Abstract
Purpose
Magnetic resonance imaging (MRI) contrast agents have been used off-label for diagnosis of cerebrospinal fluid (CSF) leaks and lately also for assessment of the glymphatic system and meningeal lymphatic drainage. The purpose of this study was to further evaluate the short- and long-term safety profile of intrathecal MRI contrast agents.
Methods
In this prospective study, we compared the safety profile of different administration protocols of intrathecal gadobutrol (GadovistTM; 1.0 mmol/ml). Gadobutrol was administered intrathecal in a dose of 0.5 mmol, with or without iodixanol (VisipaqueTM 270 mg I/ml; 3 ml). In addition, a subgroup was given intrathecal gadobutrol in a dose of 0.25 mmol. Adverse events were assessed at 1 to 3 days, 4 weeks, and after 12 months.
Results
Among the 149 patients, no serious adverse events were seen in patients without history of prior adverse events. The combination of gadobutrol with iodixanol did not increase the occurrence of non-serious adverse events after days 1–3. Intrathecal gadobutrol in a dose of 0.25 mmol caused less severity of nausea, as compared with the dose of 0.5 mmol. The clinical diagnosis was the major determinant for occurrence of non-serious adverse events after intrathecal gadobutrol.
Conclusion
This prospective study showed that intrathecal administration of gadobutrol in a dose of 0.5 mmol is safe. Non-serious adverse events were to a lesser degree affected by the administration protocols, though preliminary data are given that side effects of intrathecal gadobutrol are dose-dependent.
Keywords: Glymphatic function, Magnetic resonance imaging, Contrast agents, Gadobutrol, Iodixanol, Safety
Introduction
Since the glia-lymphatic (or glymphatic) system was described in 2012 [1], it has attracted a lot of interest and scientific discussion by providing a new perspective on brain-wide clearance of toxic brain metabolites such as amyloid-β and tau protein and thereby playing a pivotal role in neurodegenerative disease [2]. Later, intrathecal contrast-enhanced magnetic resonance imaging (MRI) gave in vivo evidence for the existence of a brain-wide glymphatic system in humans [3, 4] and also demonstrated molecular efflux pathways from cerebrospinal fluid (CSF) to neck lymph nodes [5], the parasagittal dura [6], and choroid plexus [7].
Several concerns exist about the off-label intrathecal use of MRI contrast agents, primarily due to potential neurotoxic effects [8–10], and report on retention of linear gadolinium chelates within the human brain extra-vascular space after repeated intravenous administrations [11–13]. A potential mechanism for the findings of gadolinium outside the blood-brain barrier was given by recent observations of MRI contrast agents leaking from blood to CSF [14, 15], even in individuals without blood-brain barrier dysfunction [15, 16], mainly through the choroid plexus [17], but also via the ciliary body [16, 18]. In principle, an intravenous dosage of contrast agent to venous blood therefore also represents a small dosage of contrast agent to CSF; one MRI study indicated that CSF concentration of contrast agent is one-fifth of the intravenous concentration after intravenous administration [16].
We recently reported the safety profile of intrathecal gadobutrol in 100 subjects [19]. The purpose of the present study was to expand the analysis to include additional 49 patients in order to compare different administration protocols of intrathecal gadobutrol, i.e., 0.5 mmol gadobutrol (0.5 ml of GadovistTM, 1.0 mmol/ml), with or without 3 ml iodixanol (VisipaqueTM, 270 mg I/ml). In addition, we performed MRI using 0.25 mmol gadobutrol. Adverse events, categorized as serious or non-serious, were assessed days 1–3 and after 4 weeks and 12 months.
Materials and methods
Patient material and study design
The study design was prospective and carried out during the period from September 2015 to December 2019. We included consecutively patients admitted to the Department of neurosurgery, Oslo University Hospital - Rikshospitalet, for work-up of various CSF circulation disorders (Table 1). Exclusion criteria were as follows: a history of hypersensitivity reactions to imaging contrast agents or a history of severe allergy reactions in general or evidence of renal dysfunction. Pregnant or breastfeeding women and individuals < 18 or > 80 years were not included.
