Abstract
Background
To describe the design, implementation, and evaluation of a nurse-led intravitreal injection (NL-IVT) programme in a Singapore tertiary eye hospital.
Methods
Patients requiring anti-vascular endothelial growth factor (VEGF) IVT were recruited. Implementation and evaluation were done in the Singapore National Eye Centre, a tertiary centre. To assess safety, nurse injectors recorded details of procedures performed and complications for an 8-month period from February 2019. To evaluate patient experience, we used a modified patient questionnaire and recorded both patients’ waiting time and IVT procedure duration. A retrospective audit of IVTs before and after the introduction of NL-IVT was performed from January 2017 to September 2019. Cost difference between NL-IVT and standard doctor-led (DL) IVT was evaluated.
Results
A total of 8599 NL-IVTs were performed. No cases of severe complication were detected in the follow-up. A total of 135 patients who received NL-IVT and DL-IVT were surveyed. General satisfaction, interpersonal manner, financial aspect, time spent with injector, and staff competence were higher in NL-IVTs than in DL-IVTs (p < 0.05). There were no differences in terms of technical quality and communication. For 934 patients, waiting time was significantly shorter in NL-IVT (3.6 ± 10.3 min) compared with DL-IVTs (35.3 ± 32.3 min); on average, 19.7 min were saved through NL-IVT (p < 0.01). The cost difference per IVT between NL-IVT and DL-IVT is estimated at 286 SGD (163 GBP).
Conclusion
With a well-designed training programme, NL-IVT is a safe, acceptable, and cost savings procedure. With increasing demand for IVT, NL-IVT provides an alternative model of care for healthcare systems globally.
Subject terms: Health services, Education
Introduction
With ageing populations and increasing incidence of diabetes, age-related macular degeneration (AMD) and diabetic macular oedema (DMO) remain the leading causes of vision loss globally [1–3] For AMD, DMO, and other retinal diseases such as retinal vein occlusion (RVO) or choroidal neovascularization, intravitreal injection therapy (IVT) with anti-vascular endothelial growth factor (VEGF) agents has been the mainstay of treatment for the past decade [1].
However, the enormous resources, costs and efforts of sustainable IVT treatment have placed a tremendous burden on patients and healthcare systems [4]. The majority of patients have an intensive follow-up and injection regime at four or six weekly intervals in alignment with current therapeutic concepts [5, 6]. This has resulted in significant public health challenges to ensure accessibility and timely availability of IVT treatment for patients. In many countries and in remote locations without sufficient ophthalmologists, the accessibility of IVT therapy is questionable. Partly as a result of this, real-life outcomes of IVT treatment deviate drastically from the level of benefit suggested by landmark clinical trials [5, 7, 8].
In many countries, IVT with anti-VEGF agents is currently administered by an ophthalmologist. However, there is a need to expand this service because of increasing load of AMD, DMO, and RVO [3, 9, 10]. Multidisciplinary team approaches may be used to cope with increasing treatment burden, and it has been suggested safe for appropriately trained, non-medical healthcare professionals to administer IVT. This is in line with evolving landscape such that traditional nursing work has also changed in recent years with the introduction of extended roles in many surgical specialties [11].
Nurse-led IVT (NL-IVT) was introduced in the UK, and now appears safe and acceptable to patients across many institutions there [12–14]. It has proven to be an effective means to increase IVT capacity in many retina clinics. Numerous healthcare providers and patients already accept this non-physician NL-IVT service in the clinical environment [15–21].
However, outside of UK, Finland, and a small number of countries, few countries have explored setting up sustainable NL-IVT programs (Supplementary material 1) [5, 12, 20, 22, 23]. In Asia, where the traditional roles of the physician and nurse are well demarcated and patients may prefer treatment by physicians, we are not aware of any NL-IVT programme outside Singapore. The purpose of this paper is to describe the design, implementation, and evaluation of an NL-IVT programme in a large, busy retina service in a major tertiary eye hospital in Singapore.
Methods
Design and setting
IVT training, implementation, and data acquisition were done in the Singapore National Eye Centre (SNEC). SNEC is the largest, tertiary national eye centre in Singapore, managing more than half of outpatient eye consults and surgeries in the country [24, 25].
Clinical governance
A comprehensive policy and procedure document was produced including a stipulation that there will be a continuous audit of each nurse’s complications. Consultant ophthalmologists would retain clinical responsibility for the patient. NL-injections were initially supervised, and then allowed to run independently but parallel to an ophthalmologist-led clinic so that a doctor is present if adverse events occur.
