. (2014) | Pragmatic, controlled implementation trial | Primary care, adults with DM type 2 and depression; Alberta, Canada | Shared care plan with patient and PCP; problem-solving skills for self-management; monitored treatment adherence and outcomes; symptom check-in; progress toward goals//after PHQ < 10, relapse prevention plan and then focused on DM control | Two-day training session, annual booster session, monthly teleconferences with CMs and specialists; training in problem-solving therapy, behavioral activation, motivational interviewing | 1 to 2 times per month; by phone or in-person | Consulted with PCPs, specialists, psychiatrists regarding progress; regular case conferencing | PHQ, Health-related quality-of-life measures included SF-12, 5-level EQ-5D, Problem Areas In Diabetes-5, Patient Assessment of Chronic Illness Care-11, physical health measures | Greater improvements in PHQ scores compared with control (difference of 2.0 (95% CI [0.4, 3.7], p = .015); Clinically important recovery significantly more in intervention compared with active-control (p = .03, 61% to 44%); significantly less improvement in PHQ in nonscreened controls, compared with intervention p < .001 | Level II, A |
| Katon et al. (2010) | Single-blind randomized control trial | Primary care, adults with depression and DM and CHD, Washington state | Goal setting; check-in regarding progress toward clinical and self-care goals; problem-solving; treatment protocols to adjust medications; medication adherence; motivational interviewing and coaching; education; behavioral activation; regular, proactive follow-up with patient; care plan also addressed diet and exercise | Two-day training on depression management, behavioral strategies, glycemic, blood pressure, and lipid control. PCP, nephrology specialist, endocrinologist, psychologist, psychiatrist developed the training | In-person visits every 2 to 3 weeks; once in maintenance maintenance stage, telephone check-in every 4 weeks | PCP, psychiatrist, psychologist | SCL-20 depression, physical health measures, medication adjustments, satisfaction, Patient Global Rating of Improvement for Depression | At 12 months, intervention group at significantly greater overall improvement in HbA1C, LDL cholesterol, systolic blood pressure, SCL-20 (p < .001). Intervention group also had greater satisfaction with care for diabetes, heart disease, or both (p < .001) | Level I, A |
| Lin et al. (2012) | Used Katon et al.'s (2010) study and data; further analyzed patient self-monitoring, medication adherence, and medication adjustments | See Katon et al. (2010) | See Katon et al. (2010) | See Katon et al. (2010) | See Katon et al. (2010) | See Katon et al. (2010) | Self-monitoring and medication adherence = pharmacy data for 12 months before and 12 months after intervention pharmacotherapy adjustments = increase in the number of medications prescribed, change in dosage, or switching meds 12 months of the intervention | High medication compliance in both groups at baseline. This did not increase significantly in the study group compared with control group during the intervention. At 12 months after intervention, average rate of blood pressure self-monitoring in treatment group was 3 × higher than that in control group (3.6 vs. 1.1 days per week; RR = 3.20; p < .001); the average blood glucose monitoring rate was 4.9 days per week, and 3.8 days per week, respectively (RR = 1.28; p = .006). Significantly more medication initiations for those who were not on medications at baseline in intervention versus control | Level I, B |
| Morgan et al. (2013) | Two-arm open random cluster trial with waitlist control of 6 months, followed for 12 months | Primary care, adults with depression and DM2 and CHD, Australia | Shared care plan with patient and PCP; educational resources for self-management; monitored treatment adherence and outcomes; referral follow-up; symptom check-in (PHQ-9); psychotherapy or pharmacotherapy if not improving; goal setting and progress toward goals, problem-solving; lifestyle risk factor review; monitored physical measures; succinct care plan for patients and care team members | Two-day workshop—training on PHQ-9 and on the quality-of-life measures for the SF-36; patient goal setting, behavioral techniques (activation, problem-solving); training on clinical guidelines | Once every 3 months, in-person for 45 minutes | Shared care plan and consulted with PCPs | PHQ-9, SF-36, referrals to mental health and exercise, physical health measures | Improvements in both groups' PHQ-9 scores at 6 months but significantly greater improvements in intervention group compared with control group, F(1, 309) = 6.40, p = .012). Clinically significant improvements in those with moderate-to-severe depression in intervention group at 6 months. Significant improvement in numbers of patients exercising, referred to and attending exercise, and referred to and attending mental health work at 6 and sustained at 12 months in intervention group. The significant improvement in SF-36v2 (mental health and physical health) was observed at 6 months and 12 months in intervention group | Level I, A |
Note. CI = confidence interval; CC = Collaborative Care; CHD = coronary heart disease; CM = care manager; DM = diabetes mellitus; PCP = primary care provider; PHQ-9 = Patient Health Questionnaire-9; SF = Short Form; RR = risk ratio; SCL-20 = Symptom Checklist-20; dx = diagnosis; NNT = number needed to treat; med = medication ; LDL = low-density lipoprotein.
