Abstract
Objectives
In Sweden, an increasing number of tests for sexually transmitted infections are conducted. Self-sampling services are provided free of charge at the national eHealth website. Our aim was to obtain a deeper understanding of users’ beliefs and experiences of Chlamydia trachomatis (CT) and Neisseria gonorrhoeae (NG) self-sampling services.
Methods
This qualitative study is part of the national project ‘Internet-based chlamydia and gonorrhoea self-sampling test’, conducted in Sweden. Individuals ordering a CT/NG self-sampling test at home from the eHealth website were invited to participate. Of the 114 individuals who agreed, a purposeful sample including 20 women and men aged 18–49 years (mean, 30.8 years) participated in a telephone interview in 2019.
Results
The test service for CT/NG was highly appreciated by men and women of different ages. Round-the-clock accessibility, avoiding clinical visits, ease of use, confidentiality and a rapid test result were reasons for this appreciation. Language, uncertainty about the correct sampling procedure, unreliable postal services and concerns about handling of personal data were mentioned as barriers. Reasons for testing were checking after unprotected sex, symptoms, checking a partner’s fidelity or a regular routine—‘to be on the safe side’. Knowledge about the infections and their consequences was limited; some considered them severe, especially if they could threaten fertility, and others were less concerned. Disclosing an infection was described as emotionally stressful. Participants had high self-efficacy in relation to the test and would not hesitate to use the service again, even if it involved a cost.
Conclusions
Internet-based CT/NG self-sampling at home was highly appreciated and was used for individual health reasons, but also out of concern for others’ health and for society as a whole. The benefits seem to outweigh the barriers, and the service may therefore continue to be widely offered.
Keywords: public health, qualitative research, infectious diseases, sexual medicine, reproductive medicine
Strengths and limitations of this study.
This study is based on a theoretical framework, the Health Belief Model, and aimed to obtain a deeper understanding of users’ beliefs and experiences of Chlamydia trachomatis (CT) and Neisseria gonorrhoeae (NG) self-sampling services.
A strength of this qualitative study is that it forms an integral part of the evaluation of the concept of internet-based self-sampling for CT/NG testing.
We conducted telephone interviews with a purposeful sample of individuals of different sex and sexual identity.
A limitation was that interviewing could only be performed in Swedish and English and did not permit observation of non-verbal communication.
As in all qualitative research, the aim is not to generalise, but the results might be useful in similar settings.
Introduction
From a public health perspective, it is of paramount importance to promote and address sexual and reproductive health because it concerns a large proportion of the population. There is a growing interest in offering gender-sensitive, effective internet-based care options to improve accessibility, equity and cost-effectiveness.1–3 Targeting both women and men at risk of sexually transmitted infections (STIs) may have lifelong importance for the individual and considerable implications for public health.4
One such internet-based initiative is the offer of free-of-charge testing for Chlamydia trachomatis (CT)/Neisseria gonorrhoeae (NG) with self-sampling at home. The service has been tested in some countries as a study project or in routine diagnostics.5–9 In Sweden, it is currently provided by the public healthcare service and is available in all counties through two national e-Health websites.10 Individuals with a confirmed infection are directed to a clinic for free treatment and partner notification.
An earlier Swedish study showed that users were mostly young people with high sexual risk behaviour.11 A recent study found that self-sampling, when compared with clinic-based sampling, comprised 22% of all CT tests in 2017 and accounted for 20% of all detected CT cases.10 The positivity rate was similar to clinic-based testing (5.5% vs 5.1%), as was the proportion of men using the service (33.7% vs 30.8%).
A review of users’ experiences of self-sampling concluded that self-sampling was appreciated by those using it.12 However, the review included only 10 studies with home-based sampling, and none of them was conducted in Sweden. A recent survey among 1785 users of the service in Sweden showed that users were happy with the self-sampling test service, and sexual risk behaviours motivated use of the test.13 Our aim of this qualitative study was to complement those quantitative findings to gain a deeper understanding of users’ beliefs and of their experiences of the home-based self-sampling service currently offered in Sweden.
