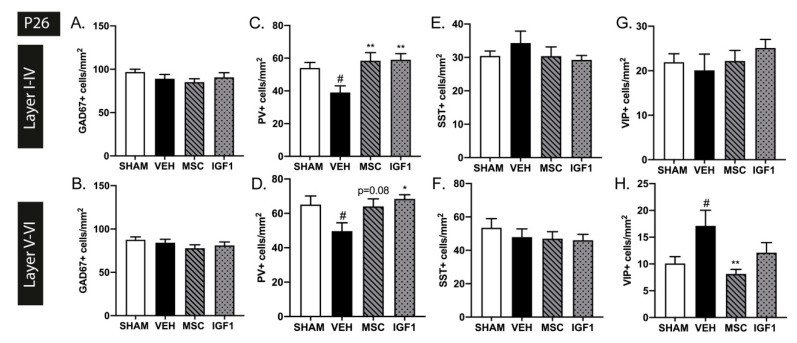
Figure 3.
Intranasal mesenchymal stem cells (MSC) or insulin-like growth factor (IGF1) therapy reduces subtype-specific cortical interneuron deficits caused by postnatal hypoxia/ischemia and systemic inflammation in neonatal mice. (A,B) Injury induction did not lead to changes in GAD67+ cell density in the upper (A) or lower (B) cortical layers in our validated EoP mouse model at P26 (SHAM n = 12, VEH n = 13, MSC n = 10, IGF1 n = 11). (C,D) A reduction in PV+ interneuron density was observed in vehicle-treated hypoxia-ischemia and lipopolysaccharide (HI+LPS) animals (n = 13) compared to sham-controls (n = 11) in both the upper (C) and lower (D) layers of the cortex at P26. Intranasal MSC (n = 10) or IGF1 (n = 10) treatment restored cortical PV+ cell density up to sham-control levels (a trend for MSC treatment-induced recovery of PV+ cells in the lower cortical layers). (E,F) The number of SST+ interneurons was not affected in the upper (E) nor lower (F) cortex after HI+LPS (SHAM n = 11, VEH n = 10, MSC n = 10, IGF1 n = 10). (G,H) Vehicle-treated EoP mice (n = 12) displayed an increase in VIP+ cells per mm2 in the lower (H) but not the upper (G) cortical regions compared to sham-controls (n = 12). Treatment with intranasal MSCs (n = 8) significantly reduced VIP+ cell density. Intranasal IGF1 administration (n = 9) did not significantly affect the amount of VIP+ interneurons after EoP. #: p < 0.05; vehicle-treated HI+LPS animals vs. sham-controls; *: p < 0.05; **: p < 0.01; MSC- or IGF1-treated HI+LPS animals vs. vehicle-treated HI+LPS animals. Nearly significant p values are indicated in d.