The call for revisiting incremental hemodialysis for patients with incident kidney failure was first introduced in the United States over half a decade ago (1). It was argued that because the progression of CKD (i.e., regression of residual kidney function [RKF]) is usually gradual, over a matter of months to years, transition to dialysis therapy should be incremental and follow a reverse mirror image of RKF, starting with lower-clearance hemodialysis prescriptions and building up to higher-clearance hemodialysis regimens (Figure 1). When used in clinical practice, the most frequently considered form of incremental hemodialysis is less-frequent hemodialysis with prescription schedules of twice-weekly or once-a-week hemodialysis, with the latter regimen being less commonly prescribed in the United States. In 2014, an expert opinion paper (1) argued that the mortality rate in patients who transition from predialysis CKD to incident kidney failure is highest in the first months of hemodialysis therapy and that the outright initiation with a thrice-weekly or more frequent hemodialysis regimen, by virtue of causing faster decline in RKF, might be a cause of this sudden surge in death. Some but not all data suggest that, relative to less-frequent incremental hemodialysis, RKF declines more rapidly with thrice-weekly hemodialysis treatments, and longer preservation of RKF is associated with greater patient longevity. Because RKF provides a reduced need for dialytic solute clearance, and given that it is an important factor to account for in the prescription of peritoneal dialysis, it is insensible to have a discrepant approach devoid of RKF when calculating the target dialysis adequacy in patients on hemodialysis (1).
Figure 1.
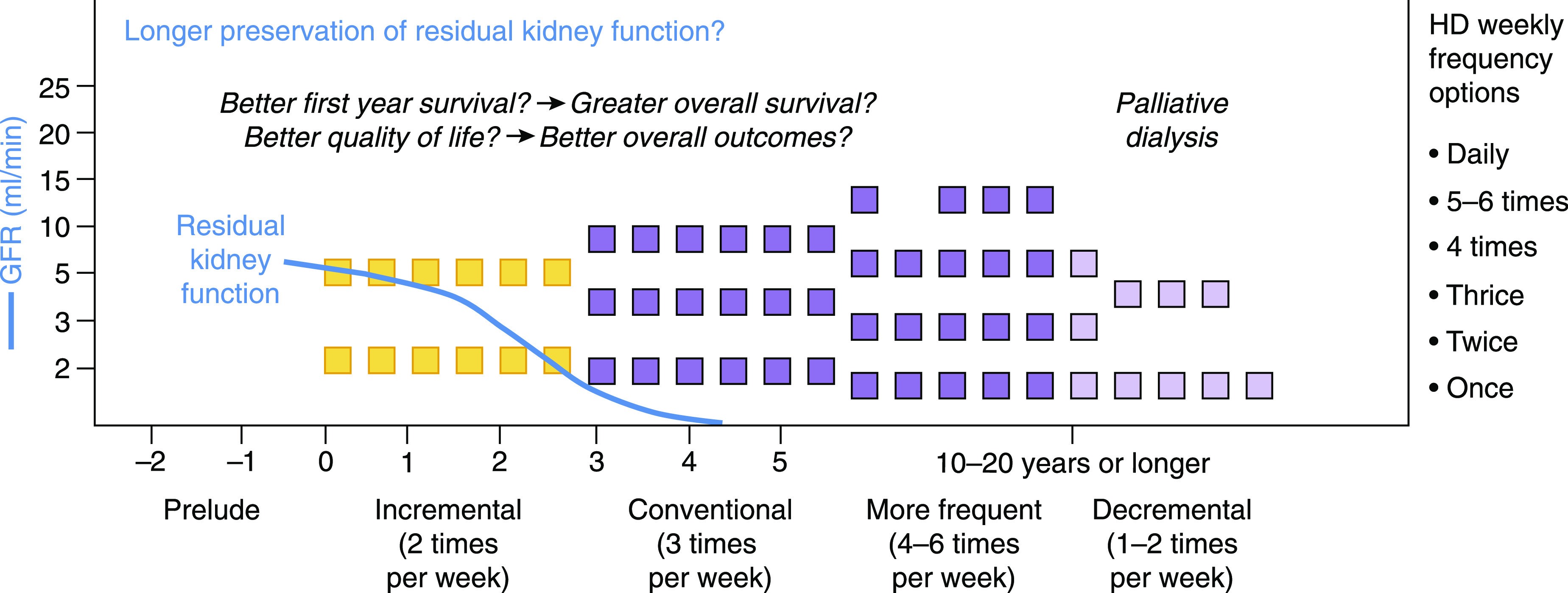
Schematic representation of the incremental dialysis program with twice-weekly hemodialysis (HD) initiation. Each block represents a weekly HD therapy. Blocks in yellow represent the period of incremental transition to twice-weekly HD, whereas dark violet blocks illustrate increase in dialysis frequency to thrice weekly or more frequently as needed. Light violet blocks highlight the transition to a palliative dialysis protocol with less-frequent HD therapy. Adapted from ref. 2, with permission.
