Figure 4. Representative case of an early in‐stent calcified nodule in a patient undergoing dialysis.
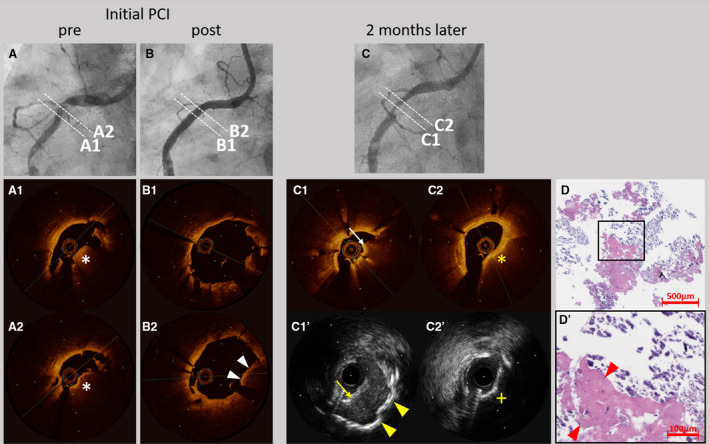
A 43‐year‐old man undergoing dialysis received everolimus‐eluting stents in the right coronary artery (RCA) for stable angina. Coronary angiography results before (A) and after (B) stent implantation are presented. Optical coherence tomography (OCT) showed a high‐backscattering protruding mass with signal attenuation suggesting the calcified nodule (white asterisks) (A1 and A2). In addition, OCT demonstrated the protrusion of the calcified nodule (white arrow heads) after stent implantation (B1 and B2). Two months later, the patient underwent coronary angiography for symptoms of unstable angina pectoris. Coronary angiography (C) revealed in‐stent restenosis in the RCA. OCT (C1) showed a red thrombus (white arrow), while intravascular ultrasound (C1’) showed a thrombus (yellow arrow) and sheet calcification at the bottom (yellow arrow heads). OCT (C2) demonstrated attenuations (yellow asterisk) and intravascular ultrasound (C2’) demonstrated acoustic shadow (yellow cross) suggesting the presence of the calcified nodule. Low‐ (D) and high‐ (D’) power images of the tissue collected through directional coronary atherectomy revealed the calcified nodule with fibrin deposition (red arrow heads). PCI indicates percutaneous coronary intervention.
