Abstract
Purpose
This is a retrospective single-institution study performed to compare the rate of unnecessary operations in pregnant women with suspected acute appendicitis with and without the use of MRI.
Methods
The study subjects were all pregnant women with suspected acute appendicitis admitted to a tertiary institution from January 2012 to December 2019. If acute appendicitis was not excluded clinically and by ultrasound (US), laparoscopies were performed until May 2017 (US-only group). MRI was added as a diagnostic tool when US was inconclusive from May 2017 (US + MRI group). Surgery was considered unnecessary when no inflamed appendix was found. The rate of unnecessary surgery, postoperative complications, length of stay were analyzed.
Results
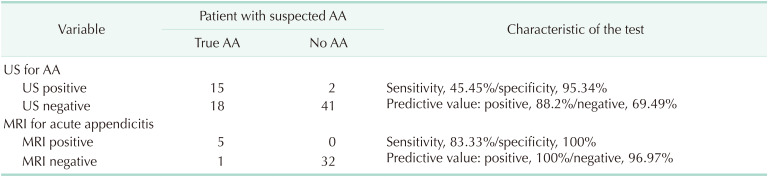
Seventy-six women were included in the study; 38 women in the US-only group and 38 women in the US + MRI group. There were no differences in admission characteristics between the groups. One of 38 women (2.6%) underwent unnecessary surgery in the US + MRI group vs. 10 of 38 (26.3%) in the US-only group (P = 0.007). The patients in the US + MRI group were significantly less likely to undergo a diagnostic operation than in the US-only group (5.26% vs. 55.3%, respectively; P < 0.001) and their hospital stay was significantly shorter (0.74 ± 1.64 days vs. 3.7 ± 3.0 days, respectively; P < 0.001). The obstetric outcomes were not different between the groups. MRI had a sensitivity of 83.3% and specificity of 100% in the series.
Conclusion
The rate of unnecessary surgery was significantly reduced in pregnant women, who underwent MRI after inconclusive transabdominal US.
Keywords: Appendicitis, Diagnostic imaging, Magnetic resonance imaging, Pregnancy
INTRODUCTION
Acute appendicitis is an important diagnostic problem worldwide—up to 27 percent of patients, especially women, undergo unnecessary operations even in some highly-developed countries [1,2]. Acute appendicitis is also the most common surgical disease in pregnant women. It occurs in about 1 in 500 to 1 in 635 pregnancies per year [3], most commonly during the second and third trimesters [4,5,6,7]. Appendicitis in pregnancy is associated with an almost 2–fold increase in sepsis and septic shock, transfusion, pneumonia, bowel obstruction, postoperative infection, and length of stay of more than 3 days [8]. The diagnosis is more difficult during pregnancy; the location of the pain of appendicitis changes with the enlarged uterus displacing the appendix and the leukocytosis may be physiological. These factors may delay the diagnosis of acute appendicitis or mimic other common disorders [3,9,10]. Incorrect preoperative diagnosis results in unnecessary operations. The surgery itself can increase the risk of unfavorable outcomes in pregnant women [11], including increased rates of premature labor (15%–45%) and fetal loss [12], as well as harm the newborn [13].
Ultrasound (US) is the first-line diagnostic modality in pregnant women [14]. However, the majority of the scans are inconclusive or the appendix is not visualized [15]. MRI is a proven diagnostic modality for acute appendicitis and suitable in women after the first trimester [3], and it should theoretically reduce the rate of unnecessary (diagnostic) operations in pregnant women.
The aim of our study was to compare the rate of unnecessary (diagnostic) operations in pregnant women with clinically suspected acute appendicitis with and without the use of MRI.
METHODS
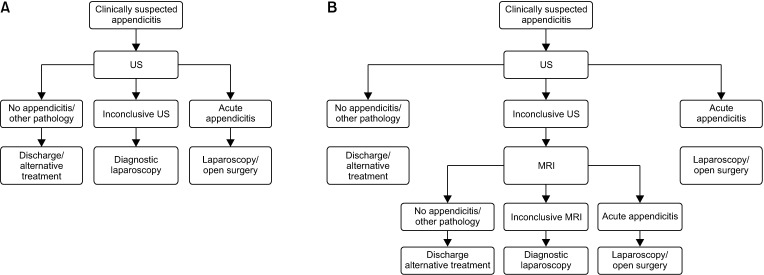
This is a retrospective single-institution study, performed at the Vilnius University Hospital Santara Clinics, Vilnius, Lithuania. All pregnant women admitted with suspected acute appendicitis at this tertiary institution were included in the study from January 2012 to December 2019. All women underwent transabdominal US in addition to the standard clinical and laboratory investigation. If acute appendicitis was not excluded clinically and by the US, laparoscopies were performed until May 2017. MRI was added as a diagnostic tool when US was inconclusive from May 2017 (Fig. 1).
