Figure 2.
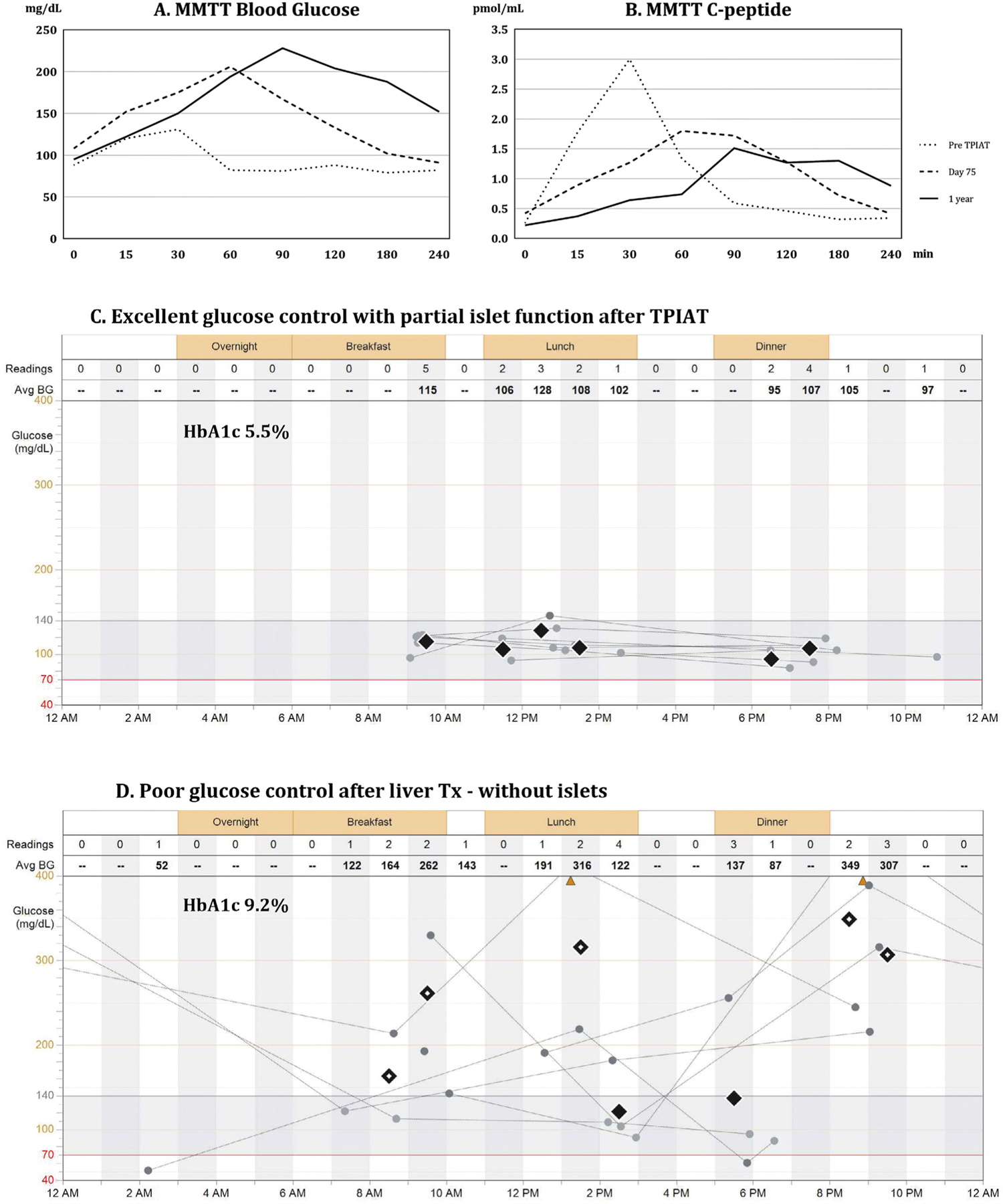
A, B, C, D. Metabolic testing of islet graft function and blood glucose control.
Panel A presents blood glucose levels, whereas Panel B presents serum c-peptide levels during mixed meal tolerance test (MMTT), which was performed prior to the procedure (dotted line), at postoperative day 75 (dashed line), and at 1 year (continuous line) after total pancreatectomy with islet autotransplantation (TPIAT). Prior to surgery, islets controlled blood glucose during the mixed meal challenge; fasting blood glucose was 100 mg/dL, peaked at 120 mg/dL around 30 minutes after consumption of mixed meal, and dropped to normal values afterwards. This was demonstrated by levels of serum c-peptide, which corresponds to endogenous insulin released from islets (Panel A, B, dotted lines). After TPIAT, insulin released from the islet autograft, as represented by serum c-peptide (Panel B, dashed and continuous line), prevented a further rise of blood glucose above 230 mg/dL during the MMTT (Panel A, dashed and continuous line). The test confirmed partial islet graft function by demonstrating a clinically significant insulin release from the islet graft and the need for exogenous support for optimal glucose control.
Panel C presents daily trends of blood glucose recorded over a period of one week in the patient after TPIAT with partial islet graft function, allowing for optimal glucose control (HbA1c 5.5%). Most of the time blood glucose remained within the normal range of 70–150 mg/dL, without episodes of hyper- or hypoglycemia.
Panel D presents extremely poor glucose control in the same patient following liver transplantation with hepatectomy of the liver, which contained the islet autograft. The patient struggled with insulin dose adjustments despite using an insulin pump, glucose monitoring system, and intensive diabetic care. He had persistent hyperglycemia (HbA1c 9.2%) with episodes of both severe hyperglycemia (> 400 mg/dL) and hypoglycemia (< 54 mg/dL) with loss of consciousness and seizures.