Training
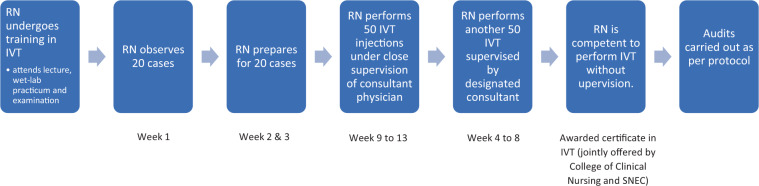
A rigorous training programme was developed for nurses (Fig. 1). This must be completed before being allowed to administer IVT injections. The programme designed includes 4-h of classroom lecture describing IVT indications (Supplementary materials 2 and 3), 4-h of wet-lab practice, 4-h observation of doctor-led (DL) IVTs (DL-IVT), and preparation for 20 patients’ IVT. During the wet-lab training, each trainee was provided with a disposable workstation consisting of an instrument pack, gloves, apron, and a fresh pig eye. The procedure was demonstrated to the trainees, who subsequently performed the procedure on their allocated pig eye. This allowed them to identify the injection location and practice the injection technique. Once comfortable, the nurses underwent step by step supervision and observation by a consultant retina specialist doing the actual procedure administered on a patient. After completing 100 supervised procedures, nurses underwent a competency assessment. Patients were fully informed and consented before a nurse performed the procedure. Regular teaching and professional development sessions were organized to support nurses undertaking this extended role.
Fig. 1. Training process for nurse-led intravitreal injection.
RN = nurse.
Procedure
Patients were given an IVT pamphlet and watched an IVT video before the procedure was administered.
Injection technique
The injection technique is standardised amongst doctors and nurses in our centre.
Before the procedure, patient’s consent and type of IVT were confirmed with medical records. The eye receiving the IVT is marked with a right/left sticker. The patient’s eyelid and eye are assessed to determine if they are safe to administer IVT. The IOP is checked with non-contact tonometry prior to the injection. Once the initial checks are performed, the ocular surface is prepared with 1–2 minims of tetracaine 1% and 1 minim of povidone iodine 5% to the conjunctival fornix. Two cycles of tetracaine and povidone iodine are administered 5 min apart. Patients with iodine allergy received gutt tobramycin 0.3% instead.
A time out is held before the injection. A speculum is inserted and a patient is instructed to look away from the site of injection. An additional nurse will assist by providing a point of fixation and reassurance. The location of the injection is inferotemporal or superotemporal, away from the lid margin and away from large vessels. The site is then marked with a caliper, with 4 mm from the limbus for phakic eyes and 3.5 mm from the limbus for pseudophakic eyes. A 30 gauge needle is directed perpendicular to the globe and aimed at the centre of the vitreous cavity. The medication is then injected into the vitreous cavity.
The needle is withdrawn carefully to avoid reflux and subconjunctival haemorrhage. The patient’s vision is checked for ability to count fingers immediately after the procedure. The IOP is not checked formally post procedure. The patient is then assessed for eye pain, non-threatening and threatening eye complications, and if required referred to an ophthalmologist immediately. The patient is counselled for potential complications they may encounter and nurses document the procedure at the end.
Planning and implementation
After consultation with senior nursing staff, it was felt appropriate that only nurses with a university degree perform this extended role. A named retina specialist was allocated for each nurse trainee. A pilot initiative was instigated and after a successful trial, the service was expanded over a year. Since February 1, 2019, nurses performed majority of IVTs at SNEC.
Outcome measures
Safety
Each nurse recorded details during each IVT administration for 8 months from February 1, 2019, and recorded it in our electronic medical records. Injections were recorded as eventful if any non-visual threatening complications occurred, and adverse if there were vision threatening complications. Presence of any non-visual threatening complications recorded are presence of intravitreal air, subconjunctival haemorrhage, or corneal abrasion. Any vision threatening complications include endophthalmitis, retinal detachment, lens damage, loss of central artery perfusion, uveitis, or vitreous haemorrhage.
Patient experience—waiting time
Informed consent was obtained from all subjects involved in the study. We evaluated the patients’ waiting time and procedure time by extracting data from the local Health Information System. A total of 934 patients were analysed—the group comprised of 467 patients who received NL-IVTs between February 1, 2019, and February 24, 2019, and a random selection of 467 patients who received DL-IVT in 2018.