Fig. 1. Diagnostic algorithms or pregnant women with suspected acute appendicitis. Before (A) and after (B) introduction of MRI. US, ultrasound.
The data on all the patients undergoing investigation for acute abdominal pain were entered into a prospectively maintained database. The database was reviewed retrospectively to identify all known pregnant patients with suspected acute appendicitis. Patients, who underwent MRI after an inconclusive US formed the study group (US + MRI group). Patients, who did not undergo MRI formed the control group (US-only group). Patient charts were reviewed for detailed demographic, clinical, laboratory, radiology, and surgical characteristics. The data were compared between the groups. Surgery was considered unnecessary when no inflamed appendix was found.
Obstetric outcomes are available for women who gave birth in the same hospital. The data was retrieved from the obstetric patient charts. The regional bioethics committee in Vilnius approved the study (No. 2019/3-1107-610). The written patient consent was received.
Categorical variables are expressed as frequencies and percentages and continuous variables as means and standard deviations. Categorical data between the groups were compared by chi-square or Fisher exact test as appropriate. Continuous characteristics were compared by Student t-test or the Mann-Whitney U-test as appropriate. All differences for which the P-value was less than 0.05 were considered to be significant. The data were analyzed with IBM SPSS Statistics ver. 23 (IBM Corp., Armonk, NY, USA).
RESULTS
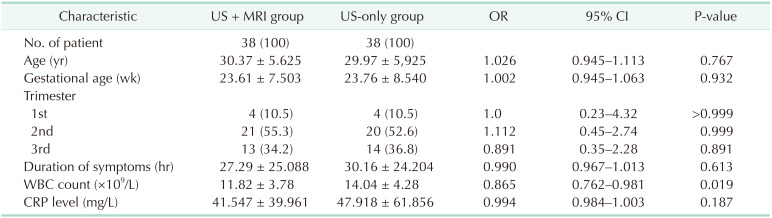
Seventy-six women were included in the study. There were 38 women in the US-only group and 38 women in the US + MRI group. The comparison of the characteristics of the groups on admission is presented in Table 1. There were no differences in admission characteristics between the groups.
Table 1. Characteristics of the patient groups on admission.
Values are presented as number (%) or mean ± standard deviation.
US, ultrasound; OR, odds ratio; CI, confidence interval.
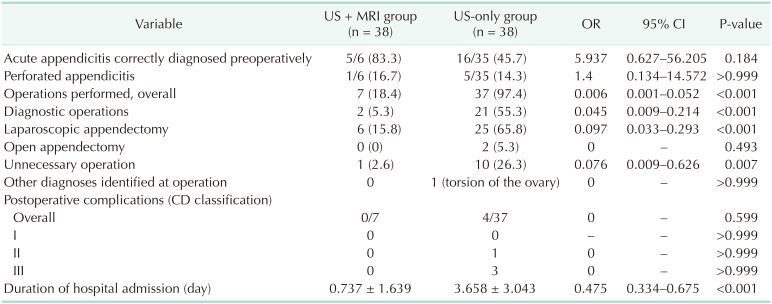
There were 11 unnecessary operations (14.5%): 3 women (7.9%) underwent diagnostic laparoscopy, 3 (7.9%) underwent laparoscopic appendectomy with normal-looking appendix, and 5 (13.2%) underwent open appendectomy with normallooking appendix. One of the 38 women (2.6%) underwent unnecessary surgery in the US + MRI group and 10 of 38 (26.3%) in the US-only group (P = 0.007) (Table 2). The judgment of surgery as unnecessary was based on pathologic findings. Surgical treatment was needed for patients with gangrenous appendicitis (n = 7), perforated appendicitis (n = 6), phegmonous appendicitis (n = 20), and unnecessary with appendicitis catarrhalis (n = 5), appendix without changes (n = 3). There was no information about the pathologic findings for 3 patients who underwent unnecessary surgery. The patients in the US + MRI group were significantly less likely to undergo a diagnostic operation than in the US-only group (5.3% vs. 55.3%, respectively; P < 0.001) and their hospital stay was significantly shorter (0.74 ± 1.64 days vs. 3.7 ± 3.0 days, respectively; P < 0.001). The incidence of perforated appendicitis was not different between the groups (16.7% vs. 14.3%; P > 0.999).