Methods
Design and setting
The present qualitative interview study is part of the project ‘Internet-based chlamydia and gonorrhoea self-sampling test’, undertaken in Uppsala county, a region with a population of 368 000. The study follows Standards for Reporting Qualitative Research14 and is reported according to the Consolidated Criteria for Reporting Qualitative Research checklist (online supplemental file l).15
bmjopen-2020-041340supp001.pdf (59.8KB, pdf)
Sample and procedure
We used a strategic approach aiming to include a broad sample of users of the self-sampling service. We wanted to explore as many different voices as possible. Eligible participants were individuals aged ≥15 years who had ordered a CT/NG self-sampling test from the national eHealth website.13 They were invited to participate in a telephone interview. Those interested provided their name, address and mobile phone number and completed a consent form online. In all, 114 individuals agreed to participate, and of these, 20 men and women with a wide range of ages and representing different sociodemographic areas (by post code) were included in the study, based on the estimation that we needed about 20 interviews to reach information power (ie, adequate information on the topic).16
The interviews were conducted in 2019, lasted between 30 and 52 min, and were audio-recorded using the application ‘TapeACall Pro’. Each interview started with brief information about the study. The interviews were transcribed verbatim, and no repeat interviews were carried out. The interviewers (MG and ML) are health professionals and PhDs with experience in qualitative methods and the topics in question.
Interview guide
We used a semistructured interview guide, based on a previous study about STIs and sexual health.17 Study-specific questions were constructed based on previous research and a quantitative internet-based questionnaire that is part of this project.13 Two pilot interviews resulted in minor changes to the guide. In summary, the questions focused on the informant’s beliefs and experiences of using the CT/NG self-sampling test, with a special emphasis on chlamydia (table 1).
Table 1.
Interview guide
| Guiding questions for the telephone interview | HBM concept |
| How did you find out about the self-sampling service? | Cues to action |
| What are your views on home-based self-sampling for STIs? | Individual beliefs |
| What are the benefits? | Benefits |
| What are the barriers? | Barriers |
| What do you know about CT/NG? | Knowledge |
| What are the risks with CT/NG? | Knowledge/severity |
| How severe would an infection be for you? | Severity |
| How do you perceive your own risk of CT/NG? | Susceptibility |
| What made you order the test kit now? | Cues to action |
| How did you find using the kit? | Self-efficacy |
| What are your thoughts about the kit in relation to privacy? | Barriers |
| What are your thoughts about the results? | Barriers |
| What do you think about the time from order to result? | Benefits/barriers |
| What do you think about home-based self-sampling in relation to clinical sampling? | Benefits/barriers |
| How often do you consider one should take such a test? | Individual beliefs |
| How much would you be willing to pay for a test if it involved a cost? | Self-efficacy |
| Would you use the service again and/or recommend it to others? | Self-efficacy |
CT, Chlamydia trachomatis; HBM, Health Belief Model; NG, Neisseria gonorrhoeae; STIs, sexually transmitted infections.
