Highlights
-
•
Administering the screening tool in an electronic format provides the best results.
-
•
41.4% of households were at risk for food insecurity at this urban clinic.
-
•
Food insecurity risk can differ by ethnicity depending on population makeup.
-
•
Screening for households at risk for food insecurity is important.
-
•
Challenges to universal screening exist but there are solutions to overcoming them.
Keywords: Social determinants of health, Chronic disease, Qualitative research, Food insecurity, Mass screening
Abstract
Millions of Americans face food insecurity, yet a universal screening tool is not in place. Food insecurity is known to be associated with poor health outcomes such as heart disease, diabetes mellitus, and hypertension in adults, and low school performance and mental illness in children. From January 2017 through February 2017, we utilized a validated two-item screening tool to assess the prevalence of households at risk for food insecurity and conducted a focus group of pediatricians. Patients at a Federally Qualified Health Center in New Haven, Connecticut were screened. Pediatricians of the American Academy of Pediatricians comprised the focus group. 534 of 1272 screening tool respondents were at risk for food insecurity (41.4%). Male respondents had higher prevalence than females (46.3% vs 38.9%, p = 0.009), and Hispanics (34.4%) less than Whites (54.4%) and Blacks (53.8%) (p < 0.001). Moreover, we executed a qualitative study of pediatricians’ perception of food insecurity screening via a focus group. Themes that emerged from the focus group were agreement on the high importance of food insecurity screening, concern from caregivers about child neglect, and the difficulty of implementing the screening tool due to time constraints. We achieved successful implementation of the screening tool into the electronic medical record with a high completion rate of 97.9%. Identified barriers to universal screening for food insecurity include lack of efficient methods to direct food-insecure patients to resources and continued stigma regarding food insecurity.
1. Introduction
Though the United States is touted as one of the world’s richest countries, millions of Americans face food insecurity. The United States Department of Agriculture (United states department of agriculture, 2019) defines food insecurity as “not having enough food for an active, healthy life.” The USDA Economic Research Service reported that 11.1% (14.3 million) of U.S. households were food insecure at some point in 2018. Moreover, 7.1% of U.S. households with children (2.7 million households) were food insecure (USDA: Household food security in the United States in 2018).
Numerous studies demonstrate the association of food insecurity with many chronic diseases such as diabetes mellitus, hypertension, and heart disease (Seligman et al., 2010, Saiz et al., 2016). In addition, children who face food insecurity are more likely than food-secure children to experience negative effects on their behavior and development; for instance, malnutrition, obesity, poor school performance, more hospitalizations, and mental health issues such as depression and anxiety (O’Keefe, 2015).
Federally Qualified Health Centers (FQHC) are medical clinics that provide medical care to underserved populations which include migratory and seasonal agricultural workers, people who are homeless, and public housing residents. The population in the city of New Haven consists of 130,612 people, of which 22.1% are 17 years and younger, 10.3% are over 65 years old, and 52.7% are female. The food insecurity rate in the city is 22%, whereas in the state of Connecticut, it is 12%. Blacks represent the majority of the city population at 33.0% (9.7% in Connecticut), while Whites comprise 30.8% (68.7% in Connecticut), and Hispanics constitute 28.6% (15.0% in Connecticut) (New Haven, 2018). These statistics outline the demographic differences between the city and state and may also affect the food insecurity rate in the city compared to that of the state.