Table 1.
Patient material and different protocols
| Patient material | Protocol | Statistics | ||||
|---|---|---|---|---|---|---|
| Total | #1 | #2 | #3 | Protocol #1 vs. #2 | Protocol #2 vs. #3 | |
| N | 149 | 115 | 29 | 5 | ||
| Age (years) | 48.6 ± 17.9 | 49.0 ± 18.7 | 46.9 ± 15.4 | 48.8 ± 15.2 | ns | ns |
| Gender (female/male) | 92 (62%)/57 (38%) | 69 (60%)/46 (40%) | 20 (69%)/9 (31%) | 3 (60%)/2 (40%) | ns | ns |
| BMI (kg/m2) | 27.5 ± 5.1 | 27.3 ± 5.1 | 28.1 ± 4.6 | 29.4 ± 7.9 | ns | ns |
| Tentative diagnosis | ||||||
| Idiopathic normal pressure hydrocephalus | 38 (26%) | 36 (31%) | 1 (3%) | 1 (20%) | P = 0.002 | ns |
| Spontaneous intracranial hypotension | 22 (15%) | 15 (13%) | 6 (21%) | 1 (20%) | ns | ns |
| Arachnoid cyst | 27 (18%) | 19 (17%) | 7 (24%) | 1 (20%) | ns | ns |
| Pineal cyst | 26 (17%) | 23 (20%) | 2 (7%) | 1 (20%) | ns | ns |
| Idiopathic intracranial hypertension | 22 (15%) | 11 (10%) | 10 (35%) | 1 (20%) | P = 0.001 | ns |
| Communicating hydrocephalus | 11 (7%) | 8 (7%) | 3 (10%) | 0 | ns | ns |
| Non-communicating hydrocephalus | 3 (2%) | 3 (3%) | 0 | 0 | ns | - |
Data given as numbers (percentage in parenthesis) and mean ± standard deviation. Significance determined by the Pearson chi-square test. ns non-significant
This research study was approved by the Institutional Review Board (2015/1868), Regional Ethics Committee (2015/96) and the National Medicines Agency (15/04932-7). Participants were included following written and oral informed consent.
Protocols for intrathecal gadobutrol
Intrathecal contrast administration was performed by interventional neuroradiologists using x-ray guided lumbar puncture. Access to the spinal canal was typically obtained at level L2/L3 or L3/L4 and in some cases at level L4/5. Correct placement of a spinal syringe tip was secured by CSF backflow from the puncture needle (22G × 3½″) and the free distribution of radiopaque contrast agent in CSF when this was used. In this study, three different protocols were used:
Protocol #1
Intrathecal injection of 0.5 mmol (0.5 ml of 1.0 mmol/ml gadobutrol; GadovistTM, Bayer Pharma AG, Berlin, Germany) in combination with 2–3 ml of 270 mg I/ml iodixanol (VisipaqueTM, GE Healthcare, USA).
Protocol #2
Intrathecal injection of 0.5 mmol (0.5 ml of 1.0 mmol/ml gadobutrol; GadovistTM, Bayer Pharma AG, Berlin, Germany) alone.
Protocol #3
Intrathecal injection of 0.25 mmol (0.25 ml of 1.0 mmol/ml gadobutrol; GadovistTM, Bayer Pharma AG, Berlin, Germany) alone.
MRI acquisitions
As previously described [20], the MRI protocol included acquisition of sagittal 3D T1-weighted spoiled gradient echo volume scans using a
3 T Philips IngeniaTM MRI scanner (Philips Medical systems, Best, The Netherlands), with equal imaging sequence parameters at all time points. The following main imaging parameters were used: repetition time = “shortest” (typically 5.1 ms), echo time = “shortest” (typically 2.3 ms), flip angle = 8 degrees, field of view = 256 × 256 cm, and matrix = 256 × 256 pixels (reconstructed 512 × 512); 184 over-contiguous slices with 1 mm thickness automatically reconstructed to 368 slices and a thickness of 0.5 mm were sampled. Each image acquisition lasted about 6.5 min.