Patient experience—patient satisfaction
Four months after the initiation of NL-IVT, we began to survey 135 patients while they were waiting for their injection. Patients were surveyed at random. A modified patient questionnaire was formulated (Supplementary material 4) based on the patient satisfaction questionnaire short form and administered to 135 patients [26]. In this questionnaire, seven elements of patient satisfaction were examined: general satisfaction, quality, interpersonal manner, financial aspects, information/communication, time spent with the doctor, and staff competence. All patients have previous IVT administered by both nurse and doctor. Patients who received IVT only by a doctor or a nurse were excluded from the study. Patients were not preselected for survey. Our survey was administered in dedicated IVT clinics. The survey was administered after patients received nurse-led injections for the first time and before if patients have already undergone both doctor and nurse-led injections in prior visits.
Number of injections before and after initiation of the nurse injector programme
To assess the impact of the nurse injector programme, the number of monthly IVTs before and after the introduction of four nurse injectors at the SNEC were evaluated. Monthly number of IVTs from January 2017 to September 2019 were calculated and used for comparison.
Impact of NL-IVT on cost
We aim to explore differences in cost between NL and DL-IVT. We evaluated the total cost of injection and delved into the cost per minute of the procedural time. Indirect costs of patients were omitted because there is heterogenicity in personal backgrounds and comorbidities. Quantifying this would prove to be challenging. A detailed cost analysis is not provided because of information sensitivity. We present the total cost difference per injection. (For review, we provided a reviewer only material in Supplementary document 2.) The monthly IVTs in 2018 were used for projection, and it was assumed that SNEC accounted for 70% of Singapore’s total medical care in ophthalmology.
Statistical analysis
Descriptive statistics were provided. Target sample size was calculated for survey. A total of 128 patients were required to achieve a power of 80% and a level of significance of 5%, for detecting a mean of the differences of 0.2 between doctor and nurse, assuming the standard deviation (SD) of the differences to be 0.8 based on our preliminary survey. Paired t test was used for estimation of patient’s satisfaction, and a histogram is displayed for time comparison. P value of <0.05 was considered statistically significant. Analyses were performed with Stata/MP version 14.0 (StataCorp, College Station, TX, USA).
Results
Safety
A total of 8599 injections were performed by nurses between February 1 and September 31 in 2019. Non-vision threatening complications like subconjunctival haemorrhage occurred in 4%, intravitreal air injections occurred in 0.55%, and one cornea abrasion occurred during study period. For adverse events, there were two patients who were unable to perceive light or hand movement post procedure. Both patients were examined by a consultant physician immediately. One had a normal eye exam, while the other had an intraocular pressure of 39 post procedure. As the patient was unable to see out of the injected eye, a decision was made to perform immediate anterior chamber paracentesis. The patient’s vision recovered after. There were no recorded cases of any endophthalmitis, retinal detachment, lens damage, loss of central artery perfusion, uveitis, or vitreous haemorrhage.
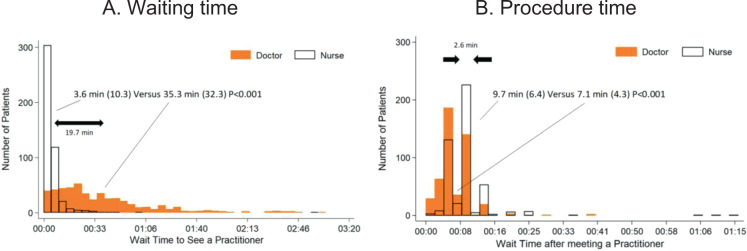
Patient experience—waiting time
A total of 934 participants’ waiting and procedure time were recorded and compared. In Fig. 2, waiting time is significantly shorter in NL-IVT (3.6 ± 10.3 min) compared with waiting time in DL-IVT (35.3 ± 32.3 min). A significantly wide SD in DL-IVT was observed. On average, 19.7 min were saved through the NL-IVT (P < 0.001). More specifically, 1 (0.2%) patient and 78 (16.7%) patients waited for more than an hour in the NL and DL-IVT, respectively. In total, 1 (0.2%) case in NL-IVT and 16 (3.4%) cases in DL-IVT waited for more than 2 h. The NL-IVTs (9.7 ± 6.4 min) took longer than the DL-IVTs (7.1 ± 4.3 min, P < 0.001). The average procedure time difference was 2.6 min (Fig. 2).
