Abstract
Background:
Ulcerative colitis (UC) belongs to chronic colitis whose etiology and pathogenesis still have remained unclear. Hyperbaric oxygen therapy (HBOT) has been demonstrated to be effective for UC therapy. Still, evidence of its efficacy and safety is inconclusive. The purpose of the protocol is to evaluate the efficacy and safety of HBOT in UC therapy.
Methods:
This systematic review will retrieve studies that meet the requirements in Embase, MEDLINE, PubMed, Web of Science, Cochrane Library Central Register of Controlled Trials, the Chinese Biomedical Literature Database (CBM), China national knowledge infrastructure database (CNKI), Wei Pu database, Wan fang database, SinoMed, Google scholar, and Baidu Scholar from their inception to November 2020. Two authors are to be independent in their article selection, data collection, and research quality assessments. The primary outcome is the clinical effectiveness. And the secondary outcomes will include 4 criteria. RevMan 5.3 software will be utilized for analysis of the data.
Results:
The results of this study are to be submitted via a peer-reviewed journal.
Conclusions:
The study is to assess the effectiveness and safety of HBOT for UC and provide valid and reliable evidence regarding HBOT for UC.
INPLASY registration number:
INPLASY2020100118.
Keywords: hyperbaric oxygen therapy, protocol, systematic review, ulcerative colitis
1. Introduction
Ulcerative colitis (UC) is chronic colitis affecting the bowel whose pathogenic mechanism is multifactored. The pathogenic mechanism of UC involves genetic, immune, and environmental factors.[1] Symptoms of UC usually present with bloody mucopurulent stool, diarrhea, and bellyache, and they seriously impair the level of health for patients.[2] In addition, diagnosis of UC mainly relies on endoscopy and clinical symptoms.[3] It has been reported that the occurrence rate of UC is increasing globally.[4] Furthermore, the incidence of UC is increasing worldwide over the past few years, affecting mostly young individuals.[5,6] And UC is becoming one of the clinically refractory diseases.
Nowadays, drug treatment and surgery have become the major treatment modalities for UC.[7] More specifically, the effective drug treatments for UC are 5-aminosalicylate compounds, corticosteroids, and immunosuppressive agents. However, failure of standard drug treatments for UC often leads to colon removed.[8] In a word, poor efficacy and side effects of drug treatment and surgery would hinder the health for some UC patients. Thus, there is an urgent need to explore novel treatment options against UC.
Hyperbaric oxygen therapy (HBOT) is a promising medical technology in which people breath 100% oxygen under elevated atmospheric pressure.[9] HBOT not only improves plasma and tissue oxygen content but also improves the oxygen levels of blood reaching inflamed bowel.[10] Indeed, several clinical trials have suggested that HBOT is effective for UC therapy,[11–13] and the mechanism of action of HBOT for UC could be associated with reduction of pro-inflammatory cytokines and chemokines which are responsible for the metabolic stress created during active inflammation.[10] However, there are no previously published systematic review and meta-analyses on assessing the effectiveness and safety of HBOT for UC, and evidence of its efficacy and safety is inconclusive. Therefore, the article intends to adopt the systematic evaluation and meta-analysis to assess the clinical effectiveness and safety of HBOT for UC, so as to offer the scientific evidence of HBOT for UC.
2. Methods
2.1. Study registration
We registered the protocol with the International Platform of Registered Systematic Review and Meta-Analysis Protocols (INPLASY) on 31 October 2020. Its accession number is INPLASY2020100118 (DOI is 10.37766/inplasy2020.10.0118, https://inplasy.com/inplasy-2020-10-0118/).
2.2. Inclusion criteria
2.2.1. Selection of researches
Randomized controlled trials (RCTs) that investigated the effectiveness and safety of HBOT for UC will be selected for inclusion. Non-randomized controlled trials, literature reviews, case reports, studies with animal experiments, specialist experience, and repeated documents will not be collected.