Table 2. Results of treatment.
Values are presented as number (%), number only, or mean ± standard deviation.
OR, odds ratio; CI, confidence interval; –, not applicable; CD, Clavien-Dindo.
For the patients who did not undergo surgery after MRI with normal appendix, the most common cause of abdominal pain was other unspecified abdominal pain (9 of 31 patients) and functional bowel disorder (8 of 31). Other diagnoses were also seen such as hydronephrosis (4 of 31), false labor before 37 pregnancy weeks (3 of 31), Crohn disease (2 of 31), gastroenterocolitis, functional dyspepsia, ovary cyst, urogenital infection, and metastatic gastric adenocarcinoma.
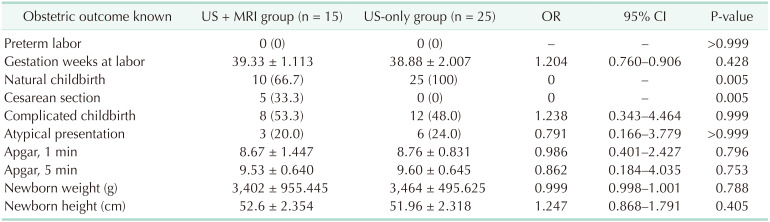
The obstetric outcomes are available for 41 women (53.9%). No adverse obstetric outcomes occurred within the index hospital admission (Table 3). Also, no major adverse obstetric outcomes were identified for the patients in the study. There was no difference between the US + MRI and US-only groups of patients.
Table 3. Obstetric outcomes.
Values are presented as number (%) or mean ± standard deviation.
OR, odds ratio; CI, confidence interval; –, not applicable.
The overall results of the radiological investigations are presented in Table 4. MRI has excellent sensitivity and specificity in pregnant women with suspected acute appendicitis, in whom transabdominal US is inconclusive.
Table 4. The results of the radiology tests for the diagnosis of acute appendicitis (AA) in pregnant patients.
US, ultrasound.
DISCUSSION
We found, that the rate of unnecessary (diagnostic) surgery was significantly higher in pregnant women who did not undergo MRI. It did not translate into the increased rate of perforated appendicitis, which could be expected due to the delay in surgery or to the increased number of complications. We also found that MRI is an effective test in pregnant women in whom transabdominal US is inconclusive. The transabdominal US can correctly diagnose acute appendicitis in 19.7% of pregnant women. We did not find any increased risk of worse obstetric outcomes in either group of patients.
Clinical and laboratory findings in pregnant women with suspected acute appendicitis are not specific. The most common clinical features in patients with confirmed acute appendicitis were similar to the findings in the literature; nausea/vomiting (29 of 42, 69.0%) and painful palpation (42 of 42, 100%) [16]. All women in our study had elevated WBC count and CRP count. It is widely known that the WBC count increases to a normal 10,000 to 14,000 cells/mm3 during pregnancy [17].
On US, the appendix is visualized as a tubular blind-ending structure arising from the ileocolic region, in the case of an acute appendicitis appendix is noncompressible, the diameter is >6 mm, walls are thickened (>2 mm), “target” appearance on the axial plane (hypoechoic fluid-filled lumen, hyperechoic mucosa/submucosa, hypoechoic muscular layer), might have appendicolith in the lumen that is usually hyperechoic. Usually, there are also some secondary findings as hyperechoic (inflamed) surrounding mesenteric fat, a small amount of free fluid, few enlarged (>5 mm) lymph nodes or inflammatory changes of bowel walls or peritoneum [18]. On MRI findings are similar; appendix diameter is 7 mm or lager, there will be seen thickened walls that might have a hyperintense signal on T2 fat-suppressed sequence, the lumen might be filled with liquid or stool that have different signal intensity on MRI, also there will be seen some secondary findings in surrounding tissues, infiltration of surrounding fatty tissue, free liquid, lymph nodes, or reactive changes of bowels [19].