Consecutive and identical MRI acquisitions covering the cranial compartment and upper neck region were repeated at regular intervals, to verify and assess time of gadobutrol entry to cranial CSF spaces. The patients were transferred between the MRI suite and the ward department and between the bed and the MRI table by the hospital staff to keep the patient in the supine position. The participants were instructed to remain supine in bed the first hours after intrathecal gadobutrol but could move freely from afternoon. The MRI protocol included MRI acquisitions after 0–20 min, 20–40 min, 40–60 min, 1–2 h, 4–6 h, 6–9 h, 24 h, and 48 h.
The first appearance of MRI contrast agent in the subarachnoid space at level of the foramen magnum was visually assessed by an experienced neuroradiologist (G.R.) on the sagittal T1-weighted volume scans in the hospital PACS (Sectra IDS7®, Sectra, Sweden).
For quantitative assessment how different doses (0.5 versus 0.25 mmol) of intrathecal gadobutrol changed the intensity of the T1 signal, a region of interest was placed within the cisterna magna, with assessment of mean T1 signal intensity (in signal units) from the image gray scale. The signal unit was normalized against a reference region of interest by dividing measured T1 intensity from CSF with the value of the reference region of interest to correct for any baseline changes of image gray scale due to image scaling. The reference region of interest was placed within the posterior part of the superior sagittal sinus in axially reconstructed images from the same T1 volume scan.
Assessment of serious and non-serious adverse events
The adverse events were categorized as serious or non-serious:
Serious adverse events were any untoward medical occurrence resulting in death, being immediately life-threatening, requiring in-patient hospitalization or prolongation of existing hospitalization, resulting in persistent or significant disability or incapacity, or being an important medical event that may jeopardize the subject or may require medical intervention to prevent one of the mentioned outcomes.
Non-serious adverse events were defined as any untoward medical occurrence in study participants, including any unfavorable and unintended sign, symptom, or temporary disease, whether or not related to the intrathecal gadobutrol administration. Participants were specifically asked for presence of defined symptoms chosen according to side effects most commonly observed after intrathecal iohexanol: headache (mild/moderate/severe), nausea (mild/moderate/severe), dizziness (mild/moderate/severe), itch, warmth feeling, paresthesia, visual symptoms, cognitive difficulties, muscular spasms, discomfort at injection site, and tremor. In addition, other complaints than those specifically questioned for were listed, independent of possible cause.
The adverse events were recorded systematically by study nurses not otherwise involved in management of patients at 1–3 days after intrathecal contrast agent administration and at 4 weeks. Patients who still reported symptoms at 4 weeks were phoned by the study nurses at a later occasion ranging from a few months to up to 12 months for a final assessment. Report of symptoms at any other contact after 4 weeks was registered and categorized as “Late.”
Statistics
The statistical analyses were performed using the SPSS software version 25 (IBM Corporation, Armonk, NY). Significant differences between categorical data were determined using the Pearson chi-square test. Differences between groups were determined using one-way ANOVA. Significance was accepted at the 0.05 level.
Results
Patients
Table 1 presents demographic information and clinical indication for intrathecal gadobutrol in the 149 patients included in this study. The type of clinical indication differed between the different protocols.
Verified intracranial distribution of gadobutrol
Entry of gadobutrol to cranial CSF spaces was verified in all individuals at MRI (Fig. 1). The time from intrathecal gadobutrol administration until first visual detection of the contrast agent in subarachnoid space at the level of foramen magnum was 22 ± 34 min (spinal transit time; Fig. 2), with no significant differences across the patient groups (Fig. 3).