2.2.2. Selection of participants
Participants who are clinically met the diagnostic criteria of UC are to be enrolled, in despite of sex, age, ethnicity, the extent of illness, economic status, or educational level. Meanwhile, some special UC participants who were pregnant or breastfeeding mothers or with cardiac, hepatic or lung diseases will be excluded.
2.2.3. Selection of intervention
On the one hand, the intervention measures of the treatment group were individual HBOT or in collaboration with conventional therapy according to modern guidelines. On the other hand, the intervention measures of the control group included no HBOT therapy, placebo and conventional treatment according to modern guidelines.
2.2.4. Settings of outcome measures
We will mainly observe the overall effectiveness to obtain the primary outcomes. And the secondary outcomes will contain 4 items: clinical response, endoscopic remission, inflammatory markers levels, and adverse events.
2.3. Search strategy
We are to systematically search medical subject headings and keywords associated with HBOT in the treatment of UC based on the following databases until November 2020: Embase, MEDLINE, PubMed, Web of Science, Cochrane Library Central Register of Controlled Trials, the Chinese Biomedical Literature Database (CBM), China national knowledge infrastructure database (CNKI), Wei Pu database, Wan fang database, and SinoMed. Meanwhile, we will also search the relevant literatures in Google scholar, Baidu Scholar. Table 1 shows the search strategy of PubMed. Likewise, similar strategies slightly modified were used for the other databases.
Table 1.
Search strategy in PubMed.
| Number | Entry terms |
| #1 | “Colitis, Ulcerative” [MeSH Terms] or “Colitis, Ulcerative” [Title/Abstract] or “Idiopathic Proctocolitis” [Title/Abstract] or “Ulcerative Colitis” [Title/Abstract] or “Colitis Gravis” [Title/Abstract] or “ Inflammatory Bowel Disease, Ulcerative Colitis Type” [Title/Abstract] |
| #2 | “Hyperbaric Oxygenation” [MeSH Terms] or “Hyperbaric Oxygenation” [Title/Abstract] or “Hyperbaric Oxygenations” [Title/Abstract] or “Oxygenations, Hyperbaric” [Title/Abstract] or “Hyperbaric Oxygen Therapy” [Title/Abstract] or “Hyperbaric Oxygen Therapies” [Title/Abstract] or “Oxygen Therapies, Hyperbaric” [Title/Abstract] or “Oxygen Therapy, Hyperbaric” [Title/Abstract] or “Therapies, Hyperbaric Oxygen” [Title/Abstract] or “Therapy, Hyperbaric Oxygen” [Title/Abstract] or “Oxygenation, Hyperbaric” [Title/Abstract] |
| #3 | “Randomized controlled trial” [Publication Type] or “Randomized controlled trial” [Title/Abstract] |
| #4 | #1 and #2 and #3 |
2.4. Data obtainment and analysis
2.4.1. Collection of articles
Firstly, according to the search strategies, the preliminary articles are to be searched and imported to EndnoteX9 tool. And then, the EndnoteX9 tool will be used to remove the duplicates. After this, 2 authors will review the titles and abstracts of the studies independently to narrow down the articles. Next, the eligible articles will be read for full-text assessment to be further screened by 2 authors. In case of disagreements, we will consult the third author and resolve them by discussions. This selection process is demonstrated by a flow chart as shown in Fig. 1.
Figure 1.