Fig. 2. The wait time for nurses was shorter and more uniform than the wait time for doctors, which varied widely.
Nurses took longer than doctors to administer the procedure, presumably due to the preparation performed by the nurses for the doctors to administer the injection, rather than technical proficiency.
Patient experience—patient satisfaction
Table 1 shows the characteristics of 135 patients in the study population. Mean age was 67.6 ± 10.3 years, and 59.3% (n = 80) were female. Patients were classified into the number of IVTs received, mainly less than five times (n = 32, 23.7%), six to ten times (n = 51, 37.8%), and ≥11 IVTs (n = 52, 38.5%). Fear of IVT was reported in 40% (n = 54).
Table 1.
Demographics of the study population (n = 135).
| Variables | Value |
|---|---|
| Age, mean (standard deviation) | 67.6 (10.5) |
| Gender (female), n (%) | 80 (59.3) |
| Race | |
| Chinese, n (%) | 84 (62.2) |
| Malay, n (%) | 27 (20) |
| Indian, n (%) | 20 (14.8) |
| Other, n (%) | 4 (3) |
| No. of injections | |
| 1–5, n (%) | 32 (23.7) |
| 6–10, n (%) | 51 (37.8) |
| ≥11, n (%) | 52 (38.5) |
| Fear of IVT (yes), n (%) | 54 (40) |
| Diagnosis | |
| AMD, n (%) | 53 (39.3) |
| DME, n (%) | 66 (48.9) |
| Other, n (%) | 16 (11.9) |
Table 2 provides the mean score in each of the seven domains of patient satisfaction. Mean score of general satisfaction was 4.8 in NL-IVTs and 4.5 in DL-IVTs (P ≤ 0.01). A wide SD of 1.1 was noted in DL-IVTs. This indicates a relatively larger variation in satisfaction reported by patients in DL-IVTs than in NL-IVTs. Score of quality was perceived to be the same (3.9 ± 0.3) between NL-IVTs than in DL-IVTs. Score of interpersonal manner is higher in NL-IVTs (4.0 ± 0.1) than in DL-IVTs (3.8 ± 0.5). In terms of financial aspect, NL-IVT (2.8 ± 1.3) showed higher score than DL-IVT (2.2 ± 1.4). However, overall score in financial aspect was lower than other dimensions in both DL- and NL-IVT. Patients responded more positively (2.8) that the injection is affordable in NL-IVT but responded negatively (2.2) in DL-IVT. There were no differences in information/communication between DL- and NL-IVT. Higher score was observed in NL-IVT than in DL-IVT in terms of time spent with injector and staff competence.
Table 2.
Mean patient satisfaction score (n = 135).
| Scale | Doctor led | Nurse led | P value |
|---|---|---|---|
| General satisfaction | 4.5 (1.1) | 4.8 (0.8) | <0.01 |
| Quality | 3.9 (0.3) | 3.9 (0.3) | 0.37 |
| Interpersonal manner | 3.8 (0.5) | 4 (0.2) | <0.01 |
| Financial aspect | 2.2 (1.4) | 2.8 (1.3) | <0.01 |
| Information/communication | 3.8 (0.7) | 3.8 (0.6) | 0.49 |
| Time spent with injector | 3.7 (0.7) | 3.9 (0.3) | <0.01 |
| Staff competence | 3.5 (0.8) | 3.8 (0.6) | <0.01 |
Bold numbers indicate superiority in the domain that it is represented in.
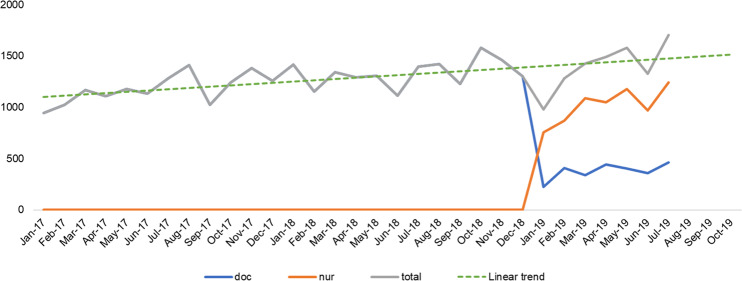
Number of injections before and after initiation of the nurse injector programme
An average of 1347 IVT injections are done every month from January 2017 to January 2019. We calculated the total number of monthly NL-IVTs from February to September 2019. There were 1280 in February, 1425 in March, 1489 in April, 1581 in May, 1327 in June, 1703 in July, 1591 in August, and 1319 NL-IVTs in September in 2019 (orange colour in Fig. 3). This increasing trend in the number of IVT delivered is likely to continue with the implementation of the new system.