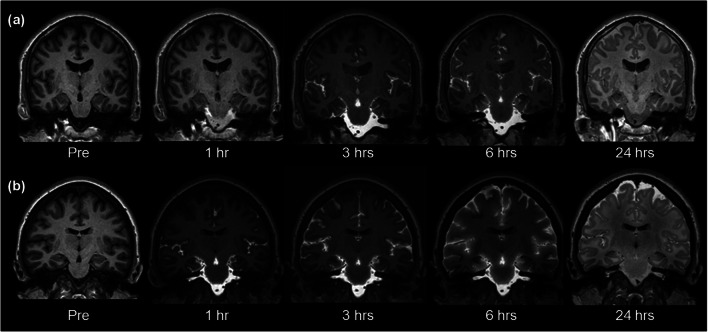
Fig. 1.
Intrathecal injection of gadobutrol in a dose of (a) 0.25 mmol (0.25 ml of 1.0 mmol/ml) or (b) 0.5 mmol (0.50 ml of 1.0 mmol/ml) at the lower lumbar level. Entry of gadobutrol in CSF within the intracranial compartment was preceded by unenhanced T1-weighted MRI (time point “Pre”), and acquisition of identical consecutive T1 scans was initiated immediately and repeated at different time points. Image window/level is adjusted to optimize qualitative illustration of CSF contrast enhancement
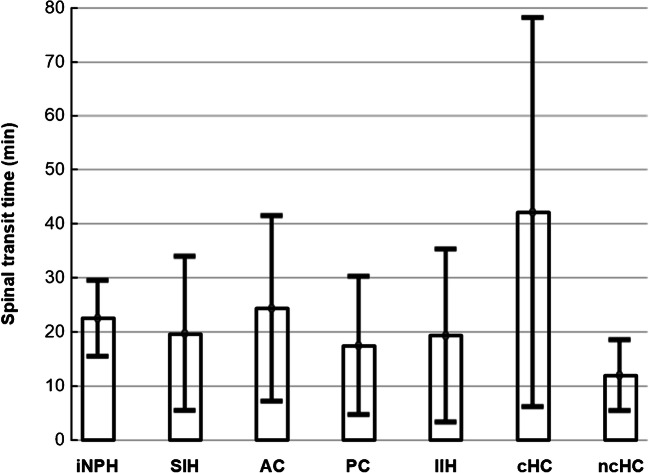
Fig. 2.
There was no significant difference between patient groups regarding time from intrathecal administration of gadobutrol until first enhancement of the contrast agent within the subarachnoid space of the foramen magnum (spinal transit time). For the entire group of 149 individuals, the mean ± stdev spinal transit time was 22 ± 34 min. The tentative diagnoses were as follows: iNPH, idiopathic normal pressure hydrocephalus; SIH, spontaneous intracranial hypotension; AC, arachnoid cyst; PC, pineal cyst; IIH, idiopathic intracranial hypertension; cHC, communicating hydrocephalus; and ncHC, non-communicating hydrocephalus
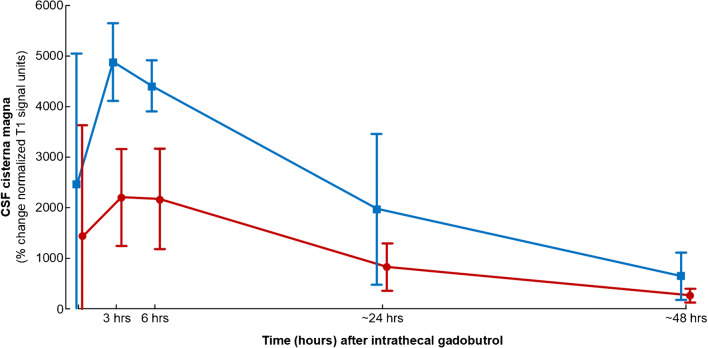
Fig. 3.
CSF tracer enrichment in cisterna magna depending on dose of CSF tracer (gadobutrol), measured as percentage change in normalized T1 signals after intrathecal injection of gadobutrol in doses of 0.5 mmol (protocols #1–2; blue line) or 0.25 mmol (protocol #3; red line). The first time point is after 10 min. The CSF tracer level was significantly different after 3 h (P < 0.001), 6 h (P = 0.001), and 48 h (P = 0.047; independent samples t test).
