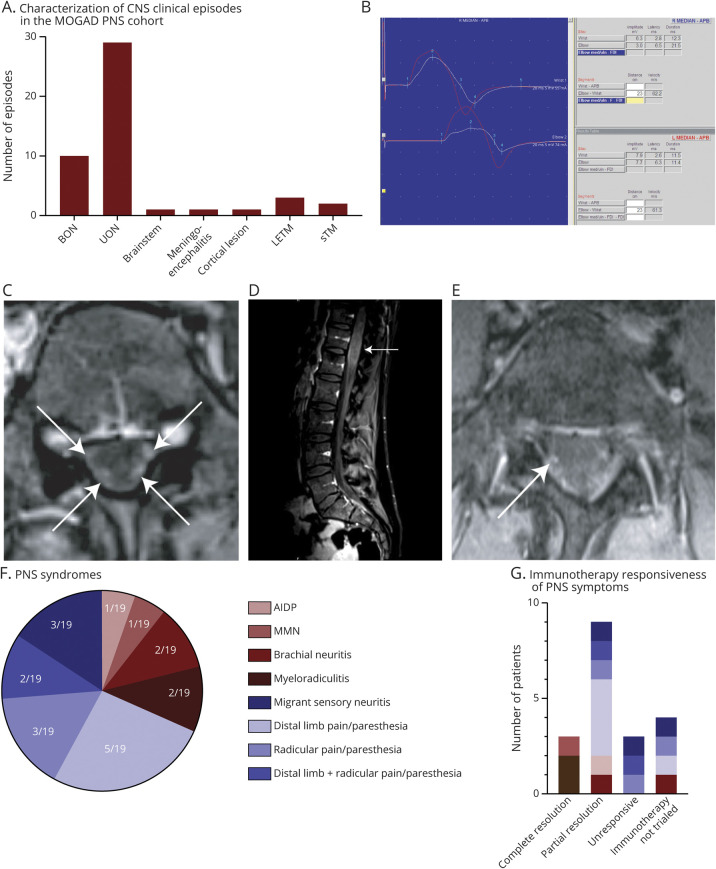
Figure 1. The clinical, neurophysiological, and radiological characterization of PNS involvement in MOGAD.
(A) Clinical phenotyping of the number of CNS episodes in patients in this cohort. ON, inclusive of both BON and UON presentations, was the most frequent clinical phenotype, making up 39/47 (83%) episodes. (B) The right median nerve motor response (white) is smaller than the left (red) with a further reduction of amplitude at the elbow and with reduced persistence of median nerve F wave responses. These findings are consistent with right median neuropathy with conduction block at the elbow in a patient diagnosed with MMN. (C) Axial T1-weighted MRI with gadolinium showing enhancement of dorsal and ventral nerve roots (white arrows). (D) Sagittal T1-weighted MRI with gadolinium showing expansion of the conus (white arrow). (E) Axial fat-suppressed T1 with gadolinium showing enhancement of intradural right S1 nerve root (white arrow). (F) Proportion of the PNS syndromes identified in this cohort of patients with MOGAD. (G) A summary of the immunotherapy responsiveness of particular PNS syndromes—complete resolution occurred in 3/15 patients in whom immunotherapy was trialed (2 with myeloradiculitis and 1 with multifocal motor neuropathy), with 9/15 having only partial resolution and 3/15 being unresponsive to immunotherapy. AIDP = acute inflammatory demyelinating polyneuropathy; BON = bilateral optic neuritis; CIDP = chronic inflammatory demyelinating polyneuropathy; LETM = longitudinally extensive transverse myelitis; MMN = multifocal motor neuropathy; MOG = myelin oligodendrocyte glycoprotein; ON = optic neuritis; PNS = peripheral nervous system; sTM = short transverse myelitis; UON = unilateral optic neuritis.