Our results are quite similar to other studies conducted recently which show the sensitivity of MRI of 54%–99% and specificity of 87%–99%; with a positive predictive value of 61% and a negative predictive value of 100% [15,20,21,22,23]. All studies agree, that if clinical and US findings are inconclusive, MRI is indicated given that it does not expose the fetus to ionizing radiation and has performed well in the diagnosis of acute appendicitis.
We found that MRI significantly reduces the rate of unnecessary operations and surgery overall in pregnant women. This is similar to other reports [23]. In situations where MRI could not be performed, a low-dose CT with oral contrast could be a second line of imaging after inconclusive US [24]. Even though CT has high sensitivity and specificity for diagnosing acute appendicitis, concern about ionizing radiation which is delivered to the fetus is significant. MRI remains a second-line diagnostic tool, which provides a systemic evaluation of the abdomen, lowers the rate of unnecessary operations, and reduces the perforation rate [25].
The effectiveness of US remains debatable. Some studies claim that US is a sufficient diagnostic method for acute appendicitis, while others show that transabdominal US has low sensitivity and specificity compared to MRI or CT. Although US has a fairly high positive predictive value, the low negative predictive value shows that US cannot be relied on to eliminate an acute appendicitis diagnosis [25]. US is a useful and safe tool to correctly diagnose at least 20% of women with suspected acute appendicitis.
Even though implementing MRI increases medical costs compared to CT or US, it is the most cost-effective strategy for pregnant patients after inconclusive US and should be used as a preoperative imaging tool [26].
Our study included pregnant patients mostly in the second and third trimesters. We did not observe any instances of pregnancy loss or premature labor. Studies confirm that most of the pregnancy losses occur in patients with diagnosed appendicitis at gestational age less than 24 weeks [12]. Adverse obstetric outcomes are also associated with delayed diagnosis and unnecessary laparoscopies [27].
Most of the women in our study underwent laparoscopic appendectomy or diagnostic laparoscopy. It has been shown, that a laparoscopic approach results in less morbidity than an open appendectomy; unfortunately, it is not available in all countries [28]. Laparoscopic surgery has been recommended as a technique of choice in pregnant women with acute appendicitis when adequate experience was available [29].
The main strength of our study is the relatively large number of patients included in the study. It is difficult to prospectively collect a large study group of pregnant patients, undergoing emergency investigations and surgery due to ethical concerns. Our study is one of the largest series of patients in the literature [20,30]. Even within this relatively small cohort, the impact of additional MRI testing is highly significant.
The main limitations of the study are the retrospective design and single-center study settings. Transabdominal US is very operator-dependent; MRI is not available during the night or weekends or freely anytime in most institutions.
MRI represents an excellent modality for the correct diagnosis of acute appendicitis in pregnant women. It could be included in the diagnostic protocols in cases when US is inconclusive. Nevertheless, further studies with larger numbers of patients will be helpful to more accurately identify the benefit of MRI in diagnosing acute appendicitis in pregnant patients.
In conclusion, the rate of unnecessary surgery was significantly reduced in pregnant women who underwent MRI after inconclusive transabdominal US. This was not associated with an increased risk of surgical or obstetric complications. MRI has a significant diagnostic value of correctly identify acute appendicitis. However, retrospective and prospective studies should be scope for further research to assess a more accurate utilization of this method.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
- Conception or design of the work: TP, RL, SM.
- Acquisition, analysis, or interpretation of data for the work: All authors.
- Writing — Original Draft: BL.
- Writing — Review & Editing: All authors.