The CSF enrichment within cisterna magna was dose-dependent with larger T1 intensity increase in CSF after 3, 6, and 48 h in individuals receiving intrathecal gadobutrol in a dose of 0.5 mmol as compared with 0.25 mmol (Fig. 3).
Serious adverse events
Serious adverse events likely related to intrathecal gadobutrol administration were not seen in patients without a history of prior adverse events. By error, one woman with known allergy to iodinated contrast agents was included in the study and given the combination of intrathecal gadobutrol and iodixanol, despite interaction with referring doctor, study nurse, the neurologist who managed hospital admittance, and an anesthesiologist. She had an immediate anaphylactic reaction consisting of skin rash, dyspnea, and fall in blood pressure similar to the previous reaction to iodinated contrast agent. After intravenous Ringer acetate (1000 ml) and surveillance within the intensive care unit for a few hours, no further actions were needed, and she was able to undergo MRI scanning after a few hours.
An 80-year-old man with idiopathic normal pressure hydrocephalus (iNPH) was diagnosed with a pulmonary embolism, which was attributed to a long train journey and reduced mobility immediately before hospitalization.
Non-serious adverse events depending on administration protocol
Table 2 lists the non-serious adverse events during days 1–3. Typically, these adverse events occurred during day 1 and rarely on days 2 or 3.
Table 2.
Non-serious adverse events depending on protocol days 1–3
| Patients | Protocol | Statistics | ||||||
|---|---|---|---|---|---|---|---|---|
| Total (n = 149) | #1 (n = 115) | #2 (n = 29) | #3 (n = 5) | Protocol #1 vs. #2 | Protocol #1 vs. #3 | Protocol #2 vs. #3 | ||
| No adverse events (N/%) | 36 (24%) | 26 (23%) | 9 (31%) | 1 (20%) | ns | ns | ns | |
| Headache (N/%) | 69 (46%) | 52 (45%) | 14 (48%) | 3 (60%) | ns | ns | ns | |
| Severity | Mild (N/%) | 8 (5%) | 4 (4%) | 4 (14%) | 0 | |||
| Moderate (N/%) | 17 (11%) | 14 (12%) | 2 (7%) | 1 (20%) | ns | ns | ns | |
| Severe (N/%) | 44 (30%) | 34 (30%) | 8 (28%) | 2 (40%) | ||||
| Nausea (N/%) | 84 (56%) | 67 (58%) | 13 (45%) | 4 (80%) | ns | ns | ns | |
| Severity | Mild (N/%) | 25 (17%) | 21 (18%) | 1 (3%) | 3 (60%) | |||
| Moderate (N/%) | 11 (7%) | 7 (6%) | 4 (14%) | 0 | ns | ns | P = 0.004 | |
| Severe (N/%) | 48 (32%) | 39 (34%) | 8 (28%) | 1 (20%) | ||||
| Dizziness (N/%) | 60 (40%) | 44 (38%) | 13 (45%) | 3 (60%) | ns | ns | ns | |
| Severity | Mild (N/%) | 20 (13%) | 13 (11%) | 5 (17%) | 2 (40%) | |||
| Moderate (N/%) | 16 (11%) | 12 (10%) | 4 (14%) | 0 | ns | ns | ns | |
| Severe (N/%) | 24 (16%) | 19 (17%) | 4 (14%) | 1 (20%) | ||||
| Itch/paresthesia (N/%) | 20 (13%) | 18 (16%) | 2 (7%) | 0 | ns | ns | ns | |
| Urinary incontinence (N/%) | 1 (1%) | 1 (1%) | 0 | 0 | - | - | - | |
| Fatigue (N/%) | 4 (3%) | 1 (1%) | 2 (7%) | 1 (20%) | - | - | - | |
| Vision problems (N/%) | 2 (1%) | 1 (1%) | 1 (3%) | 0 | - | - | - | |
| Cognitive impairment (N/%) | 0 | 0 | 0 | 0 | - | - | - | |
| Back pain from spinal puncture (N/%) | 18 (12%) | 15 (13%) | 2 (7%) | 1 (20%) | ns | ns | ns | |
| Muscular spasms (N/%) | 1 (1%) | 1 (1%) | 0 | 0 | - | - | - | |
| Tremor (N/%) | 1 (1%) | 1 (1%) | 0 | 0 | - | - | - | |
| Chills/warm feeling (N/%) | 14 (9%) | 11 (10%) | 2 (7%) | 1 (20%) | ns | ns | ns | |
| Changed tasting experience (N/%) | 3 (2%) | 2 (2%) | 1 (3%) | 0 | - | - | - | |
Non-serious adverse events were common, independent of administration protocol (Table 2). No symptoms at all after intrathecal contrast administration were reported by 23%, 31%, and 20% of patients for protocols #1, #2, and #3, respectively. The severity of nausea was weaker in individuals with protocol #3 as compared with protocol #2 (P = 0.004), providing preliminary evidence that occurrence of non-serious adverse events of intrathecal gadobutrol are dose-dependent. Otherwise, the occurrence of other non-serious adverse events did not differ significantly between protocols.