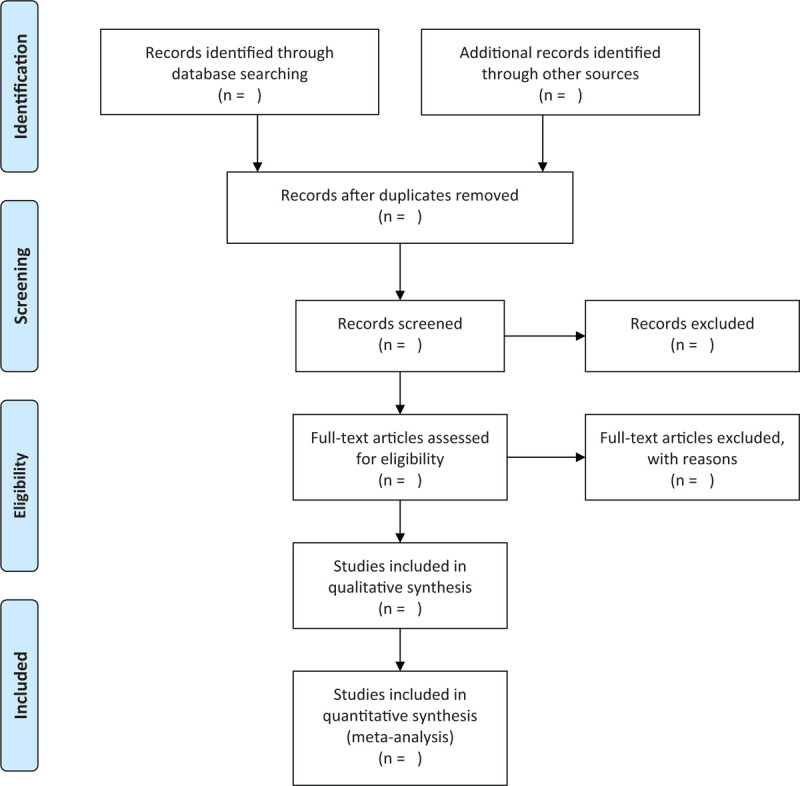
Flow diagram of the study selection process.
2.4.2. Data refinement
Two authors are to independently refine the data from the articles which met the eligibility, containing routine information of articles, study approaches, all participant information, the content of control and the intervention, outcome indexes, and adverse effects. Should data be missing, inaccurate or ambiguous, we will resolve it via contacting the corresponding author in obtained articles, or consulting the third party or conducting internal discussions.
2.4.3. Evaluation of risk of bias
Two authors will independently assess the risk of bias on the basis of the Cochrane risk-of-bias tool for each study included. And they will determine the bias based on these aspects: random sequence generation, concealed allocation, implementation of blind method of the participants and subjects, implementation of blind method of the research results, data integrity, reporting with selectivity, and other aspects. In the end, each study will be evaluated into 3 conditions, “Low risk,” “High risk,” and “Unclear risk.”[14] In addition, we will resolve any inconsistencies through contacting the corresponding author in obtained literature, consulting the third party, or conducting internal discussions.
2.4.4. Determination of treatment efficacy
For continuous data, we are to apply the mean difference with 95% confidence intervals to determine the treatment efficacy. For dichotomous data, we are to apply relative risk with 95% confidence intervals for analysis.
2.4.5. Handling missing data
Where data are missing, we need attempt to communicate with the first author or correspondent author by e-mail or phone to acquire the complete data. If the contact fails, we will start our analysis according to the existing data.[15] Additionally, the probable effect of incomplete data will also be included in the discussion.
2.4.6. Determination of heterogeneity
Heterogeneity will be determined with the I2 statistic and chi-squared test. There is substantial heterogeneity among the trials when I2 ≥ 50%, but low or no heterogeneity while I2 < 50%. Moreover, we will conduct subgroup analysis or sensitivity analysis to check the possible reasons when heterogeneity is substantial.
2.4.7. Analysis of reporting bias
We will apply funnel plots and Egger test to detect reporting bias if at least 10 RCTs are available to us.[16]
2.4.8. Data synthesis
Related analyses will be performed in RevMan 5.3 software (The Cochrane Collaboration, Oxford, England). If heterogeneity is minor (I2 < 50%), we will apply the fixed-effect approach for meta-analysis. However, if heterogeneity is substantial (I2 ≥ 50%), we will apply the random-effect approach for meta-analysis. On the other hand, we will carry out the narrative analysis if there is significant heterogeneity or inability to judge the source of it.
2.4.9. Subgroup analysis
If necessary, we need carry out subgroup analysis to deal with heterogeneity due to interventions, participant information, and outcome indexes.