Discussion
Evidence Reviewed
The studies reviewed explored different designs of the CM role (see Table 2). Ekers et al. (2013) conducted a systematic review and meta-analysis of randomized-controlled trials that tested nurse CM interventions in adults at least 16 years of age who had depression as well as a long-term health issue. The effects of nurse CM interventions across 14 randomized-controlled trials and 4,440 participants were analyzed. Studies were included in the review if they provided care with at least two or more of the following components of collaborative care: proactive follow-up of patients, assessment of care plan adherence, monitoring of symptoms with evidence-based tools, care plan or medication adjustment as indicated, psychological support being available, and regular communication between the PCPs and mental health staff. Ekers et al. (2013) found the mean effect size on depression symptoms to be moderate, d = 0.43 (95% CI [0.34, 0.52], p < .001, NNT 4.23). However, not all of the studies reviewed were in a PC setting, and many of these studies are now over 10 years old. Not all of the studies in this review were relevant to answering the question of how a nurse CM intervention should be operationalized and what training elements were required.
Table 2.
Elements of the Nurse CM Intervention.
| CM Intervention elements/characteristics | Ekers et al. (2013) | Johnson et al. (2014) | Katon et al. (2010) | Morgan et al. (2013) |
|---|---|---|---|---|
| Nurse-led | x | x | x | x |
| Follow-up phone visits | x | x | x | |
| In-person follow-up visits | x | x | x | x |
| Behavioral intervention | x | x | x | x |
| Behavioral activation | x | x | x | x |
| Motivational interviewing | ? | x | x | |
| Problem-solving | x | x | x | x |
| Goal setting | ? | x | x | x |
| Self-management skills | ? | x | x | x |
| Patient-centered care plan | x | x | x | x |
| Treatment plan adherence check-in | ? | x | x | x |
| Symptom check-in | x | x | x | x |
| Medication check-in | x | x | x | x |
| CM—care team contact | x | x | x | x |
| Shared care plan | x | x | x | x |
Note. The “?” indicates that it was not explicitly addressed. The “x” indicates that the corresponding CM Intervention elements/characteristics was present in this study. Table structure adapted from Melnyk and Fineout-Overholt (2015). CM = care manager.
Katon et al. (2010) and Morgan et al. (2013) were included in Ekers et al.'s (2013) meta-analysis and were also found in this review's search strategy. These studies both describe their interventions in detail (see Table 1). Katon et al. (2010) conducted a single-blind randomized-controlled trail in 14 integrated PC settings, involving 214 adults with diabetes and coronary heart disease, as well as depression. Their nurse-led intervention in an integrated care setting demonstrated a significant improvement in the physical markers of hemoglobin A1C, low-density lipoprotein cholesterol, systolic blood pressure, and depression, as measured by the Symptom Checklist Depression Scale-20, at 12 months (p < 0.001; Katon et al., 2010). The fact that PCPs cared for both the intervention group and the control group is a limitation, as the increased awareness of mental health issues may have influenced care to the control group (Katon et al., 2010). Lin et al. (2012) did further analysis on Katon et al.'s (2010) data and found that at 12 months after the intervention, those in the intervention group had significantly higher rates of self-monitoring of blood pressure and blood glucose as compared with the control group (RR = 3.20, p < .001; RR = 1.28, p = .006, respectively). They also found that the intervention group had significantly more new medication starts than those in the control group (Lin et al., 2012).