The USDA provides several tools (6-, 10-, and 18-item) to screen for food insecurity (USDA ERS: Survey Tools, 2019). In November 2015, the American Academy of Pediatrics (AAP) issued a policy statement (Promoting Food Security for All Children, 2018) that endorses the use of the two-item screening tool, now coined the Hunger Vital SignTM. This survey developed by Hager et al. (2010) for identifying households at risk for food insecurity has 97% sensitivity, 83% specificity, and decreases respondent burden (2010). Specifically, this screening tool was designed to be utilized in the clinics; thus, the results are applicable and valid in this particular setting, rather than in community organizations or food pantries, etc. Other recent studies have also proven the high sensitivity and good specificity of this simple screening tool (Makelarski et al., 2017, Gundersen et al., 2017). Once patients are identified as being at risk for food insecurity, they are referred to food assistance programs such as the Supplemental Nutrition Assistance Program (SNAP, formerly known as the Food Stamp Program), the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), and free food programs for school-age children and for seniors. Since the announcement of the AAP policy recommendation for universal food insecurity screening, an increasing number of clinics and emergency departments have piloted this tool (Makelarski et al., 2017, Smith et al., 2017, Knowles et al., 2018, Starr et al., 2018, Martel et al., 2018, Barnidge et al., 2017, Garcia-Silva et al., 2017). Recently, the Centers for Medicare and Medicaid Innovation Center launched a $157 million program to assess the impact of screening for health-related social needs, including risk of food insecurity (Gundersen et al., 2017).
The purpose of this study was to assess the prevalence of households at risk for food insecurity using the two-item screening tool and to identify the challenges associated with universal screening in clinics with recommended solutions by pediatricians of the Connecticut Chapter of the AAP.
2. Methods
2.1. Implementation of survey
We used the triangulation method to gain better understanding of an investigated phenomenon—in this case, food insecurity—by obtaining information from different perspectives (Carter et al., 2014, Farmer et al., 2006). In other words, we collected data from multiple sources which included literature review, interviews, surveys and a focus group to identify convergence, dissonance, potential biases and uncertainties of evidence. After conducting literature review, the Community Services Administration (CSA) of the City of New Haven convened a half-day meeting in June 2016 to discuss food insecurity with non-profit organizations, food and meal distribution agencies, businesses, government entities, academia, health professionals, and associations. Follow-up interviews were held with the chief executive officers (CEO) of four healthcare organizations to explore the perspectives of food insecurity and feasibility of using the Hunger Vital SignTM (HVS). This tool was used to assess risk for food insecurity in their clinics for a period of two months. The CEOs of the four healthcare organizations agreed to participate in this study. Two are FQHCs, one is a private pediatric health clinic, and the fourth is a family medical practice. The private pediatric health clinic, the family medical practice, and one of the FQHCs screened for food insecurity using the paper form of the HVS while the other FQHC programmed the tool into the patient intake form of their electronic health record. This latter FQHC is Cornell Scott-Hill Health Center (CSHHC) and this manuscript will be limited to findings from this study site.
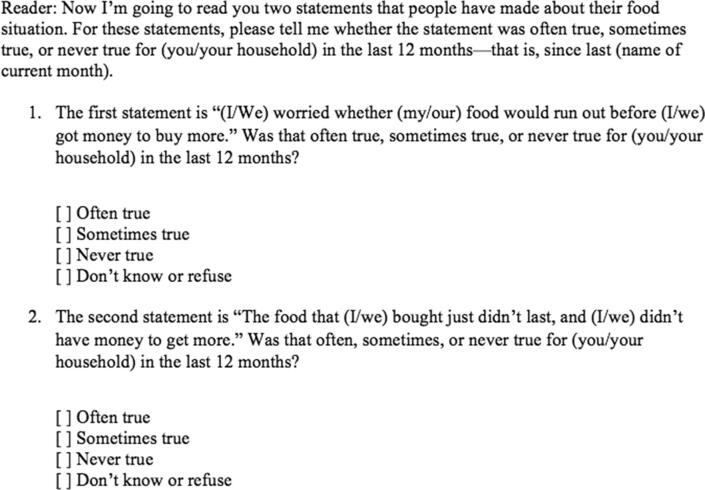
We met with the CEO, two chief medical officers (CMO), and two nurses of CSHHC to plan the pilot study. We obtained necessary leadership approval and a decision was made to adjust their electronic health system (Centricity) and add the two-item screening tool to improve consistency of practice. Moreover, the two CMOs were designated as the “champions” to coordinate the pilot implementation of the two-item screening tool within CSHHC. At CSHHC, the two-item screening tool was administered electronically by a medical assistant during each patient encounter from January 9, 2017 through February 28, 2017. The medical assistant administered the survey by conducting it verbally with the patient and entering their responses into the health record by computer. This occurred during the intake process before the encounter with the healthcare provider. All patients who presented for any type of visit (physical exam, follow-up visit, or chief complaint visit) were screened. Patients of any age were included; there were no specific inclusion or exclusion criteria. Patients who were minors (younger than 18 years old) had their surveys answered by the parent or guardian who presented with the patient. For any patients with low literacy, the medical assistant would read out the survey questions in either English or Spanish (or use a translator for patients who did not speak either language fluently). Both English and Spanish versions (Fig. 1) were provided. The two statements were:
-
1.