Theoretical framework: the Health Belief Model
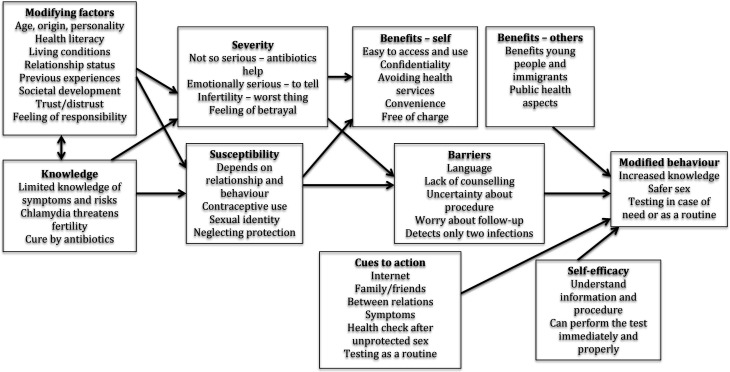
The Health Belief Model (HBM) is useful in understanding the factors that influence the health behaviour.18 The model includes the following central constructs: perceived susceptibility, perceived severity, perceived benefit, perceived barriers and individual behaviour. In addition, sociodemographic factors such as age, sex and ethnicity, and also knowledge, can influence the individual’s behaviour. Important concepts in the theory are cues to action, which can motivate individuals to alter their behaviour, and self-efficacy—the ability of the individual to perform certain behaviour. In addition, the authors suggest a modification of the model to include modified behaviour.
Analysis
We used a deductive approach19 with key concepts from the HBM to analyse and discuss our findings. The transcripts were read to get an overall picture of the data. Units of meaning were extracted, condensed and labelled with a colour mark. These units were then sorted into suitable HBM categories by two researchers working individually. Finally, all the authors discussed the categories until consensus was reached.
Patient and public involvement statement
This study is part of a larger study.10 13 Three university students were engaged in the project design. Furthermore, the questionnaire used in the previous survey13 was tested on two patients in a pilot study, and thereafter the questionnaire was slightly modified. By definition, patients are involved in this interview study. Before commencement, the interview guide was tested on representatives of the public, that is, individuals similar to the target group, resulting in minor changes to the interview guide (table 1).
Results
In total, 11 women and 9 men, aged 18–49 years (mean, 30.8 years), participated. The participants had different sexual identities (heterosexual and homosexual) and diverse countries of birth and cultural backgrounds. The findings are presented according to the HBM concepts and are summarised in figure 1.
Figure 1.
Findings according to the Health Belief Model.
Modifying factors
A plethora of modifying factors seemed to influence the use of the self-sampling test, some personal and others more of a relational or contextual nature.
Individual factors
Individual factors included personality, sexual identity, health awareness and emotions such as shyness and physical discomfort:
I am a bit shy to go to the health center …. [my country] it is a bit different from Sweden. (Woman, #12)
I am not very comfortable with someone else touching my penis. My first thought was: Will this hurt or won’t it? (Man, #2)
Relational factors
Relational factors were sexual behaviour, current relationship status, trust or distrust in one’s partner, and previous experience of infidelity or betrayal:
In many relationships it happens that … you become aware of infidelity because of a positive chlamydia test. (Woman, #7)
Contextual factors
Contextual factors such as country of birth, previous healthcare experiences, economy and encountering unknown sex partners via dating applications were also mentioned:
People who are like newly here, they have maybe like a lot of stigma about sex and stuff like that. So they wouldn’t tell, even to the doctors. From the culture I came from, they are not open about the sexuality. (Man, #15)
Knowledge
Knowledge about the infection
Participants had limited knowledge about chlamydia and were unsure of its consequences. Most stated that CT was a common STI with few or no symptoms but should be reported according to the Diseases Act. They had mostly learnt about CT and STIs online, but also mentioned sexuality education in school. They did not know how the infection could affect health, but believed that if untreated it could threaten fertility. Some stated that they were unsure how CT was transmitted, whether it was transmitted through body fluids, by oral sex or if women have sex with women. There were uncertainties about whether CT was a bacterium and how it was treated:
I don’t know how it would feel if I had it, if you get symptoms, which I don’t think you do. And then I don’t know the consequences. I actually know very little. (Woman, #18)
Knowledge about the testing service
Knowledge about the testing service was mostly adequate and came from different sources—internet, other media, school, friends, healthcare providers and also through their own previous experience:
I know about the procedure, I receive the letter, I know what to do, I send it back. Within a couple of weeks I will know what to do, if I have it or not. (Man, #19)
I have never heard any of my male friends saying that they have ordered it (the test kit). (Man, #6)
Severity
Emotional severity
Most participants expressed that a chlamydia infection would be serious, especially for emotional reasons. They would feel guilty and that they were betraying others. Compulsory contact tracing was demanding. The entire procedure was cumbersome, the worst part being disclosing a chlamydia infection to previous and/or current partners. Others were less bothered. They just needed antibiotic treatment and then everything would be OK:
I would find it hard, but not the end of the world. You don’t die from it. The worst part would be disappointing people … that you have caused harm to someone. (Woman, #1)
Physical severity
The participants considered that fertility was important and that infertility would be the worst thing that could happen to them:
It becomes an existential issue, because what meaning is there then to life? (in case of infertility) So it goes deep. (Man, #10)
I really, really want to have children. So, even if … because I am in a same-sex relationship, which makes it even harder. But still, it is very, very important for me to be able to have a child. (Man, #10)
Societal severity
Several participants voiced concerns about a spread of infections in society. CT was perceived as increasing, and risk-taking without condom use often in combination with alcohol consumption was considered common. The fact that the Communicable Diseases Act includes these infections was a sign that society takes them seriously, and the compulsory registration of cases was appreciated as a means of preventing spread of infections in the population:
I think it (the registration of cases) is good … It is still a disease than can influence and damage for a long time. (Man, #9)
Susceptibility
Participants had different perceptions of their own risk of contracting chlamydia. Some believed the risk was low because they had a long-term relationship with one partner or claimed that they chose their sexual partners with care. Others stated that their risk was significant because they were sexually active with different partners without condom protection and/or said that you could never know who to trust. They considered that condom use was cumbersome and that sex was better without it:
I divorced four years ago. Before that I had a steady partner for 16 years. So then I did not think about it at all. But now, when I have been single, I have dated quite a lot and mostly had unprotected sex. (Man, #17)
Benefits
Benefits—self
Participants found it convenient to test the kit online and considered it easy to use. Being able to perform the test at home at a time of one’s choosing was appreciated. Some described the advantage of not having to visit a health service clinic when living in a small community where it was difficult to maintain confidentiality. Avoiding showing one’s genitals to a health professional was also mentioned. The test being free of charge was another benefit. The packaging was discreet and did not disclose that the contents had to do with an STI. Participants felt that they received the result reasonably fast and that it was easy to check for it online:
The instructions were clear, you just follow the steps. You can do it any time, when you want. You do not need to go somewhere or stay away from work … or talk to somebody. You do not need to feel … embarrassed. (Woman, #4)
Benefits—others
Participants described several benefits for other people. Young people and immigrants were seen as more vulnerable and could benefit from the free, confidential service. A public health aspect was also mentioned. An easy-to-use self-sampling service could increase the number of tests and enable contact tracing and treatment, thus avoiding the spread of the infection in society. Some participants had used the home sampling service several times and argued it should be used every time after unprotected sex to protect not only themselves but also others:
Everybody should be able to take a test, without having to consider the cost … the possibility to protect oneself—and to protect against carrying around a disease. (Woman, #6)
Perceived barriers
Although most participants felt confident in the use of the sampling test, some barriers were mentioned, some personal and others more of a technical nature or related to a possible unmet care need.