The incremental dialysis expert opinion paper (1) suggested ten criteria for an incremental transition to dialysis, the leading one being adequate RKF upon dialysis transition in the form of a daily urine volume of at least 600 ml/d and a native kidney urea clearance (Kru) of at least 3 ml/min. It was suggested that a patient is eligible for twice-weekly hemodialysis if he or she meets the said RKF criterion plus five or more (of nine) other criteria (i.e., intradialytic weight gain <2.5 kg; stable cardiovascular status; infrequent hospitalization; satisfactory health-related quality of life; small to normal body size; good nutritional status; and absence of hyperkalemia, hyperphosphatemia, or profound anemia) (1). The 2006 Kidney Disease Outcomes Quality Initiative (KDOQI) Work Group recommended a twice-weekly dialysis schedule among patients with “substantial RKF” defined as those with a Kru>3 ml/min (3). Each individual’s RKF should be assessed on a monthly to quarterly basis, and after the urine volume is <0.5 L/d or Kru<2 ml/min, the hemodialysis prescription should be changed from twice weekly to thrice weekly to complement the decline in RKF. However, these threshold levels are mostly arbitrary, and in some observational studies, including from China (4) and South Korea (5), the outcomes of incremental dialysis of twice versus thrice weekly were not affected by presence or absence of RKF.
In late 2014, the University of California Irvine initiated implementing incremental hemodialysis transition in select patients with incident kidney failure who met the above criteria (6). Since the inception of the incremental program, the patients on the regimen of twice-weekly hemodialysis have been followed for their RKF trends and clinical outcomes. The preliminary data from the first 13 patients on twice-weekly incremental hemodialysis showed that five patients maintained a twice-weekly hemodialysis schedule for more than a year, whereas eight patients transitioned to thrice-weekly hemodialysis regimen within the first 12 months; the main causes of incremental transition from twice to thrice weekly included unmanageable fluid overload, hyperkalemia, and inadequate clearance (6). Since its inception, the said model of the twice-weekly hemodialysis program has not only penetrated across Southern California dialysis centers, including the Veterans Affairs (VA)–based dialysis centers (2), but has also been utilized regularly in Northern California, where regional investigators have suggested that over half of patients on incident dialysis would be suitable for incremental less-frequent hemodialysis on the basis of plausible simulation modeling (7).
While the growth and expansion of twice-weekly and incremental hemodialysis programs have continued both within the United States and overseas, old questions remain to be answered, and new questions have emerged. Is twice-weekly hemodialysis truly associated with a lower first-year mortality? Will patients be compliant with the expected incremental regimen of transitioning from less-frequent to more-frequent hemodialysis when they started on just twice weekly? While anecdotal data on incremental hemodialysis showed that most patients complied with the prescribed incremental hemodialysis schedule and that very few experienced an end-of-life event before transitioning from twice-weekly to thrice-weekly hemodialysis, there are currently no outcome reports from prospectively collected large clinical data on incremental hemodialysis, and recently started clinical trials have yet to be completed (8), as also suggested by the 2015 KDOQI Guidelines (9). Middle and large molecule clearance with less-frequent hemodialysis requires more studies, as underway by other investigators at VA Palo Alto, California (10).