Within the past 12 months, we worried whether our food would run out before we got money to buy more.
-
2.
Within the past 12 months, the food we bought just didn’t last and we didn’t have the money to get more.
Fig. 1.
Two-item food insecurity screening tool administered at Cornell-Scott Hill Health Center in New Haven, Connecticut from January 2017 through February 2017.
The answer options were “often true,” “sometimes true,” “never true,” or “Don’t know/refuse to answer.” Patients who answered “often true” or “sometimes true” to either statement were identified as at risk of food insecurity. Those identified as food-insecure received resources on how to obtain food and supplemental nutrition in New Haven, such as the Get Connected cards issued by the City of New Haven (Fig. 2). Answers remained confidential. Moreover, previously recorded information from the electronic health record on patient age, gender, and race/ethnicity were compared to food security status. The Quinnipiac University Human Experimentation Committee/Institutional Review Board approved the study protocol (#09916 “Screening for Food Insecurity in New Haven using a Two-Item Questionnaire”).
Fig. 2.

Get Connected New Haven card provided to patients surveyed using the two-item food insecurity screening tool at Cornell-Scott Hill Health Center in New Haven, Connecticut from January 2017 through February 2017.
2.2. Focus group
After the completion of the survey at CSHHC in February 2017 and reviewing the results, we were curious about the pediatricians’ opinions regarding implementation of the HVS. Based on the interview findings from the four CEOs mentioned earlier in the methods section, we developed these three questions for the focus group discussion:
-
1.
How important is screening for food insecurity?
-
2.
Does your clinic currently screen for food insecurity?
-
3.
What should be done in order to implement this screening tool in all of Connecticut?
We took the time to foster a professional relationship with the Connecticut chapter of the AAP (CT-AAP). We partnered with CT-AAP to discuss their members’ perspectives on food insecurity and compliance with the AAP recommendation to screen for food insecurity using the HVS. We pilot-tested these three questions with two other researchers and a pediatrician who was a former president of CT-AAP for clarity of meaning and alignment with the study purpose. An additional probe question to find out who administers the screening tool for those that use the tool was suggested.
In 2018, the CT-AAP chapter invited members to a focus group meeting. Due to the busy schedules of the pediatricians, we conducted a 30-minute focus group as part of an already scheduled AAP event. A facilitator was used to make conversation flow easily and a note taker to document the narratives. Eleven pediatricians attended and all of them participated in the discussion at the CT-AAP chapter meeting. None of these pediatricians worked at the FQHC Cornell Scott-Hill Health Center. A verbal consent was obtained from the pediatricians at the onset of the conversation. These participants allowed us to tape-record the conversation as a quality check to assure accuracy of the note-taking, data reporting, and interpretation. Promise of confidentiality was provided and subjects remained anonymous. The three pilot-tested focus group questions were asked with the additional probe question about who specifically administered the screening tool and in what form–paper or computer (electronic health record)—the survey was administered. We heard their perspectives on the screening tool and suggestions to aid adherence with implementing the screening tool.
Descriptive statistics included frequencies and percentages. Chi-square was used to test for an association between demographic characteristics and food insecurity. Analyses were conducted using SPSS v25 (IBM Corp. Armonk, NY) and statistical significance was set at an alpha level of 0.05. We conducted tests of interaction effects and none were significant.