Fig. 3. Number of monthly injections from January 2017 to September 2019 in the Singapore National Eye Centre.
After an initial dip in the number of intravitreal injections at the start of the nurse programmee, there was a gradual increase in the number of monthly injections performed in the centre. The increase in capacity is expected to continue as the service develops.
Evaluation of the financial cost of IVT after implementing NL-IVT
The difference in cost between a DL-IVT and NL-IVT was estimated to be 286 SGD (136 GBP). The monthly difference is projected to be 386,000 SGD based on the average monthly number of IVTs in 2019. Therefore, a total of 4.6 and 6.6 million SGD (2.61–3.75 million GBP) can be saved annually for patients receiving NL-IVT in SNEC and Singapore, respectively.
Discussion
Our study describes an introduction of NL-IVT in an Asian tertiary eye centre and evaluates patient safety, waiting time, satisfaction, and cost savings. In the patient satisfaction survey, the patients were satisfied with the NL-IVTs and average waiting time was reduced by 20 min since the implementation. The number of monthly IVTs continued to increase steadily before and after the implementation. Implementing this service is expected to save up to 6.6 million SGD (3.8 million GBP) annually.
Safety
The most feared complication of anti-VEGF injections is endophthalmitis, which has an occurrence or incidence ranging from 1 case in 1000 to 1 case in 5000 [27–29]. We would expect one to five patients developing endophthalmitis in our study population of 8599 injections based on previous statistics [27–29]. The complication rate in this study suggests that NL-IVTs are a viable alternative to DL-IVTs. Other complications like vitreous haemorrhage (0.07%) and raised intraocular pressure (0.17%) have also not been recorded in our study so far [18]. Our results thus far suggest the comparable quality and safety of an NL-IVT service. However, patient safety must be judiciously audited to ensure high safety standards as the service develops further.
Waiting time
The issue of long patient waits has attracted increasing public attention due to the negative effects of waiting on patients’ satisfaction with healthcare [30, 31]. A previous study in an ophthalmology clinic showed that waiting time was associated with patient satisfaction, regardless of financial status, with a linear relationship between these two variables [32]. We show that an average of 20 min is saved per injection for the patient when the injection is carried out by a nurse. Waiting time for NL-IVTs was only 3.6 min with minimal waiting time for the procedure itself. Shortening the waiting time for IVT injection will increase patients’ satisfaction with the service. These time savings to these patients and their family are not insubstantial because young people who accompany the elderly patient are mainly an economically active population. An efficient service will result in better compliance rates. A positive experience will contribute to patients being more proactive with their IVT treatment and potentially improve the real-world visual outcomes of IVT.
Patient satisfaction
Previous studies have shown a high acceptance rate of NL-IVT [12, 17]. Our patient sample is more satisfied with NL-IVT as measured in our survey. NL-IVT scored higher in five out of seven dimensions than DL-IVT. Patients were generally satisfied with both NL and DL-IVTs with score of ~4. However, the financial aspect of IVT is particularly concerning for patients, with relatively low scores of 2.8 for NL-IVT and 2.2 for DL-IVT. Although patients are happier with the reduction in cost, some still struggle with the continual need for IVT and the cost can rise quickly. We believe that the financial cost will serve as an important decision-making factor for compliance for IVT. Overall, our results suggest that patients are equally satisfied with an NL-IVT service.
The trend of IVT and the relevance of a nurse-led service
The prevalence of AMD, DMO, and RVO is projected to increase by 113%, 54% and 46% by 2040, respectively, in the Singapore population [33]. The amount of IVTs is expected to increase accordingly (Fig. 3). Currently, our centre delivers ~16,000 injections a year. Ophthalmology training is long and expensive. The increases in IVT demand will outpace the ability to train sufficient ophthalmologists to deliver this service. There will be difficulties in coping with the increasing treatment burden if an adequate solution is not available. Many studies have shown that supplementing manpower via training more allied health professionals is one successful solution for overcoming the medical workforce shortage [15, 17, 21, 34]. Ophthalmologic trainees/doctors must carry out clinical duties and perform injections concurrently. By having trained allied health professionals administer IVT, doctors can dedicate more time to see clinical cases and treat patients. This will also reduce the workload of the doctors. By providing a quick, safe, and effective training programme for nurses to deliver IVT, we can overcome the inelastic supply of doctors and ensure that the service will not be overwhelmed in the future. This is in line with the new models of care needed to sustain the growing patient population amidst the expected shrinking healthcare professional team.