The occurrence of non-serious adverse events after 4 weeks and 12 months is presented in Table 3. After 12 months, two patients (1 %) reported urinary incontinence, but with unclear association to the administration protocol, as both had other diseases that might explain these complaints. No other individuals reported complaints related to participation in the project.
Table 3.
Non-serious adverse events after 4 weeks and 12 months
| 4 weeks | 12 months | ||
|---|---|---|---|
| Headache (N/%) | 10 (7%) | 2 (1%) | |
| Severity | Mild (N/%) | 2 (1%) | 0 |
| Moderate (N/%) | 4 (3%) | 0 | |
| Severe (N/%) | 4 (3%) | 0 | |
| Nausea (N/%) | 4 (3%) | 0 | |
| Severity | Mild (N/%) | 0 | 0 |
| Moderate (N/%) | 1 (1%) | 0 | |
| Severe (N/%) | 3 (2%) | 0 | |
| Dizziness (N/%) | 4 (3%) | 0 | |
| Severity | Mild (N/%) | 1 (1%) | 0 |
| Moderate (N/%) | 2 (1%) | 0 | |
| Severe (N/%) | 1 (1%) | 0 | |
| Itch/paresthesia (N/%) | 4 (3%) | 0 | |
| Urinary incontinence | 2 (1%) | 2 (1%) | |
| Fatigue | 1 (1%) | 0 | |
| Vision problems | 1 (1%) | 0 | |
| Cognitive impairment | 0 | 0 | |
| Back pain from spinal puncture | 2 (1%) | 0 | |
| Muscular spasms | 0 | 0 | |
| Tremor | 0 | 0 | |
| Chills/warm feeling | 0 | 0 | |
| Changed tasting experience | 0 | 0 | |
Data presented as number of individuals (percentage in parenthesis)
Non-serious adverse events depending on clinical indication for MRI
The non-serious adverse events during days 1–3 heavily depended on clinical diagnosis (Table 4). While 37% of individual with iNPH did not reported any non-serious adverse events, the same numbers were 0% and 14% for individuals with a pineal gland cyst or idiopathic intracranial hypertension (IIH), respectively. The occurrence and severity of headache, nausea, and dizziness differed significantly between clinical diagnoses (Table 4).
Table 4.