3. Results
3.1. Demographics and overall food insecurity
Table 1 shows the demographic characteristics of the patients who visited CSHCC during the study period. The age of the patients ranged from 13 months to 94 years old. Most were female (58%), a significant proportion were children (17%) or elderly (10%), and the largest ethnic group was Hispanic (59%) followed by Blacks (30%). Nearly 3% were homeless. Table 2 shows the responses to the two food insecurity questions. Nearly 40% responded sometimes or always true to “would worry food would run out before got money to buy more food” and a similar percentage responded sometimes or always to “food bought just didn’t last and didn’t have money to get more.” The percentage of patients who met the criteria for food insecurity was 42%.
Table 1.
Demographic Characteristics (n = 1299) of patients surveyed using the two-item food insecurity screening tool at Cornell-Scott Hill Health Center in New Haven, Connecticut from January 2017 through February 2017.
| Characteristic | Frequency | Percentage |
|---|---|---|
| Gender | ||
| Female | 759 | 58.4% |
| Male | 540 | 41.6 |
| Age Group | ||
| ≤17 | 222 | 17.1% |
| 18 – 30 | 146 | 11.2 |
| 1 – 45 | 316 | 24.3 |
| 46 – 65 | 488 | 37.6 |
| ≥66 | 127 | 9.8 |
| Ethnicity | ||
| Hispanic | 763 | 58.7% |
| Black | 388 | 29.9 |
| Asian | 9 | 0.7 |
| White | 130 | 10.0 |
| Other | 9 | 0.7 |
| Homeless Status | ||
| Homeless/Shelter/Street | 36 | 2.8% |
| Not Homeless | 1263 | 97.2 |
Table 2.
Responses to Food Insecurity Questions from patients surveyed at the Cornell-Scott Hill Health Center in New Haven, Connecticut from January 2017 through February 2017.
| Characteristic | Frequency | Percentage |
|---|---|---|
| Worried food would run out before got money to buy more | ||
| Never True | 746 | 57.4% |
| Sometimes True | 480 | 37.0 |
| Always True | 46 | 3.5 |
| Refued to Answer | 27 | 2.1 |
| Food bought just didn’t last & didn’t have money to get more | ||
| Never True | 793 | 61.0% |
| Sometimes True | 421 | 32.4 |
| Always True | 56 | 4.3 |
| Refused to Answer | 29 | 2.2 |
| Food Insecurity (n = 1272) | ||
| No | 738 | 58.0% |
| Yes | 534 | 42.0% |
3.2. Food security status vs. Demographic factors
Table 3 shows the prevalence of food insecurity by CHSCC demographic characteristics. Males were more likely to experience food insecurity than females (46% vs 39%, p = 0.009). There was a difference by age group (p < 0.001) with children (19%) and the elderly (37%) having lower rates compared to other adults. Food insecurity differs by ethnicity (p < 0.001) with Whites and Blacks reporting the highest rate of insecurity (54%) and Asians the least (22%).
Table 3.
Percentage with Food Insecurity by Demographic Characteristics of patients surveyed using the two-item food insecurity screening tool at the Cornell-Scott Hill Health Center in New Haven, Connecticut from January 2017 through February 2017.