Although some evidence suggests that incremental dialysis with a twice-weekly schedule may preserve RKF longer than outright thrice-weekly initiation, it is not clear whether other interventions to preserve RKF in patients on hemodialysis can have synergistic effects with this regimen, such as maintaining angiotensin-pathway modulators and high-dose loop diuretics and avoiding intravenous contrast media and excessive ultrafiltration during dialysis. There is an emerging concept of intermittent “AKI” for the RKF, given that fluctuations in RKF have been described in dialysis-dependent patients. If so, urgent research is needed to better understand similarities and distinctions between hemodialysis-associated AKI and the traditional AKI in nondialysis-dependent patients.
Incremental dialysis is consistent with precision medicine given individualized dialysis dose adjustment, lower patient burden and postdialysis fatigue, and possibly better health-related quality of life rendered by less-frequent incremental hemodialysis upon CKD to kidney failure transition. This approach is useful not only in patients treated with peritoneal dialysis, but also in patients receiving home hemodialysis. Gradual transition to more frequent or more intense dialysis therapy within several months or longer can be implemented on an as-needed basis when fluid retention worsens, uremic symptoms develop, or urine volume reaches less than half a liter, especially if loss of nocturia ensues.
The health policy and fiscal implications of a twice-weekly dialysis program are another sensitive topic with many unanswered questions given that, under the traditional model, dialysis providers may lose a third of their bundle payment incentives when patients receive less-frequent hemodialysis. While physician reimbursement is theoretically independent of dialysis frequency, some nephrologists may question lost charges due to less than usual possibilities for physician-patient encounters when patients are present less frequently in the dialysis units. Nevertheless, incremental dialysis was expected to become a preferred treatment in End Stage Renal Disease Seamless Care Organizations (ESCOs). Recent health policy developments, including the US Presidential Executive Order on Advancing American Kidney Health Initiative, are expected to replace the original ESCO plans and be more aligned with incremental dialysis given patient-centeredness and fiscal advantages of the incremental dialysis programs, notwithstanding discussions about the use of twice-weekly dialysis during the coronavirus disease 2019 pandemic.
We recognize that the twice-weekly hemodialysis regimen may represent a provocative paradigm shift for many practicing nephrologists and dialysis providers. It may become the ultimate model for precision medicine and patient centeredness in kidney failure. In addition to classic observational studies on the role of RKF in incremental dialysis (11) and several smaller-scale randomized studies for comparing twice- versus thrice-weekly hemodialysis, which have recently started in the United States and overseas (8), large-scale, pragmatic, randomized controlled trials in patients with incident kidney failure are urgently needed to assess the role of incremental dialysis on RKF preservation, patient survival, patient-reported health-related quality of life, and health care expenses. In-center and home incremental hemodialysis is still in its infancy, and additional studies are warranted.
Disclosures
K. Kalantar-Zadeh has received commercial honoraria and/or support from Abbott, Abbvie, Alexion, Amag Pharma, Amgen, AstraZeneca, Aveo, Baxter, Chugai, DaVita, Dr. Schaer, Fresenius, Genentech, Haymarket Media, Hospira, Kabi, Keryx, National Institutes of Health, Novartis, PCORI, Pfizer, Relypsa, Resverlogix, Sandoz, Sanofi, Shire, UpToDate, Vifor, and ZS-Pharma. M. Murea has received clinical trial funding support from Relypsa, a Vifor Pharma Group Company.
Funding
This work was supported by National Institute of Diabetes and Digestive and Kidney Diseases research grant K24-DK091419 and philanthropic grants from Harold Simmons, Louis Chang, Joseph Lee, and Aveo.
Acknowledgments
We acknowledge the input and responses from patients and health care workers throughout the United States and overseas.
The content of this article reflects the personal experience and views of the author(s) and should not be considered medical advice or recommendations. The content does not reflect the views or opinions of the American Society of Nephrology (ASN) or CJASN. Responsibility for the information and views expressed herein lies entirely with the author(s).