Personal barriers
Language could be an obvious one, and one participant actually went to a health service clinic to have the procedure explained:
If you have problems with reading and low level of school education. (Woman, #12)
Technical barriers
Not knowing whether they were performing the self-sampling correctly or whether the test would be handled properly caused some worries, as did unreliable postal services and insecure storing of personal data. Some would have liked an extra swab in the kit in case of a mistake:
Maybe it is not 100% reliable? I may not do it the right way … you can be unsure whether the test could end up in the hands of someone unauthorised … it is still personal data. Those are the things you discuss. (Woman, #7)
Unmet care need
Participants expressed that not having the possibility of counselling could be a disadvantage. They also mentioned that they did not know exactly where to turn in case of an infection. Another disadvantage was that the test only covers two infections, chlamydia and gonorrhoea:
Could maybe be problematic that you are not automatically connected to any clinic. (Woman, #1)
Questions may have needed to be asked both from my side and from yours. A broader spectrum of diseases would perhaps be needed. (Man, #17)
Self-efficacy
Self-efficacy in handling the test and obtaining the result
Most participants described had high self-efficacy in their use of the service. They felt confident about taking the sample and sending it by post to the laboratory. However, some disclosed uncertainty in handling the procedure, some had not sent the test and one informant had dropped the swab on the floor. Participants believed they were able to take the test earlier via the self-sampling service compared with visiting a clinic, and most were prepared to use it again. Even if self-sampling overall was considered convenient, waiting for the test result was stressful:
It is not difficult, with the swab … how to place it and how to send it in. You just read, point by point how to do it. (Woman, #16)
I simply forgot, it just lay there in the envelope. So, you have no one to check that it really is done. (Man, #9)
Self-efficacy in relation to a potential cost
Most would be willing to pay for the test; about €10–€30 was considered appropriate. However, a charge would probably lead to fewer tests:
… even if it involved a cost, let us say 100 to 200 Swedish crowns, I would still order the test because the service is so easy and convenient. (Man, #5)
Cues to action
Participants mentioned different aspects that had served as cues to action for them.
Awareness of the availability of the service
The participants expressed that they were aware of the self-sampling test by chance when web surfing on the internet or when visiting health-related websites. Others had become aware of the self-sampling service either from friends or from healthcare providers:
It was on the national e-health web site. I had logged in to book another appointment and then I read about the home test. So I just ‘Ah that sounds good’. (Man, #10)
Health-related reasons
Many took the test to ensure that they were healthy after unprotected sex. Some had also experienced symptoms. Others had made it a routine to take a test regularly—‘to be on the safe side’. Several emphasised the importance of avoiding spreading an infection to others:
… and it is so severe that you should absolutely not spread it on, or hide it to someone. (Man, #9)
Relational aspects
Another reason to take a test was to exclude a potential infection before engaging in a new relationship. Checking whether a partner had been unfaithful was also mentioned; a positive chlamydia test would be seen as a proof of unfaithfulness:
I had left a long relationship and had a new partner. So I wanted to be 100% sure, as I had been earlier. (Woman, #7)
Modified behaviour
Modified sexual behaviour
The participants discussed whether the home-based self-sampling method could lead to modified sexual behaviour. Some said they had learnt a lot and/or become worried and were motivated to use a condom more frequently, whereas others did not have any intention to change. The fact that the test was free of charge, in contrast to condoms, led some participants to argue in favour of a moderate charge so that testing would not replace condom use:
Now I’m into protecting myself a bit better as long as I don’t have a stable partner. The day after (a negative test result) I took cookies to school and we celebrated. Lesson learned, you could say. (Woman, #1)
Modified testing routines
Most participants would use the service again, either as their normal routine or in case of future need:
I have started to think about testing for HIV too, even if it is not that widespread, but still … This has been an eye-opener for me, you could say, and it never hurts to take a test. (Man, #11)
Discussion
The free-of-charge self-sampling test service for CT/NG was highly appreciated by the participants owing to its high accessibility, ease of use, confidentiality, convenience and a rapid result. Barriers included language, uncertainty about the procedure, unreliable postal services and insecure handling of personal data. Checking after unprotected sex or a regular routine—‘to be on the safe side’—was the key reason for ordering the test.