| Characteristic | Percentage | P-Value |
|---|---|---|
| Gender | 0.009 | |
| Female | 38.9% | |
| Male | 46.3 | |
| Age Group | <0.001 | |
| ≤17 | 19.1% | |
| 18 – 30 | 43.2 | |
| 31 – 45 | 49.8 | |
| 46 – 65 | 48.1 | |
| ≥66 | 36.9 | |
| Ethnicity | <0.001 | |
| Hispanic | 34.4% | |
| Black | 53.8 | |
| Asian | 22.2 | |
| White | 54.4 | |
| Other | 25.0 | |
| Homeless Status | 0.002 | |
| Homeless/Shelter/Street | 15.6% | |
| Not Homeless | 42.7 |
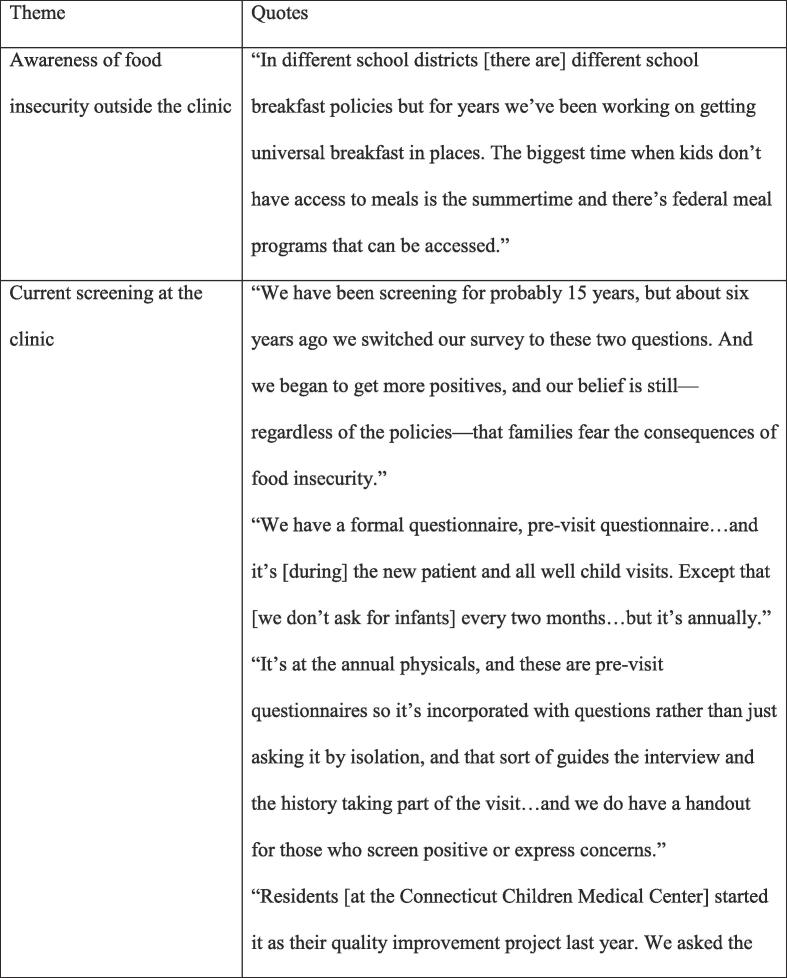
3.3. Focus group responses
Participants agreed that screening for food insecurity is either important or very important. Barriers to asking the questions included lack of time and other competing screening questions (i.e. anticipatory guidance questions such as car seat safety, sunscreen usage, gun safety, domestic violence) and uncertainty in how to direct food-insecure patients to food resources (Fig. 3).
Fig. 3.
Themes and quotes from focus group of pediatricians discussing food insecurity. The focus group was conducted at the American Academy of Pediatrics Connecticut Chapter meeting in Hartford, Connecticut in 2018.
One pediatrician stated that they have been screening for food insecurity for at least a decade and that they screen during the annual physicals. Two responded that the surveys are administered in paper form, are administered in the waiting room for the caregiver to complete, and that the provider reviews it with the caregiver.
Challenges that were identified or perceived include these themes: (i) the caregivers were reluctant to answer due to fear that responding in the affirmative would reflect child neglect or failure of the parent to provide for their children and (ii) the difficulty and costliness of incorporating the screening tool into the various electronic health record systems.
Suggestions shared to increase screening of food insecurity include but are not limited to the following: (i) develop and provide information on available local food resources to be easily accessible to the doctors’ offices, (ii) work with health insurance companies and group healthcare providers, including accountable care organizations, to mandate food insecurity screening, (iii) work with legislators and state Medicaid or administrative offices to require food insecurity screening and provide a metric or add as part of anticipatory guideline for universal screening, (iv) promote through professional associations and integrate the food insecurity screening tool into a standard tool, like Bright FuturesTM, and (v) provide webinars and trainings on subject.