References
- 1.Kryzauskas M, Danys D, Poskus T, Mikalauskas S, Poskus E, Jotautas V, et al. Is acute appendicitis still misdiagnosed? Open Med (Wars) 2016;11:231–236. doi: 10.1515/med-2016-0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhangu A RIFT Study Group on behalf of the West Midlands Research Collaborative. Evaluation of appendicitis risk prediction models in adults with suspected appendicitis. Br J Surg. 2020;107:73–86. doi: 10.1002/bjs.11440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kave M, Parooie F, Salarzaei M. Pregnancy and appendicitis: a systematic review and meta-analysis on the clinical use of MRI in diagnosis of appendicitis in pregnant women. World J Emerg Surg. 2019;14:37. doi: 10.1186/s13017-019-0254-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Wilde JP, Rivers AW, Price DL. A review of the current use of magnetic resonance imaging in pregnancy and safety implications for the fetus. Prog Biophys Mol Biol. 2005;87:335–353. doi: 10.1016/j.pbiomolbio.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 5.Mourad J, Elliott JP, Erickson L, Lisboa L. Appendicitis in pregnancy: new information that contradicts long-held clinical beliefs. Am J Obstet Gynecol. 2000;182:1027–1029. doi: 10.1067/mob.2000.105396. [DOI] [PubMed] [Google Scholar]
- 6.Dewhurst C, Beddy P, Pedrosa I. MRI evaluation of acute appendicitis in pregnancy. J Magn Reson Imaging. 2013;37:566–575. doi: 10.1002/jmri.23765. [DOI] [PubMed] [Google Scholar]
- 7.Oto A, Srinivasan PN, Ernst RD, Koroglu M, Cesani F, Nishino T, et al. Revisiting MRI for appendix location during pregnancy. AJR Am J Roentgenol. 2006;186:883–887. doi: 10.2214/AJR.05.0270. [DOI] [PubMed] [Google Scholar]
- 8.Abbasi N, Patenaude V, Abenhaim HA. Management and outcomes of acute appendicitis in pregnancy-population-based study of over 7000 cases. BJOG. 2014;121:1509–1514. doi: 10.1111/1471-0528.12736. [DOI] [PubMed] [Google Scholar]
- 9.Tinoco-González J, Rubio-Manzanares-Dorado M, Senent-Boza A, Durán-Muñoz-Cruzado V, Tallón-Aguilar L, Pareja-Ciuró F, et al. Acute appendicitis during pregnancy: differences in clinical presentation, management, and outcome. Emergencias. 2018;30:261–264. [PubMed] [Google Scholar]
- 10.Tamir IL, Bongard FS, Klein SR. Acute appendicitis in the pregnant patient. Am J Surg. 1990;160:571–576. doi: 10.1016/s0002-9610(05)80748-2. [DOI] [PubMed] [Google Scholar]
- 11.Prodromidou A, Machairas N, Kostakis ID, Molmenti E, Spartalis E, Kakkos A, et al. Outcomes after open and laparoscopic appendectomy during pregnancy: a meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2018;225:40–50. doi: 10.1016/j.ejogrb.2018.04.010. [DOI] [PubMed] [Google Scholar]
- 12.Theilen LH, Mellnick VM, Shanks AL, Tuuli MG, Odibo AO, Macones GA, et al. Acute appendicitis in pregnancy: predictive clinical factors and pregnancy outcomes. Am J Perinatol. 2017;34:523–528. doi: 10.1055/s-0036-1593764. [DOI] [PubMed] [Google Scholar]
- 13.Jakubauskiene L, Jakubauskas M, Mainelis A, Buzinskiene D, Drasutiene G, Ramasauskaite D, et al. Factors influencing quality of life during the first trimester of pregnancy: a prospective cohort study. Medicina (Kaunas) 2019;55:666. doi: 10.3390/medicina55100666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tremblay E, Thérasse E, Thomassin-Naggara I, Trop I. Quality initiatives: guidelines for use of medical imaging dur ing pregnancy and lactat ion. Radiographics. 2012;32:897–911. doi: 10.1148/rg.323115120. [DOI] [PubMed] [Google Scholar]
- 15.Burke LM, Bashir MR, Miller FH, Siegelman ES, Brown M, Alobaidy M, et al. Magnetic resonance imaging of acute appendicitis in pregnancy: a 5-year multiinstitutional study. Am J Obstet Gynecol. 2015;213:693. doi: 10.1016/j.ajog.2015.07.026. [DOI] [PubMed] [Google Scholar]
- 16.Brown JJ, Wilson C, Coleman S, Joypaul BV. Appendicitis in pregnancy: an ongoing diagnostic dilemma. Colorectal Dis. 2009;11:116–122. doi: 10.1111/j.1463-1318.2008.01594.x. [DOI] [PubMed] [Google Scholar]