Non-serious adverse events days 1–3 depending on clinical indication for intrathecal gadobutrol
| Days 1–3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| iNPH (n = 38) | SIH (n = 22) | AC (n = 27) | PC (n = 26) | IIH (n = 22) | cHC (n = 11) | ncHC (n = 3) | Significance | ||
| No non-serious adverse events (N/%) | 14 (37%) | 5 (23%) | 10 (37%) | 0 | 3 (14%) | 3 (27%) | 1 (33%) | P = 0.016 | |
| Headache (N/%) | 6 (16%) | 10 (46%) | 9 (33%) | 22 (85%) | 15 (68%) | 6 (55%) | 1 (33%) | P < 0.001 | |
| Severity | Mild (N/%) | 1 (3%) | 2 (9%) | 0 | 0 | 5 (23%) | 0 | 0 | |
| Moderate (N/%) | 3 (8%) | 5 (23%) | 3 (11%) | 4 (15%) | 0 | 2 (18%) | 0 | P < 0.001 | |
| Severe (N/%) | 2 (5%) | 3 (14%) | 6 (22%) | 18 (69%) | 10 (46%) | 4 (36%) | 1 (33%) | ||
| Nausea (N/%) | 18 (47%) | 11 (50%) | 12 (44%) | 21 (81%) | 14 (64%) | 6 (55%) | 2 (67%) | ns | |
| Severity | Mild (N/%) | 7 (18%) | 6 (27%) | 5 (19%) | 3 (12%) | 1 (5%) | 2 (18%) | 1 (33%) | |
| Moderate (N/%) | 1 (3%) | 2 (9%) | 2 (7%) | 1 (4%) | 4 (18%) | 1 (9%) | 0 | P = 0.044 | |
| Severe (N/%) | 10 (26%) | 3 (14%) | 5 (19%) | 17 (65%) | 9 (41%) | 3 (27%) | 1 (33%) | ||
| Dizziness (N/%) | 6 (16%) | 7 (32%) | 12 (44%) | 20 (77%) | 12 (55%) | 2 (18%) | 1 (33%) | P < 0.001 | |
| Severity | Mild (N/%) | 5 (13%) | 4 (18%) | 5 (19%) | 3 (12%) | 3 (14%) | 0 | 0 | |
| Moderate (N/%) | 1 (3%) | 2 (9%) | 2 (7%) | 7 (27%) | 3 (14%) | 0 | 1 (33%) | P < 0.001 | |
| Severe (N/%) | 0 | 1 (5%) | 5 (19%) | 10 (39%) | 6 (27%) | 2 (18%) | 0 | ||
| Itch/paresthesia (N/%) | 2 (5%) | 4 (18%) | 3 (11%) | 8 (31%) | 1 (5%) | 1 (9%) | 1 (33%) | ns | |
| Urinary incontinence | 0 | 1 (5%) | 0 | 0 | 0 | 0 | 0 | ||
| Fatigue | 0 | 0 | 1 (4%) | 2 (8%) | 1 (5%) | 0 | 0 | ns | |
| Vision problems | 0 | 0 | 0 | 0 | 1 (5%) | 1 (9%) | 0 | ||
| Cognitive impairment | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Back pain from spinal puncture | 1 (3%) | 1 (5%) | 3 (11%) | 8 (31%) | 3 (14%) | 2 (18%) | 0 | P = 0.032 | |
| Muscular spasms | 0 | 1 (5%) | 0 | 0 | 0 | 0 | 0 | ||
| Tremor | 0 | 1 (5%) | 0 | 0 | 0 | 0 | 0 | ||
| Chills/warm feeling | 3 (8%) | 1 (5%) | 2 (7%) | 5 (19%) | 3 (14%) | 0 | 0 | ns | |
| Changed tasting experience | 0 | 0 | 0 | 1 (4%) | 1 (5%) | 0 | 1 (33%) | ||
Data presented as number of individuals (percentage in parenthesis). Significance determined by the Pearson chi-square test. Data presented as number of individuals (percentage in parenthesis). iNPH idiopathic normal pressure hydrocephalus, SIH spontaneous intracranial hypotension, AC arachnoid cyst, PC pineal cyst, IIH idiopathic intracranial hypertension, cHC communicating hydrocephalus, ns non-significant
After 4 weeks, particularly the occurrence and severity of headache differed significantly between diagnosis categories (Table 5). Among individuals with pineal cysts and IIH, 12% and 18% reported headache.
Table 5.