A strength of this qualitative study is that it forms an integral part of the evaluation of the concept of internet-based self-sampling for CT/NG testing. This study is part of a larger project with access to a population with recent experience of the internet-based self-sampling service.13 Thus, we could use a strategic sample of individuals. Our previous work showed this service to be widely used and to play an important role in CT/NG detection,10 and an internet-based questionnaire showed that users greatly appreciate the service and that their behaviour indicates that they are at risk of STIs.13 The criteria for assessing trustworthiness were considered. Credibility was achieved by purposeful sampling of informants, continuous analysis of the data, description of the entire process and supporting quotes. To avoid lone researcher bias, two authors individually read the transcripts and sorted the data into categories. To increase dependability, the analytical process was rigorous and systematic; all data were thoroughly analysed.
A limitation, as in all qualitative research where the aim is not to generalise, is that the results may not be transferable to other settings or societies different from Sweden. Another limitation was that telephone interviewing could only be performed in Swedish and English and did not permit observation of non-verbal communication.
We found the HBM useful in all phases of the project—in developing the interview guide as well as in the analysis and interpretation of the data. However, using HBM both as a guide in designing the study and as an analytical tool may entail a risk for circular reasoning and not being open to unexpected findings. Below we discuss the findings according to this model and in relation to other studies.
Several individual factors and personal knowledge about the infection seemed to influence the decision to use the self-sampling service. This has also been shown in other studies.20–22 The participants discussed perceived threat, the combination of beliefs about severity and susceptibility, with infertility and emotional distress being particularly prominent. This is in agreement with other studies.23 24 If the threat is perceived as significant, willingness to act on it increases.
Our study also showed that users reflect on benefits and barriers in relation to the service. Interestingly, the benefits mentioned were not only for oneself but also for others and for society as a whole. This finding is in contrast to another Swedish study, which showed that young men who took a chlamydia test were not particularly concerned about passing on the infection to others.25 The barriers mentioned by our participants are in line with what other studies have shown.12 26 The HBM postulates that a certain behaviour is more likely to occur if the benefits outweigh the barriers.18 It is therefore important to remove as many barriers as possible. Translation of the information into other languages could be one obvious improvement. However, closing the gap in health inequality due to lower socioeconomics and illiteracy is more challenging. Health literacy, the degree to which individuals have the capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions including risk perceptions, has an impact. Even if health information is available in different languages, individuals might have difficulties to understand and appraise the health service offered. Consequently, the national eHealth service may not reach the population at large. It is essential to reach out to vulnerable groups and provide health information through different arenas and sources including face-to-face information on school health, at youth health clinics and in the primary care setting. We believe that free-of-charge self-tests have the potential to reach individuals of different socioeconomic status in rural areas and in the end, decrease health inequity in Sweden.
Our participants had often learnt about the service through the internet, by actively searching for information, but also unintentionally. Friends were also mentioned, in line with other studies that show that individuals tend to put considerable trust in friends.27 28 Most participants had high self-efficacy in their use of the service, even if they had some doubts about where to turn in the event of a positive test result. A study from the USA showed that most people were in favour of receiving a test result online,29 and another US study concluded that introducing a home-based self-sampling service would be appreciated.30
Some of our participants described the testing procedure as an eye-opener and intended to protect themselves better in the future, whereas others said they would continue to rely on regular testing as a routine. Findings from a large trial in the Netherlands indicate that sexual behaviour can change in two ways after internet-based testing. Those with a positive test result seemed to become more cautious, in contrast to those who had a negative test result, who tended to adopt riskier behaviour.31 These findings are intriguing and would need to be confirmed in further studies. It is also important to note that the findings presented here are opinions and experiences of the users of the self-sampling service. There is thus a need for similar research among people who have chosen not to use an online service and explore their views as well.
In summary, CT/NG infection was considered severe if it could lead to infertility. The test was mainly taken as an individual health check after unprotected sex, but also out of concern for others’ health and for society overall, to avoid spreading an infection. The benefits of the self-sampling test service outweighed the barriers, owing to its high accessibility, ease of use, confidentiality, convenience and a rapid result, and the service may therefore continue to be widely offered.
Supplementary Material
Acknowledgments
We would like to thank all the individuals who participated in the study.