Morgan et al. (2013) conducted a two-arm open random cluster trial with a waitlist control of 6 months, followed for 12 months in Australian PC clinics, in 400 adults with depression and diabetes mellitus type 2, or coronary heart disease. They saw improvements in both groups' PHQ-9 scores at 6 months but significantly greater improvements in the intervention group compared with control group, F(1, 309) = 6.40, p = .012 (Morgan et al., 2013). In those with moderate-to-severe depression, these improvements were clinically significant. They suspect that the control group had improvements in depression symptoms because clinicians were more aware of the comorbidity of depression with diabetes and heart disease, as evidenced by the significant increase in mental health referrals in the control group during the study period (p < .001; Morgan et al., 2013). Furthermore, there were significant improvement in numbers of referrals to and engagement in exercise plans and mental health work in the intervention groups at both 6 and 12 months. Significant improvements in the intervention group's mental health and physical health scores in the Short Form Health Survey-36 version two were observed at 6 months (p = .034, p = .023, respectively; Morgan et al., 2013). Limitations of this study include the fact that they did not comprehensively discuss their other elements of their CCM, and the control group may have been more aware of mental health issues by participating in the study (Morgan et al., 2013).
Johnson et al. (2014) conducted a pragmatic, controlled implementation trial in PC settings in Alberta, Canada, in 157 patients with depression and type 2 diabetes. They found greater improvements in PHQ scores between the intervention group and the control group (difference of 2.0, 95% CI [0.4, 3.7], p = .015; Johnson et al., 2014). There was also a higher percentage of clinically significant improvements in depression symptoms in the intervention group as compared with the active-control group (p = .03) and significantly less improvement in PHQ scores in the nonscreened controls compared with intervention group (p < .001; Johnson et al., 2014). Strengths of this study include their thorough description of their intervention, but one must consider the unique aspects of the Canadian health-care system when considering its applicability to the United States.
Frequency and Modality of Contact With Patients
Differences existed in the frequency, length, and modality of patient and nurse CM contact across the studies. However, Ekers et al. (2013) found in their meta-analysis that while the number of nurse CM visits ranged from 4 to 12 across studies, outcomes were similar. In Johnson et al (2014), nurse CM appointments occurred 1 to 2 times per month, by phone or in-person. Morgan et al. (2013) had nurse CM 45 minutes, in-person visits every 3 months, while Katon et al. (2010) had in-person nurse CM visits every 2 to 3 weeks. Once the patient achieved remission, telephone appointments were done every 4 weeks (Katon et al., 2010). All studies discussed the importance of regular nurse CM follow-up.
Components of CM Intervention
All of the studies reviewed provided some kind of psychological support intervention. Ekers et al. (2013) did not discuss all of the specific psychological support interventions that the included studies used, though they did specifically reference behavioral activation and Problem-Solving Therapy, which are therapies based in Cognitive Behavioral Therapy. Behavioral Activation is a brief psychological support intervention based in which the depressed individual is supported in engaging in activities that once brought them joy (Jacobson et al., 1996; Jacobson, Martell, & Dimidjian, 2001). By doing so, depressive symptoms improve, and the cycle of avoiding pleasurable activities and feeling more depressed is broken. Problem-Solving Therapy is a brief therapy model in which the client's depressive symptoms are improved through guiding them through the process of solving problems (Malouff, Thorsteinsson, & Schutte, 2007). The individual's problem-solving skills and confidence improve in this seven-step therapy model. Johnson et al. (2014), Morgan et al. (2013), and Katon et al. (2010) all had behavioral activation, problem-solving, goal setting, and patient self-management skills in their nurse CM programs. Johnson et al. (2014) and Morgan et al. (2013) also found motivational interviewing to be useful in their interventions. Motivational interviewing is a counseling approach and a way of being with clients that elicits desire for behavior change through nonjudgmentally exploring and resolving ambivalence in the client (Miller & Rollnick, 1991). Psychoeducation is a psychological support intervention that involves educating the client about their psychological illness, treatment options, and prognosis (Zhao, Sampson, Xia, & Jayaram, 2015). Psychoeducation and education regarding self-management were also common components across the four studies.