4. Discussion
This study demonstrated that a two-item food insecurity screening tool can be effectively used at a Federally Qualified Health Center. We obtained a high response rate of 97.9% and identified 41.4% of households at risk for food insecurity within this population.
Due to the large sample size, there are notable and statistically significant differences between the different sociodemographic groups. The age group with the highest rate of food insecurity was the 31–45 years old group (155/311 or 49.8%), while the 17 years and younger group had the lowest rate (41/215 or 19.1%). Moreover, more males identified as at risk of being food insecure than females. White respondents comprised the highest percentage of food insecurity (68/125 or 54.4%), and Blacks came second (203/377 or 53.8%). Interestingly, these findings are different compared to what is observed on a national basis, which is that children, females, and non-white respondents were more likely to be food insecure. This may be due to the fact that the population in New Haven, where CSHHC is located, has a higher proportion of food-insecure white and male individuals/households which can skew the demographics.
Our screening tool was administered verbally by a medical assistant during the intake process rather than having the respondent complete the survey on a written basis i.e. on an electronic device. Interestingly, a recent study demonstrated that written food insecurity surveys had higher numbers of positive screens compared to surveys administered verbally (Palakshappa et al., 2019). Several explanations for this phenomenon include 1) the patient is more comfortable when filling out a written survey rather than asked face-to-face about their food security status and 2) written surveys being more efficient than verbal surveys especially in a busy clinic.
More efforts need to be done to educate medical students, residents, and physicians on how to screen for food insecurity and how to refer food-insecure patients to resources. A few clinics and institutions have already demonstrated effective models. A pre/post-survey with an educational intervention (i.e. 30–50 min lecture-based presentation with a discussion about how to discuss food insecurity with a patient and suggestions for systems-based changes) at the University of California, San Diego (UCSD) revealed that the staff were more knowledgeable about food insecurity and began referring their food-insecure patients to resources (Smith et al., 2017). One of its residency programs included the two-item tool into their electronic health records. In this system, positive screens generate an ICD-10 code for food insecurity and create referrals to the local food pantries and on-site SNAP application. Moreover, a successful program in Orange County, California educates food businesses about donating excess food and connects food-insecure individuals to food pantries. Once patients at the Children’s Hospital of Orange County and Family Resource Center are identified as positive, they can utilize the program’s interactive Google Map pantry directory to find pantries closest to their home (Garcia-Silva et al., 2017).
Unsurprisingly, the responses from our focus group are consistent with findings from other studies. Medical students, residents, and faculty at UCSD felt that screening for patients, particularly those of low-income, at risk for food insecurity was important even though very few had actually executed the screening or made referrals (Smith et al., 2017). This was similar to our findings with our focus group of pediatricians. A common theme from our study and that of other researchers was that many practitioners are uncertain how to handle positive screens and that caregivers or patients are reluctant to identify themselves as food-insecure due to stigma.
Despite these perceived barriers, there are some suggestions for overcoming them. The Knowles et al study found the following factors which facilitated screening and referral: having a strong, trusting relationship with the practitioner and receiving assistance in navigating government benefit application centers as they are perceived as confusing and intimidating (2018). Furthermore, patient comfort that is developed over time with repeated screening may help to screen in the context of sensitive topics such as food insecurity and domestic violence (Barnidge et al., 2017).
This study has several limitations. Firstly, we do not know if these respondents already receive SNAP benefits or visit food pantries—this may affect their food security status. Moreover, considering that FQHCs serve medically underserved patients, most are of low socioeconomic status and may have low literacy which can affect the form of survey administration and the positive screen rate (Palakshappa et al., 2019, Smith et al., 2016). In the Palakshappa study it was found that written surveys obtained higher rates of positive screens for those at risk for food insecurity than surveys conducted verbally (2019). This could mean that our screening tool which was administered verbally may have a lower than expected number of households at risk for food insecurity. In regards to the focus group, the researchers conducted the interview, which may introduce respondent bias. However, there was no demographic information obtained or any financial or material incentive for the participants to answer the questions in a particular manner.