Footnotes
Correction notice: This article has been corrected since it first published. The provenance and peer review statement has been included.
Contributors: MG, ML and BH designed the study; BH was responsible for data collection; and MG and ML conducted interviews, carried out the analysis and composed the initial manuscript. All authors contributed to the finalisation of the manuscript.
Funding: The study was funded by the Public Health Agency of Sweden in 2018; no specific funding number is available. The funders of the study had no role in study design, data collection, data analysis, data interpretation or the writing of the report.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study was approved by the Swedish Ethical Review Authority (Dnr. 2018/250). All participants received written information and provided consent online.
References
- 1.Minichiello V, Rahman S, Dune T, et al. E-health: potential benefits and challenges in providing and accessing sexual health services. BMC Public Health 2013;13:790. 10.1186/1471-2458-13-790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Burns K, Keating P, Free C. A systematic review of randomised control trials of sexual health interventions delivered by mobile technologies. BMC Public Health 2016;16:778. 10.1186/s12889-016-3408-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Woodhall SC, Sile B, Talebi A, et al. Internet testing for Chlamydia trachomatis in England, 2006 to 2010. BMC Public Health 2012;12:1095. 10.1186/1471-2458-12-1095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO . Global health sector strategy on sexually transmitted infections, 2016–2021. Geneva: World Health Organization, 2016. http://www.who.int/reproductivehealth/publications/rtis/ghss-stis/en/ [Google Scholar]
- 5.Ostergaard L, Møller JK, Andersen B, et al. Diagnosis of urogenital Chlamydia trachomatis infection in women based on mailed samples obtained at home: multipractice comparative study. BMJ 1996;313:1186–9. 10.1136/bmj.313.7066.1186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Novak DP, Karlsson RB. Simplifying chlamydia testing: an innovative Chlamydia trachomatis testing approach using the internet and a home sampling strategy: population based study. Sex Transm Infect 2006;82:142–7. 10.1136/sti.2005.016832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fajardo-Bernal L, Aponte-Gonzalez J, Vigil P, et al. Home-based versus clinic-based specimen collection in the management of Chlamydia trachomatis and Neisseria gonorrhoeae infections. Cochrane Database Syst Rev 2015;316:CD011317. 10.1002/14651858.CD011317.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Chlamydia Screening Programme (NCSP) . Information, data, guidance and resources about the NCSP. Available: www.gov.uk/government/collections/nationalchlamydia-screening-programme-ncsp [Accessed 14 Apr 2020].
- 9.Queensland Government Home Sexual Health . Available: https://www.qld.gov.au/health/staying-healthy/sexual-health/chlamydia-test [Accessed 14 Apr 2020].
- 10.Söderqvist J, Gullsby K, Stark L, et al. Internet-based self-sampling for Chlamydia trachomatis testing: a national evaluation in Sweden. Sex Transm Infect 2020;96:160–5. 10.1136/sextrans-2019-054256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Novak D, Novak M. Use of the Internet for home testing for Chlamydia trachomatis in Sweden: who are the users? Int J STD AIDS 2012;23:83–7. 10.1258/ijsa.2011.011030 [DOI] [PubMed] [Google Scholar]
- 12.Paudyal P, Llewellyn C, Lau J, et al. Obtaining self-samples to diagnose curable sexually transmitted infections: a systematic review of patients’ experiences. PLoS One 2015;10:e0124310. 10.1371/journal.pone.0124310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grandahl M, Mohammad J, Larsson M, et al. Users’ opinions of internet-based self-sampling tests for Chlamydia trachomatis and Neisseria gonorrhoeae in Sweden. Acta Derm Venereol 2020;100:adv00315. 10.2340/00015555-3677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O'Brien BC, Harris IB, Beckman TJ, et al. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med 2014;89:1245–51. 10.1097/ACM.0000000000000388 [DOI] [PubMed] [Google Scholar]