In these visits, medication follow-up was conducted, and medication was adjusted based on nurse protocol or consultation with the prescribing clinician (Ekers et al., 2013; Johnson et al., 2014; Katon et al., 2010; Morgan et al., 2013). Depressive symptom check-in was in all of the studies' nurse CM designs, and often the PHQ-9 was used to monitor depressive symptoms.
Utilization of a patient-centered care plan was evident across the studies reviewed. Goal setting and following up with patients about progress toward goals was also discussed, and the nurse CM would help the patient identify and overcome barriers to achieving their goals (Johnson et al., 2014; Katon et al., 2010; Morgan et al., 2013). Katon et al. (2010) and Johnson et al. (2014) had the nurse CM develop a relapse prevention plan with patients after they achieved remission of their depression. Morgan et al. (2013) included referral follow-up, lifestyle risk factor review, and monitoring of physical measures in their nurse CM check-ins, while Katon et al. (2010) included diet and exercise components of their care plans. While all studies had the nurse CM check-in and collaborate with other team members regularly, only Johnson et al. (2014) actually shared the care plan itself among team-members and with the patient.
Training of CM
Although Ekers et al. (2013) found variation in length of training to be up to 7 days, Johnson et al. (2014), Morgan et al. (2013), and Katon et al. (2010) all held 2-day training sessions for their nurse CMs. The content of the trainings in the studies reviewed by Ekers et al. (2013) included instruction in behavioral support interventions, administration of the psychological assessment tools, education about depression, and pertinent medical symptoms in their instruction design. The training in Katon et al. (2010) was led by a psychologist, a psychiatrist, PCPs, and a nephrologist and endocrinologist, who specifically spoke about diabetes. The other studies did not discuss who specifically led the training.
Implications for Practice
It is important that the nurse CM intervention be appropriate to the practice setting. The studies reviewed utilized different expectations for frequency, duration, and mode of patient contact. As there was no significant difference in outcomes between telephone or face-to-face patient contact, it would be wise for the practice to design an intervention that is most appropriate to their patient population (Ekers et al., 2013). It may be practical for the nurse CM to have both in-person and telephone contact with patients, as this design is supported by the literature and may be more accessible for patients. Regardless of the modality of communication, the nurse CM should have regular, proactive contact with the patient. The content of these visits should be thoughtfully constructed.
Practices should design their nurse CM visits to include regular follow-up evaluation of depression symptoms, medication adherence, and need for treatment adjustment. Some practices may be ready to have the nurse CM adjust medications based on protocols, while others may want to continue clinician-driven adjustments. Regardless, interdisciplinary collaboration is important in this model. The nurse's interdisciplinary care plan itself may be utilized to help support this collaboration among care providers as well as with the patient (Johnson et al., 2014).
Helping the patient set goals and supporting them in identifying and overcoming barriers to achieving these goals were also common elements in these intervention designs (Ekers et al., 2013; Johnson et al., 2014; Katon et al., 2010; Morgan et al., 2013). Behavioral activation may be included in these goals to help support depression improvement. Education, motivational interviewing, and problem-solving skills can help the patient in achieving their goals.
Training of the nurse CM should be relevant to the elements included in the intervention. Having colleagues from different disciplines in the practice lead the training may be helpful both in educating the nurse CM and also in fostering interdisciplinary relationships, which may lead to better interdisciplinary management of these patients. Training does not have to be extensive, as the studies reviewed only had 2-day trainings, but having continual access to and support from other team members is helpful in this model.