- 17.Sanci M, Töz E, Ince O, Özcan A, Polater K, Inan AH, et al. Reference values for maternal total and differential leukocyte counts in different trimesters of pregnancy and the initial postpartum period in western Turkey. J Obstet Gynaecol. 2017;37:571–575. doi: 10.1080/01443615.2016.1268575. [DOI] [PubMed] [Google Scholar]
- 18.Mostbeck G, Adam EJ, Nielsen MB, Claudon M, Clevert D, Nicolau C, et al. How to diagnose acute appendicitis: ultrasound first. Insights Imaging. 2016;7:255–263. doi: 10.1007/s13244-016-0469-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spalluto LB, Woodfield CA, DeBenedectis CM, Lazarus E. MR imaging evaluation of abdominal pain during pregnancy: appendicitis and other nonobstetric causes. Radiographics. 2012;32:317–334. doi: 10.1148/rg.322115057. [DOI] [PubMed] [Google Scholar]
- 20.Patel D, Fingard J, Winters S, Low G. Clinical use of MRI for the evaluation of acute appendicitis during pregnancy. Abdom Radiol (NY) 2017;42:1857–1863. doi: 10.1007/s00261-017-1078-7. [DOI] [PubMed] [Google Scholar]
- 21.Oto A, Ernst RD, Ghulmiyyah LM, Nishino TK, Hughes D, Chaljub G, et al. MR imaging in the triage of pregnant patients with acute abdominal and pelvic pain. Abdom Imaging. 2009;34:243–250. doi: 10.1007/s00261-008-9381-y. [DOI] [PubMed] [Google Scholar]
- 22.Tsai R, Raptis C, Fowler KJ, Owen JW, Mellnick VM. MRI of suspected appendicitis during pregnancy: interradiologist agreement, indeterminate interpretation and the meaning of non-visualization of the appendix. Br J Radiol. 2017;90:20170383. doi: 10.1259/bjr.20170383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burns M, Hague CJ, Vos P, Tiwari P, Wiseman SM. Utility of magnetic resonance imaging for the diagnosis of appendicitis during pregnancy: a Canadian experience. Can Assoc Radiol J. 2017;68:392–400. doi: 10.1016/j.carj.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 24.Poletti PA, Botsikas D, Becker M, Picarra M, Rutschmann OT, Buchs NC, et al. Suspicion of appendicitis in pregnant women: emergency evaluation by sonography and low-dose CT with oral contrast. Eur Radiol. 2019;29:345–352. doi: 10.1007/s00330-018-5573-1. [DOI] [PubMed] [Google Scholar]
- 25.Aggenbach L, Zeeman GG, Cantineau AE, Gordijn SJ, Hofker HS. Impact of appendicitis during pregnancy: no delay in accurate diagnosis and treatment. Int J Surg. 2015;15:84–89. doi: 10.1016/j.ijsu.2015.01.025. [DOI] [PubMed] [Google Scholar]
- 26.Kastenberg ZJ, Hurley MP, Luan A, Vasu-Devan V, Spain DA, Owens DK, et al. Cost-effectiveness of preoperative imaging for appendicitis after indeterminate ultrasonography in the second or third trimester of pregnancy. Obstet Gynecol. 2013;122:821–829. doi: 10.1097/AOG.0b013e3182a4a085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McGory ML, Zingmond DS, Tillou A, Hiatt JR, Ko CY, Cryer HM. Negative appendectomy in pregnant women is associated with a substantial risk of fetal loss. J Am Coll Surg. 2007;205:534–540. doi: 10.1016/j.jamcollsurg.2007.05.025. [DOI] [PubMed] [Google Scholar]
- 28.GlobalSurg Collaborative. Laparoscopy in management of appendicitis in high-, middle-, and low-income countries: a mulBeatrice ticenter, prospective, cohort study. Surg Endosc. 2018;32:3450–3466. doi: 10.1007/s00464-018-6064-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ball E, Waters N, Cooper N, Talati C, Mallick R, Rabas S, et al. Evidence-based guideline on laparoscopy in pregnancy: commissioned by the British Society for Gynaecological Endoscopy (BSGE) Endorsed by the Royal College of Obstetricians & Gynaecologists (RCOG) Facts Views Vis Obgyn. 2019;11:5–25. [PMC free article] [PubMed] [Google Scholar]
- 30.Wi SA, Kim DJ, Cho ES, Kim KA. Diagnostic performance of MRI for pregnant patients with clinically suspected appendicitis. Abdom Radiol (NY) 2018;43:3456–3461. doi: 10.1007/s00261-018-1654-5. [DOI] [PubMed] [Google Scholar]