We encountered a few challenges and barriers prior to this study. Another FQHC and a private pediatric office initially agreed to use the two-item screening tool and administered it by paper. However, we were not able to obtain a sufficient amount of responses compared to that at the CSHHC, which used a “champion” and administered the two-item screening as part of its electronic health record. It appears that using an electronic health system to implement the survey tool and incorporating it as part of the intake process ensures consistency and thus a high screening rate. The medical staff at the other three clinics reported forgetfulness and very busy schedules with other competing priorities as obstacles to obtaining a high screening rate. Moreover, we have encountered some health professionals who refused to administer the survey—for instance, one believed that asking these questions may offend patients who are not of low socioeconomic status.
Given the identified barriers, key actions include: (i) embarking on a public awareness campaign to educate the general public about how significant this problem is and its health implications, (ii) addressing the stigma by talking about it and working collaboratively to show how common food insecurity is in America and what makes people vulnerable to food insecurity, (iii) encouraging all health professionals to screen regardless of patient population and demographics, (iv) advocating for policy change to implement screening for each patient as well as provide incentives and monitor compliance, and (v) providing technical assistance, such as provider trainings and information on local food resources. We prefer the two-item screening tool as it has the least respondent burden in terms of time spent and high sensitivity value. Most importantly, implementing the tool into electronic health records resulted in a practice to ensure consistency and easier data collection rather than administering the screening tool using a paper form. The use of an electronic screening tool was the main contributor to our large sample size. We recommend integrating this screening tool into practice as part of a standard assessment or history. We also observed that a practice champion who advocates daily execution of the survey is important. Once patients are identified as food insecure, it is crucial to make referrals to food resources and discuss other viable options.
5. Conclusion
We highly recommend the use of the validated two-item screening tool for identifying food-insecure individuals and households as it has low respondent burden. Moreover, healthcare providers agree that addressing food insecurity is an important issue as low-quality diet leads to chronic health conditions. As patient stigma and practitioners’ uncertainty of how to direct food-insecure patients persist, more education and training in screening for food insecurity is required.
CRediT authorship contribution statement
Martha Okafor: Conceptualization, Methodology, Investigation, Resources, Writing - review & editing, Visualization, Supervision. Sarah Wing-Yin Chiu: Conceptualization, Investigation, Writing - original draft, Writing - review & editing. Richard Feinn: Formal analysis, Data curation, Writing - review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We would like to thank Michael Taylor, Dr. Bruce Douglas, MD, and Dr. Ece Tek, MD of Cornell Scott-Hill Health Center for facilitating the process of implementing the screening tool into the electronic health record system. Moreover, Tasha Hamblin of CSHHC helped to organize the respondent data. We would like to thank Jillian Wood and Dr. Anton Alerte, MD of the Connecticut Chapter of the American Academy of Pediatrics for the advice and for making the focus group possible. Finally, we appreciate Joy Johannes and Dr. Sandra Carbonari, MD for their insight. We have received permission from those named in the acknowledgement.
Contributor Information
Martha Okafor, Email: martha.okafor@yale.edu.
Sarah Chiu, Email: sarah.w.chiu@kp.org.
Richard Feinn, Email: Richard.Feinn@quinnipiac.edu.