Conclusion
Although there is strong evidence supporting the CCM, and the CM is an essential component of this model, differences exist in CM role implementation. Nurses have been successful as the CM, and having the nursing background may be especially important in supporting patients with complex medical conditions. Furthermore, nurses are trained to see the patient as a whole person, integrating the behavioral, medical, and psychosocial in the patient-centered care plan development. Despite the volume of existing evidence about the CCM, evidence on how to implement a nurse CM intervention in a PC setting with adults with depression and a chronic medical condition remains limited. A review of the existing evidence suggests the importance of regular patient follow-up, goal setting, problem-solving, behavioral activation, treatment plan engagement, symptom identification, and medication adherence in the nurse CM intervention. While there is no standard training requirement for this role, training plans should be designed such that the nurse CM feels equipped to adequately fulfill the care plan elements. Regular contact with other care team members may support the success of this role. Additional research is needed regarding the best way to operationalize the nurse CM role in an integrated care setting and should further explore this role's potential for improving patient outcomes and interdisciplinary care.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- Advancing Integrated Mental Health Solutions Center. (n.d.). Principles of collaborative care. Retrieved from https://aims.uw.edu/collaborative-care/principles-collaborative-care.
- American Psychological Association, & Academy of Psychosomatic Medicine (2016) Dissemination of integrated care within adult primary care settings: The collaborative care model. Retrieved from https://www.integration.samhsa.gov/integrated-care-models/APA-APM-Dissemination-Integrated-Care-Report.pdf. [Google Scholar]
- Archer J., Bower P., Gilbody S., Lovell K., Richards D., Gask L., Coventry P. (2012) Collaborative care for depression and anxiety problems. The Cochrane Database of Systematic Reviews 10: CD006525 doi:10.1002/14651858.CD006525.pub2. [DOI] [PubMed] [Google Scholar]
- Askerud A., Conder J. (2017) Patients' experiences of nurse case management in primary care: A meta-synthesis. Australian Journal of Primary Health 23(5): 420–428. doi:10.1071/PY17040. [DOI] [PubMed] [Google Scholar]
- Björkelund C., Svenningsson I., Hange D., Udo C., Petersson E.-L., Ariai N., Westman J. (2018) Clinical effectiveness of care managers in collaborative care for patients with depression in Swedish primary health care: A pragmatic cluster randomized controlled trial. BMC Family Practice 19: 28 doi:10.1186/s12875-018-0711-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke D. M., Currie K. C. (2009) Depression, anxiety and their relationship with chronic diseases: A review of the epidemiology, risk and treatment evidence. The Medical Journal of Australia 190(7 Suppl): S54–S60. [DOI] [PubMed] [Google Scholar]
- Dang D., Dearholt S. L. (2018) Johns Hopkins nursing evidence-based practice: Model and guidelines, Indianapolis, IN: Sigma Theta Tau International. [Google Scholar]
- Ekers D., Murphy R., Archer J., Ebenezer C., Kemp D., Gilbody S. (2013) Nurse-delivered collaborative care for depression and long-term physical conditions: A systematic review and meta-analysis. Journal of Affective Disorders 149(1–3): 14–22. doi:10.1016/j.jad.2013.02.032. [DOI] [PubMed] [Google Scholar]
- Holt R. I. G., de Groot M., Lucki I., Hunter C. M., Sartorius N., Golden S. H. (2014) NIDDK international conference report on diabetes and depression: Current understanding and future directions. Diabetes Care 37(8): 2067–2077. doi:10.2337/dc13-2134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson N. S., Dobson K. S., Truax P. A., Addis M. E., Koerner K., Gollan J. K., Prince S. E. (1996) A component analysis of cognitive-behavioral treatment for depression. Journal of Consulting and Clinical Psychology 64(2): 295–304. doi:10.1037/0022-006X.64.2.295. [DOI] [PubMed] [Google Scholar]