2.4.10. Sensitivity analysis
We are to conduct sensitivity analysis to assess the stability of the conclusions by eliminating the inferior methodological quality studies.
2.4.11. Determination of evidence quality
We will use the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) working group approach to determine the evidence quality for all outcomes. The quality of evidence quality will be classified into as high, moderate, low, or very low.
2.5. Ethics and dissemination
The study does not need ethics approval for the reason that primary personal data will not be collected. In addition, the results of this study are to be submitted via a peer-reviewed journal.
3. Discussion
UC is a refractory and immune-related intestinal lesion with repeated attack and unknown etiology, which substantially diminishes the quality of life of patients.[17] HBOT is a commonly primary or adjunctive medical treatment[18] and more and more clinical studies suggest it is potentially beneficial to therapy for UC.[11–13,19,20] Nevertheless, there are no systemic reviews published regarding the effectiveness and safety of HBOT for UC. Consequently, we will perform the study to determine the effectiveness and safety of HBOT for UC. Similarly, it is our hope that this study will supply further evidence to guide clinical practice for UC. Additionally, it is important to notice that this study still has several potential limitations. First, the quality of different study could lead to the substantial heterogeneity. Second, the different modalities of HBOT and the different conditions of patients with UC may also cause clinical heterogeneity.
Author contributions
Data curation: Wei Wang, Ying He, Shangshang Jiang.
Formal analysis: Wei Wang, Ying He, Shangshang Jiang.
Methodology: Wei Wang, Ying He, Dou Wen.
Project administration: Shangshang Jiang, Xiaodong Zhao.
Resources: Dou Wen, Xiaodong Zhao.
Software: Wei Wang, Ying He, Dou Wen.
Visualization: Wei Wang, Ying He, Xiaodong Zhao.
Writing – original draft: Wei Wang, Ying He.
Writing – review & editing: Shangshang Jiang, Xiaodong Zhao.
Footnotes
Abbreviations: HBOT = hyperbaric oxygen therapy, INPLASY = International Platform of Registered Systematic Review and Meta-Analysis Protocols, RCTs = randomized controlled trials, UC = ulcerative colitis.
How to cite this article: Wang W, He Y, Wen D, Jiang S, Zhao X. Efficacy and safety evaluation of hyperbaric oxygen therapy for patients with ulcerative colitis: A protocol of systematic review and meta-analysis. Medicine. 2021;100:1(e00000).
WW, YH and XZ have contributed equally to this work and are co-first authors.
This project was funded by the National Natural Science Foundation of China (No.82074187).
The sponsor was not involved in design, execution, or writing the study.
If amendments are needed, we will update the protocol to include any changes in the entire research process.
The datasets generated during and/or analyzed during the current study are publicly available.
The authors have no conflicts of interest to disclose.