- 15.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–57. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 16.Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res 2016;26:1753–60. 10.1177/1049732315617444 [DOI] [PubMed] [Google Scholar]
- 17.Grandahl M, Nevéus T, Dalianis T, et al. ‘I also want to be vaccinated!’ - adolescent boys’ awareness and thoughts, perceived benefits, information sources, and intention to be vaccinated against Human papillomavirus (HPV). Hum Vaccin Immunother 2019;15:1794–802. 10.1080/21645515.2018.1551670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Champion VL, Skinner Sugg C. The health belief model. In: Glantz K, Rimer B, Viswanath K, eds. Health behavior and health education: theory, research and practice. 4th edn. San Francisco: Jossey-Bass, 2008. [Google Scholar]
- 19.Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs 2008;62:107–15. 10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- 20.Op de Coul EL, Götz HM, van Bergen JE. Who participates in the Dutch chlamydia screening? A study on demographic and behavioral correlates of participation and positivity. BMC Public Health 2006;1:221. [DOI] [PubMed] [Google Scholar]
- 21.Barnard S, Free C, Bakolis I, et al. Comparing the characteristics of users of an online service for STI self-sampling with clinic service users: a cross-sectional analysis. Sex Transm Infect 2018;94:377–83. 10.1136/sextrans-2017-053302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Balfe M, Brugha R, O'Connell E, et al. Men’s attitudes towards chlamydia screening: a narrative review. Sex Health 2012;9:120–30. 10.1071/SH10094 [DOI] [PubMed] [Google Scholar]
- 23.Pavlin NL, Gunn JM, Parker R, et al. Implementing chlamydia screening: what do women think? A systematic review of the literature. BMC Public Health 2006;6:221. 10.1186/1471-2458-6-221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Duncan B, Hart G, Scoular A, et al. Qualitative analysis of psychosocial impact of diagnosis of Chlamydia trachomatis: implications for screening. BMJ 2001;322:195–9. 10.1136/bmj.322.7280.195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ekstrand M, Tydén T, Larsson M. Exposing oneself and one’s partner to sexual risk-taking as perceived by young Swedish men who requested a Chlamydia test. Eur J Contracept Reprod Health Care 2011;16:100–7. 10.3109/13625187.2010.549253 [DOI] [PubMed] [Google Scholar]
- 26.Lorimer K, McDaid L. Young men's views toward the barriers and facilitators of internet-based Chlamydia trachomatis screening: qualitative study. J Med Internet Res 2013;15:e265. 10.2196/jmir.2628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Niu Z, Jeong DC, Willoughby JF. Friends over doctors? The influences of source and perceived customization on College drinking. Health Commun 2020;39:1–11. 10.1080/10410236.2020.1712034 [DOI] [PubMed] [Google Scholar]
- 28.Hendry NA, Brown G, Dowsett GW, et al. Association between sexually transmissible infection testing, numbers of partners and talking to partners and friends about sexual health: survey of young adults. Sex Health 2017;14:378–82. 10.1071/SH16076 [DOI] [PubMed] [Google Scholar]
- 29.Gibbs J, Aicken CRH, Sutcliffe LJ, et al. Mixed-methods evaluation of a novel online STI results service. Sex Transm Infect 2018;94:622–4. 10.1136/sextrans-2017-053318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pearson WS, Kreisel K, Peterman TA, et al. Improving STD service delivery: would American patients and providers use self-tests for gonorrhea and Chlamydia? Prev Med 2018;115:26–30. 10.1016/j.ypmed.2018.08.007 [DOI] [PubMed] [Google Scholar]
- 31.Soetens LC, van Benthem BHB, Op de Coul ELM. Chlamydia test results were associated with sexual risk behavior change among participants of the Chlamydia screening implementation in the Netherlands. Sex Transm Dis 2015;42:109–14. 10.1097/OLQ.0000000000000234 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-041340supp001.pdf (59.8KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.