- Jacobson N. S., Martell C. R., Dimidjian S. (2001) Behavioral activation treatment for depression: Returning to contextual roots. Clinical Psychology: Science and Practice 8(3): 255–270. doi:10.1093/clipsy.8.3.255. [Google Scholar]
- Johnson J. A., Sayah F. A., Wozniak L., Rees S., Soprovich A., Qiu W., Majumdar S. R. (2014) Collaborative care versus screening and follow-up for patients with diabetes and depressive symptoms: Results of a primary care–based comparative effectiveness trial. Diabetes Care 37(12): 3220–3226. doi:10.2337/dc14-1308. [DOI] [PubMed] [Google Scholar]
- Katon W. J., Korff M. V., Lin E., Walker E., Simon G. E., Bush T., Russo J. (1995) Collaborative management to achieve treatment guidelines: Impact on depression in primary care. Journal of the American Medical Association 273(13): 1026–1031. doi:10.1001/jama.1995.03520370068039. [PubMed] [Google Scholar]
- Katon W. J., Lin E. H. B., Von Korff M., Ciechanowski P., Ludman E. J., Young B., McCulloch D. (2010) Collaborative care for patients with depression and chronic illnesses. New England Journal of Medicine 363(27): 2611–2620. doi:10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochanek, K. D., Murphy, S. L., & Tejada-Vera, B. (2016). Deaths: Final data for 2014 (National Vital Statistics Report No. 2016–1120). Retrieved from National Center for Health Statistics website: https://www.cdc.gov/nchs/data/nvsr/nvsr65/nvsr65_04.pdf. [PubMed]
- Lin E. H. B., Von Korff M., Ciechanowski P., Peterson D., Ludman E. J., Rutter C. M., Katon W. J. (2012) Treatment adjustment and medication adherence for complex patients with diabetes, heart disease, and depression: A randomized controlled trial. Annals of Family Medicine 10(1): 6–14. doi:10.1370/afm.1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malouff J., Thorsteinsson E., Schutte N. (2007) The efficacy of problem solving therapy in reducing mental and physical health problems: A meta-analysis. Clinical Psychology Review 27(1): 46–57. doi:10.1016/j.cpr.2005.12.005. [DOI] [PubMed] [Google Scholar]
- Melnyk B. M., Fineout-Overholt E. (2015) Evidence-based practice in nursing & healthcare: A guide to best practice, 3rd ed. South Holland, the Netherlands: Wolters Kluwer. [Google Scholar]
- Miller W., Rollnick S. (1991) Motivational interviewing: Preparing people to change addictive behavior, New York, NY: Guilford Press. [Google Scholar]
- Morgan M. A. J., Coates M. J., Dunbar J. A., Reddy P., Schlicht K., Fuller J. (2013) The TrueBlue model of collaborative care using practice nurses as case managers for depression alongside diabetes or heart disease: A randomised trial. BMJ Open 3(1): e002171 doi:10.1136/bmjopen-2012-002171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naylor C., Parsonage M., Mcdaid D., Knapp M., Fossey M., Galea A. (2012) Long-term conditions and mental health: The cost of co-morbidities. Retrieved from The King's Fund Centre for Mental Health website: https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/long-term-conditions-mental-health-cost-comorbidities-naylor-feb12.pdf. [Google Scholar]
- Richards D. A., Hill J. J., Gask L., Lovell K., Chew-Graham C., Bower P., Barkham M. (2013) Clinical effectiveness of collaborative care for depression in UK primary care (CADET): Cluster randomised controlled trial. British Medical Journal 347: f4913 doi:10.1136/bmj.f4913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rui P., Okeyode T. (2015) National ambulatory medical care survey: 2015 state and national summary tables. Retrieved from https://www.cdc.gov/nchs/data/ahcd/namcs_summary/2015_namcs_web_tables.pdf. [Google Scholar]
- Thota A. B., Sipe T. A., Byard G. J., Zometa C. S., Hahn R. A., McKnight-Eily L. R., Williams S. P. (2012) Collaborative Care to improve the management of depressive disorders. American Journal of Preventive Medicine 42(5): 525–538. doi:10.1016/j.amepre.2012.01.019. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2018, March 22). Depression [Fact sheet]. Retrieved from http://www.who.int/mediacentre/factsheets/fs369/en/.
- Zhao S., Sampson S., Xia J., Jayaram M. B. (2015) Psychoeducation (brief) for people with serious mental illness. The Cochrane Database of Systematic Reviews 4: CD010823 doi:10.1002/14651858.CD010823.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]