References
- Barnidge E., LaBarge G., Krupsky K., Arthur J. Screening for food insecurity in pediatric clinical settings: opportunities and barriers. J. Community Health. 2017;42(1):51–57. doi: 10.1007/s10900-016-0229-z. [DOI] [PubMed] [Google Scholar]
- Carter N., Bryant-Lukosius D., DiCenso A., Blythe J., Neville A.J. The use of triangulation in qualitative research. Oncol. Nurs. Forum. 2014;41(5):545–547. doi: 10.1188/14.ONF.545-547. [DOI] [PubMed] [Google Scholar]
- Farmer T., Robinson K., Elliot S.J., Eyles J. Developing and implementing a triangulation protocol for qualitative health research. Qual. Health Res. 2006;16(3):377–394. doi: 10.1177/1049732305285708. [DOI] [PubMed] [Google Scholar]
- Garcia-Silva B., Handler E., Wolfe J. A public-private partnership to mitigate food insecurity and food waste in Orange County, California. Am. J. Public Health. 2017;107(1):105–107. doi: 10.2105/AJPH.2016.303450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gundersen C., Engelhard E.E., Crumbaugh A.S., Seligman H.K. Brief assessment of food insecurity accurately identifies high-risk US adults. Public Health Nutr. 2017;20(8):1367–1371. doi: 10.1017/S1368980017000180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hager E.R., Quigg A.M., Black M.M., Coleman S.M., Heeren T., Rose-Jacobs R., Frank D.A. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. 2010;126(1):e26–e32. doi: 10.1542/peds.2009-3146. [DOI] [PubMed] [Google Scholar]
- Knowles M., Khan S., Palakshappa D., Cahill R., Kruger E., Poserina B.G., Chilton M. Successes, challenges, and considerations for integrating referral into food insecurity screening in pediatric settings. J. Health Care Poor Underserved. 2018;29(1):181–191. doi: 10.1353/hpu.2018.0012. [DOI] [PubMed] [Google Scholar]
- Makelarski J.A., Abramsohn E., Benjamin J.H., Du S., Lindau S.T. Diagnostic accuracy of two food insecurity screeners recommended for use in health care settings. Am. J. Public Health. 2017;107(11):1812–1817. doi: 10.2105/AJPH.2017.304033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel M.L., Klein L.R., Hager K.A., Cutts D.B. Emergency department experience with novel electronic medical record order for referral to food resources. Western J. Emergency Med. 2018;19(2):232–237. doi: 10.5811/westjem.2017.12.35211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- New Haven: New Haven County, Connecticut. (2018). Retrieved from http://www.ctdatahaven.org/profiles/new-haven.
- O’Keefe, L. Identifying food insecurity: Two-question screening tool has 97% sensitivity. (2015). Retrieved from http://www.aappublications.org/content/early/2015/10/23/aapnews.20151023-1.
- Palakshappa D., Goodpasture M., Albertini L., Brown C.L., Montez K., Skelton J. Written vs verbal food insecurity screening in one primary care clinic. Academic Pediatrics. 2019;20(2):203–207. doi: 10.1016/j.acap.2019.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Promoting food security for all children. (2018). Pediatrics, 136(5), September 24, 2018. [DOI] [PubMed]
- Saiz A.M., Aul A.M., Malecki K.M., Bersch A.J., Bergmans R.S., LeCaire T.J., Nieto F.J. Food insecurity and cardiovascular health: Findings from a statewide population health survey in Wisconsin. Prev. Med. 2016;93:1–6. doi: 10.1016/j.ypmed.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligman H.K., Laraia B.A., Kushel M.B. Food insecurity is associated with chronic disease among low-income NHANES participants. J. Nutr. 2010;140(2):304–310. doi: 10.3945/jn.109.112573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith S., Malinak D., Chang J., Perez M., Perez S., Settlecowski E., Aedo S. Implementation of a food insecurity screening and referral program in student-run free clinics in San Diego, California. Preventive Medicine Reports. 2016;5:134–139. doi: 10.1016/j.pmedr.2016.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith S., Malinak D., Chang J., Schultz A., Brownell K. Addressing food insecurity in family medicine and medical education. Fam. Med. 2017;49(10):765–771. [PubMed] [Google Scholar]
- Starr M.C., Fisher K., Thompson K., Thurber-Smith K., Hingorani S. A pilot investigation of food insecurity among children seen in an outpatient pediatric nephrology clinic. Preventive Medicine Reports. 2018;10:113–116. doi: 10.1016/j.pmedr.2018.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United states department of agriculture: Household food security in the United States in 2018. (2019). Retrieved from https://www.ers.usda.gov/webdocs/publications/94849/err270_summary.pdf?v=4515.2.
- United states department of agriculture economic research service: Survey tools. (2019). Retrieved from https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/survey-tools/.