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
- [1].Wu H, Rao Q, Ma GC, et al. Effect of triptolide on dextran sodium sulfate-induced ulcerative colitis and gut microbiota in mice [published correction appears in Front Pharmacol. 2020 Mar 10;11:319]. Front Pharmacol 2020;10:1652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Shi L, Han X, Li JX, et al. Identification of differentially expressed genes in ulcerative colitis and verification in a colitis mouse model by bioinformatics analyses. World J Gastroenterol 2020;26:5983–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Hata K, Ishihara S, Ajioka Y, et al. Long-term follow-up of targeted biopsy yield (LOFTY Study) in ulcerative colitis surveillance colonoscopy. J Clin Med 2020;9:2286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Wu H, Rao Q, Ma GC, et al. Effect of triptolide on dextran sodium sulfate-induced ulcerative colitis and gut microbiota in mice [published correction appears in Front Pharmacol. 2020 Mar 10;11: 319]. Front Pharmacol 2020;10:1652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Ng SC, Shi HY, Hamidi N, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies.[published correction appears in Lancet 2020; 396: e56]. Lancet 2018;390:2769–78. [DOI] [PubMed] [Google Scholar]
- [6].Tian C, Huang Y, Wu X, et al. The efficacy and safety of mesalamine and probiotics in mild-to-moderate ulcerative colitis: a systematic review and meta-analysis. Evid Based Complement Alternat Med 2020;2020:6923609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Shi G, Wang G, Lu S, et al. PD-L1 is required for human endometrial regenerative cells-associated attenuation of experimental colitis in mice. Am J Transl Res 2019;11:4696–712. [PMC free article] [PubMed] [Google Scholar]
- [8].Rather IA, Bajpai VK, Ching LL, et al. Effect of a bioactive product SEL001 from Lactobacillus sakei probio65 on gut microbiota and its anti-colitis effects in a TNBS-induced colitis mouse model. Saudi J Biol Sci 2020;27:261–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Tanaka T, Minami A, Uchida J, et al. Potential of hyperbaric oxygen in urological diseases. Int J Urol 2019;26:860–7. [DOI] [PubMed] [Google Scholar]
- [10].Dulai PS, Gleeson MW, Taylor D, et al. Systematic review: the safety and efficacy of hyperbaric oxygen therapy for inflammatory bowel disease. Aliment Pharmacol Ther 2014;39:1266–75. [DOI] [PubMed] [Google Scholar]
- [11].Dulai PS, Raffals LE, Hudesman D, et al. A phase 2B randomised trial of hyperbaric oxygen therapy for ulcerative colitis patients hospitalised for moderate to severe flares [published online ahead of print, 2020 Aug 3]. Aliment Pharmacol Ther 2020;52:955–63. [DOI] [PubMed] [Google Scholar]
- [12].Jairath V. Hyperbaric oxygen for hospitalized patients with ulcerative colitis. Am J Gastroenterol 2018;113:1432–4. [DOI] [PubMed] [Google Scholar]
- [13].Dulai PS, Buckey JC, Jr, Raffals LE, et al. Hyperbaric oxygen therapy is well tolerated and effective for ulcerative colitis patients hospitalized for moderate-severe flares: a phase 2A pilot multi-center, randomized, double-blind, sham-controlled trial. Am J Gastroenterol 2018;113:1516–23. [DOI] [PubMed] [Google Scholar]
- [14].Yan X, Ma F, Yu Y, et al. Effects of herb-partitioned moxibustion for ulcerative colitis: a protocol for systematic review and meta-analysis. Medicine (Baltimore) 2020;99:e21319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Yang L, Song Y, Jin P, et al. Shen-Ling-Bai-Zhu-San for ulcerative colitis: protocol for a systematic review and meta-analysis. Medicine (Baltimore) 2018;97:e12337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Satani N, Cai C, Giridhar K, et al. World-wide efficacy of bone marrow derived mesenchymal stromal cells in preclinical ischemic stroke models: systematic review and meta-analysis. Front Neurol 2019;10:405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Gu S, Xue Y, Gao Y, et al. Mechanisms of indigo naturalis on treating ulcerative colitis explored by GEO gene chips combined with network pharmacology and molecular docking. Sci Rep 2020;10:15204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Kovacevic S, Ivanov M, Miloradovic Z, et al. Hyperbaric oxygen preconditioning and the role of NADPH oxidase inhibition in postischemic acute kidney injury induced in spontaneously hypertensive rats. PLoS One 2020;15:e0226974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Fahad H, Dulai PS, Shen B, et al. Hyperbaric oxygen therapy is effective in the treatment of inflammatory and Fistulizing pouch complications [published online ahead of print, 2020 Jun 19]. Clin Gastroenterol Hepatol 2020;S1542–S3565:30840–5. [DOI] [PubMed] [Google Scholar]
- [20].Seo HI, Lee HJ, Han KH. Hyperbaric oxygen therapy for pyoderma gangrenosum associated with ulcerative colitis. Intest Res 2018;16:155–7. [DOI] [PMC free article] [PubMed] [Google Scholar]