Cost
Another important aspect is injection cost. In a fee for service healthcare model, the accumulated number of IVT injections can result in considerable financial cost for the patient. A recent study showed that living in the most deprived areas was associated with a significantly higher risk of severe reduction in the visual acuity of patients with neovascular AMD (relative risk = 3.59, 95% confidence interval, 1.39–9.27) [35]. Through the introduction of the NL-IVT, we have reduced the cost of injection by ~61% per injection, this would represent substantial savings for the patients given that the average patient receives 6–11 injections per year. This will potentially lead to an increase in treatment compliance if financial concerns have been a deterring factor. We hope lower costs of IVT will improve patient accessibility to treatment.
This study evaluates the patient’s experience of NL-IVT in a high volume centre in Singapore and identifies potential improvements we can make to the service. Implementing an NL-IVT service will reduce the number of injections that ophthalmologists perform, and importantly allow doctors to dedicate more time to seeing patients with these retinal diseases.
Limitations of this study include a short study duration and the questionnaire’s qualitative nature. It is noteworthy that >8000 IVT cases were done by nurse from February to September 2019 without significant adverse effect in the largest institution in Singapore, but we must always be cautious and continually audit the service. There is a possibility that the patients gave favourable answers to the nurse because the IVT was administered by nurses. To reduce this response bias, patients were surveyed by doctor. There is also a possibility that our modified questionnaire could not fully estimate the patients’ satisfaction. Our study might not be able to capture the full range of complications as some may be unreported. English is also not the first language for many taking the survey and understanding the questions might not be easy. We have tried to mitigate this by using the same questions for DL- and NL-IVT to evaluate the service. Cost would also influence patient satisfaction with the service, regardless of care standards. This may not be applicable to other countries, where the cost of IVT might not differ based on provider.
In conclusion, with an increasing trend of anti-VEGF IVT for the foreseeable future, an NL-IVT could transform models of care for many major ophthalmology services globally. We have shown that an NL-IVT program is safe, reduced waiting time for the procedure, increased patients’ satisfaction of IVT, and reduce patents’ cost. This will reduce any potential delays in the management of retinal diseases. Our study provides a rationale for the design, implementation, and evaluation of an NL-IVT service in Asia, which appears comparable compared with DL-IVT.
Summary
What was known before
Intravitreal injection load is increasing.
Nurse administered intravitreal injection services are slowly gaining acceptance to increase treatment capacity but apart from few centres like Tan Tock Seng Hospital (TTSH) in Singapore, who have launched this service in 2017, no such services have been reported in Asia.
What this study adds
Design of an NL-IVT programme.
Experience and patient satisfaction in NL-IVT in a large Asian eye centre.
Safety and cost efficacy of NL-IVTs.
Supplementary information
Compliance with ethical standards
Conflict of interest
THR was a scientific advisor to Medi-Whale Inc. THR received stocks as a part of the standard compensation package; potential conflicts of interests are managed according to the institutional policies of the Singapore Health System (SingHealth). TYW is an inventor of a patent on the various deep learning system in ophthalmology; potential conflicts of interests are managed according to the institutional policies of the Singapore Health System (SingHealth) and the National University of Singapore. The remaining authors declare no competing interests.
Ethics statement
This retrospective cross-sectional study was conducted in accordance with the declaration of Helsinki and approved by the Singhealth Centralised Institutional Review Board.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Alvin Teo Wei Jun, Tyler Hyungtaek Rim
Change history
2/11/2021
A Correction to this paper has been published: 10.1038/s41433-020-1077-8
Supplementary information
The online version of this article (10.1038/s41433-020-0920-2) contains supplementary material, which is available to authorized users.