K. Kalantar-Zadeh collected data for the text and the figure, wrote the first draft, reviewed revisions and the final draft, and was responsible for funding for the work. M. Murea expanded the revised drafts and reviewed and amended the final draft.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Kalantar-Zadeh K, Unruh M, Zager PG, Kovesdy CP, Bargman JM, Chen J, Sankarasubbaiyan S, Shah G, Golper T, Sherman RA, Goldfarb DS: Twice-weekly and incremental hemodialysis treatment for initiation of kidney replacement therapy. Am J Kidney Dis 64: 181–186, 2014. 10.1053/j.ajkd.2014.04.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kalantar-Zadeh K, Crowley ST, Beddhu S, Chen JLT, Daugirdas JT, Goldfarb DS, Jin A, Kovesdy CP, Leehey DJ, Moradi H, Navaneethan SD, Norris KC, Obi Y, O’Hare A, Shafi T, Streja E, Unruh ML, Vachharajani TJ, Weisbord S, Rhee CM: Renal replacement therapy and incremental hemodialysis for veterans with advanced chronic kidney disease. Semin Dial 30: 251–261, 2017. 10.1111/sdi.12601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Kidney Foundation : 2006. Updates Clinical Practice Guidelines and Recommendations. Available at: https://www.kidney.org/sites/default/files/docs/12-50-0210_jag_dcp_guidelines-hd_oct06_sectiona_ofc.pdf. Accessed July 11, 2020
- 4.Yan Y, Wang M, Zee J, Schaubel D, Tu C, Qian J, Bieber B, Wang M, Chen N, Li Z, Port FK, Robinson BM, Anand S: Twice-weekly hemodialysis and clinical outcomes in the China dialysis outcomes and practice patterns study. Kidney Int Rep 3: 889–896, 2018. 10.1016/j.ekir.2018.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park JI, Park JT, Kim YL, Kang SW, Yang CW, Kim NH, Oh YK, Lim CS, Kim YS, Lee JP; CRC for ESRD Investigators: Comparison of outcomes between the incremental and thrice-weekly initiation of hemodialysis: A propensity-matched study of a prospective cohort in Korea. Nephrol Dial Transplant 32: 355–363, 2017. 10.1093/ndt/gfw332 [DOI] [PubMed] [Google Scholar]
- 6.Ghahremani-Ghajar M, Rojas-Bautista V, Lau WL, Pahl M, Hernandez M, Jin A, Reddy U, Chou J, Obi Y, Kalantar-Zadeh K, Rhee CM: Incremental hemodialysis: The University of California Irvine experience. Semin Dial 30: 262–269, 2017. 10.1111/sdi.12591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chin AI, Appasamy S, Carey RJ, Madan N: Feasibility of incremental 2-times weekly hemodialysis in incident patients with residual kidney function. Kidney Int Rep 2: 933–942, 2017. 10.1016/j.ekir.2017.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murea M, Moossavi S, Garneata L, Kalantar-Zadeh K: Narrative review of incremental hemodialysis. Kidney Int Rep 5: 135–148, 2019. 10.1016/j.ekir.2019.11.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Kidney Foundation : KDOQI Clinical Practice Guideline for Hemodialysis: 2015. Update. Available at: https://www.kidney.org/professionals/guidelines/hemodialysis2015. Accessed July 11, 2020 [DOI] [PubMed]
- 10.Leong SC, Sao JN, Taussig A, Plummer NS, Meyer TW, Sirich TL: Residual function effectively controls plasma concentrations of secreted solutes in patients on twice weekly hemodialysis. J Am Soc Nephrol 29: 1992–1999, 2018. 10.1681/ASN.2018010081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vilar E, Wellsted D, Chandna SM, Greenwood RN, Farrington K: Residual renal function improves outcome in incremental haemodialysis despite reduced dialysis dose. Nephrol Dial Transplant 24: 2502–2510, 2009. 10.1093/ndt/gfp071 [DOI] [PubMed] [Google Scholar]