References
- 1.Lim LS, Mitchell P, Seddon JM, Holz FG, Wong TY. Age-related macular degeneration. Lancet. 2012;379:1728–38. doi: 10.1016/S0140-6736(12)60282-7. [DOI] [PubMed] [Google Scholar]
- 2.Yau JW, Rogers SL, Kawasaki R, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35:556–64. doi: 10.2337/dc11-1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wong WL, Su X, Li X, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health. 2014;2:e106–116. doi: 10.1016/S2214-109X(13)70145-1. [DOI] [PubMed] [Google Scholar]
- 4.Spooner KL, Mhlanga CT, Hong TH, Broadhead GK, Chang AA. The burden of neovascular age-related macular degeneration: a patient’s perspective. Clin Ophthalmol. 2018;12:2483–91. doi: 10.2147/OPTH.S185052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kataja M, Hujanen P, Huhtala H, Kaarniranta K, Tuulonen A, Uusitalo-Jarvinen H. Outcome of anti-vascular endothelial growth factor therapy for neovascular age-related macular degeneration in real-life setting. Br J Ophthalmol. 2018;102:959–65. doi: 10.1136/bjophthalmol-2017-311055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martin DF, Maguire MG, Fine SL, et al. Ranibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: two-year results. Ophthalmology. 2012;119:1388–98. doi: 10.1016/j.ophtha.2012.03.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cohen SY, Mimoun G, Oubraham H, et al. Changes in visual acuity in patients with wet age-related macular degeneration treated with intravitreal ranibizumab in daily clinical practice: the LUMIERE study. Retina. 2013;33:474–81. doi: 10.1097/IAE.0b013e31827b6324. [DOI] [PubMed] [Google Scholar]
- 8.Holz FG, Tadayoni R, Beatty S, et al. Multi-country real-life experience of anti-vascular endothelial growth factor therapy for wet age-related macular degeneration. Br J Ophthalmol. 2015;99:220–6. doi: 10.1136/bjophthalmol-2014-305327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leasher JL, Bourne RR, Flaxman SR, et al. Global estimates on the number of people blind or visually impaired by diabetic retinopathy: a meta-analysis from 1990 to 2010. Diabetes Care. 2016;39:1643–9. doi: 10.2337/dc15-2171. [DOI] [PubMed] [Google Scholar]
- 10.Rogers S, McIntosh RL, Cheung N, et al. The prevalence of retinal vein occlusion: pooled data from population studies from the United States, Europe, Asia, and Australia. Ophthalmology. 2010;117:313–319.e311. doi: 10.1016/j.ophtha.2009.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McKendry M, McGloin H, Saberi D, Caudwell L, Brady AR, Singer M. Randomised controlled trial assessing the impact of a nurse delivered, flow monitored protocol for optimisation of circulatory status after cardiac surgery. BMJ. 2004;329:258. doi: 10.1136/bmj.38156.767118.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.DaCosta J, Hamilton R, Nago J, et al. Implementation of a nurse-delivered intravitreal injection service. Eye. 2014;28:734–40. doi: 10.1038/eye.2014.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simcock P, Kingett B, Mann N, Reddy V, Park J. A safety audit of the first 10 000 intravitreal ranibizumab injections performed by nurse practitioners. Eye. 2014;28:1161–4. doi: 10.1038/eye.2014.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Michelotti MM, Abugreen S, Kelly SP, et al. Transformational change: nurses substituting for ophthalmologists for intravitreal injections—a quality-improvement report. Clin Ophthalmol. 2014;8:755–61. doi: 10.2147/OPTH.S59982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rasul A, Subhi Y, Sorensen TL, Munch IC. Non-physician delivered intravitreal injection service is feasible and safe—a systematic review. Dan Med J. 2016;63:pii: A522. [PubMed] [Google Scholar]
- 16.Austeng D, Morken TS, Bolme S, Follestad T, Halsteinli V. Nurse-administered intravitreal injections of anti-VEGF: study protocol for noninferiority randomized controlled trial of safety, cost and patient satisfaction. BMC Ophthalmol. 2016;16:169. doi: 10.1186/s12886-016-0348-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gregg E. Nurse-led ranibizumab intravitreal injections in wet age-related macular degeneration: a literature review. Nurs Stand. 2017;31:44–52. doi: 10.7748/ns.2017.e10344. [DOI] [PubMed] [Google Scholar]
- 18.Samalia P, Garland D, Squirrell D. Nurse specialists for the administration of anti-vascular endothelial growth factor intravitreal injections. N Z Med J. 2016;129:32–38. [PubMed] [Google Scholar]
- 19.Li E, Greenberg PB, Krzystolik MG. Nurse-administered intravitreal injections: a systematic review. Graefes Arch Clin Exp Ophthalmol. 2015;253:1619–21. doi: 10.1007/s00417-014-2921-y. [DOI] [PubMed] [Google Scholar]
- 20.Mohamed R, Ramcharan D, Srikaran S, Mensch E. A model of clinical practice: a randomised clinical study evaluating patient satisfaction of nurse-led vs consultant-led intravitreal injection. Eye. 2018;32:1148–9. doi: 10.1038/s41433-017-0008-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gallagher MJ. Introduction of a nurse-led intravitreal injection service in ophthalmology. Br J Nurs. 2017;26:800–3. doi: 10.12968/bjon.2017.26.14.800. [DOI] [PubMed] [Google Scholar]
- 22.Hasler PW, Bloch SB, Villumsen J, Fuchs J, Lund-Andersen H, Larsen M. Safety study of 38,503 intravitreal ranibizumab injections performed mainly by physicians in training and nurses in a hospital setting. Acta Ophthalmol. 2015;93:122–5. doi: 10.1111/aos.12589. [DOI] [PubMed] [Google Scholar]
- 23.Bolme S, Morken TS, Follestad T, Sorensen TL, Austeng D. Task shifting of intraocular injections from physicians to nurses: a randomized single-masked noninferiority study. Acta Ophthalmol. 2019;98:139–44. doi: 10.1111/aos.14184. [DOI] [PubMed] [Google Scholar]
- 24.Ng WY, Cheung CM, Mathur R, et al. Trends in age-related macular degeneration management in Singapore. Optom Vis Sci. 2014;91:872–7. doi: 10.1097/OPX.0000000000000283. [DOI] [PubMed] [Google Scholar]
- 25.Ng WY, Tan GS, Ong PG, et al. Incidence of myocardial infarction, stroke, and death in patients with age-related macular degeneration treated with intravitreal anti-vascular endothelial growth factor therapy. Am J Ophthalmol. 2015;159:557–564.e551. doi: 10.1016/j.ajo.2014.12.005. [DOI] [PubMed] [Google Scholar]
- 26.Marshall GN, Hays RD. The patient satisfaction questionnaire short-form (PSQ-18). Santa Monica, CA: Rand; 1994.
- 27.Mason JO, 3rd, White MF, Feist RM, et al. Incidence of acute onset endophthalmitis following intravitreal bevacizumab (Avastin) injection. Retina. 2008;28:564–7. doi: 10.1097/IAE.0b013e3181633fee. [DOI] [PubMed] [Google Scholar]
- 28.Fintak DR, Shah GK, Blinder KJ, et al. Incidence of endophthalmitis related to intravitreal injection of bevacizumab and ranibizumab. Retina. 2008;28:1395–9. doi: 10.1097/IAE.0b013e3181884fd2. [DOI] [PubMed] [Google Scholar]
- 29.Fileta JB, Scott IU, Flynn HW., Jr Meta-analysis of infectious endophthalmitis after intravitreal injection of anti-vascular endothelial growth factor agents. Ophthalmic Surg Lasers Imaging Retin. 2014;45:143–9. doi: 10.3928/23258160-20140306-08. [DOI] [PubMed] [Google Scholar]
- 30.Mohsin M, Forero R, Ieraci S, Bauman AE, Young L, Santiano N. A population follow-up study of patients who left an emergency department without being seen by a medical officer. Emerg Med J. 2007;24:175–9. doi: 10.1136/emj.2006.038679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boudreaux ED, O’Hea EL. Patient satisfaction in the emergency department: a review of the literature and implications for practice. J Emerg Med. 2004;26:13–26. doi: 10.1016/j.jemermed.2003.04.003. [DOI] [PubMed] [Google Scholar]
- 32.McMullen M, Netland PA. Wait time as a driver of overall patient satisfaction in an ophthalmology clinic. Clinical ophthalmology. 2013;7:1655. [DOI] [PMC free article] [PubMed]
- 33.Ansah JP, Koh V, de Korne DF, et al. Projection of eye disease burden in Singapore. Ann Acad Med Singap. 2018;47:13–28. [PubMed] [Google Scholar]
- 34.Michelotti MM, Abugreen S, Kelly SP, et al. Transformational change: nurses substituting for ophthalmologists for intravitreal injections–a quality-improvement report. Clin Ophthalmol. 2014;8:755. doi: 10.2147/OPTH.S59982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.More P, Almuhtaseb H, Smith D, Fraser S, Lotery AJ. Socio-economic status and outcomes for patients with age-related macular degeneration. Eye. 2019;33:1224–31. doi: 10.1038/s41433-019-0393-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.