Non-serious adverse events after 4 weeks depending on clinical indication for intrathecal gadobutrol
| 4 weeks | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| iNPH (n = 38) | SIH (n = 22) | AC (n = 27) | PC (n = 26) | IIH (n = 22) | cHC (n = 11) | ncHC (n = 3) | Significance | ||
| No non-serious adverse events (N/%) | 35 (92%) | 19 (86%) | 24 (89%) | 21 (81%) | 17 (77%) | 10 (91%) | 2 (67%) | ns | |
| Headache (N/%) | 0 | 1 (5%) | 1 (4%) | 3 (12%) | 4 (18%) | 0 | 1 (33%) | P = 0.042 | |
| Severity | Mild (N/%) | 0 | 0 | 1 (4%) | 0 | 0 | 0 | 1 (33%) | |
| Moderate (N/%) | 0 | 1 (5%) | 0 | 1 (4%) | 2 (9%) | 0 | 0 | P = 0.002 | |
| Severe (N/%) | 0 | 0 | 0 | 2 (8%) | 2 (9%) | 0 | 0 | ||
| Nausea (N/%) | 0 | 0 | 0 | 1 (4%) | 3 (14%) | 0 | 0 | ||
| Severity | Mild (N/%) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Moderate (N/%) | 0 | 0 | 0 | 0 | 1 (5%) | 0 | 0 | ns | |
| Severe (N/%) | 0 | 0 | 0 | 1 (4%) | 2 (9%) | 0 | 0 | ||
| Dizziness (N/%) | 1 (3%) | 0 | 1 (4%) | 0 | 2 (9%) | 0 | 0 | ||
| Severity | Mild (N/%) | 0 | 0 | 0 | 0 | 1 (5%) | 0 | 0 | |
| Moderate (N/%) | 1 (3%) | 0 | 1 (4%) | 0 | 0 | 0 | 0 | ns | |
| Severe (N/%) | 0 | 0 | 0 | 0 | 1 (5%) | 0 | 0 | ||
| Itch/paresthesia (N/%) | 1 (3%) | 1 (5%) | 1 (4%) | 0 | 1 (5%) | 0 | 0 | ||
| Urinary incontinence | 0 | 1 (5%) | 0 | 1 (4%) | 0 | 0 | 0 | ||
| Fatigue | 1 (3%) | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Vision problems | 0 | 0 | 0 | 0 | 1 (5%) | 0 | 0 | ||
| Cognitive impairment | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Back pain from spinal puncture | 0 | 0 | 1 (4%) | 1 (4%) | 0 | 0 | 0 | ||
| Muscular spasms | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Tremor | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Chills/warm feeling | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Changed tasting experience | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
Data presented as number of individuals (percentage in parenthesis). Significance determined by the Pearson chi-square test. Data presented as number of individuals (percentage in parenthesis). iNPH idiopathic normal pressure hydrocephalus, SIH spontaneous intracranial hypotension, AC arachnoid cyst, PC pineal cyst, IIH idiopathic intracranial hypertension, cHC communicating hydrocephalus, ns non-significant
Discussion
The main result of this prospective study is that intrathecal gadobutrol in doses of either 0.25 or 0.5 mmol caused no serious adverse events in individuals without prior history of allergic reactions to contrast agents. The frequency of non-serious adverse events after days 1–3 or 4 weeks was primarily determined by the tentative patient diagnosis prior to intrathecal injection. There were no definitive adverse events after 12 months.
The clinical indications for intrathecal gadobutrol in this study were various forms of suspected CSF circulation disorders, where gadobutrol at the same time served as a CSF tracer as part of our gMRI protocol [21]. We administered gadobutrol off-label based on special permission from the National Medicines Agency of Norway, in a standardized research setting only. However, intrathecal MRI contrast agents in similar concentrations have previously been used clinically off-label to visualize CSF leakage in individuals with spontaneous intracranial hypotension (SIH) [22, 23] and otorhinorrhea [24], as well as in the diagnostic assessment of disorders such as arachnoid cysts [25] and iNPH [26].
The safety profile of gadolinium-based contrast agents was recently reviewed in this journal; the authors concluded that no cause-effect relationship has been shown in humans regarding brain gadolinium exposure and clinical consequences specific to neurological toxicity [8]. Previously, several studies found the linear contrast agent gadopentetic acid to have low risk when given intrathecally to patients in a dose 0.5–1.0 mmol [22, 27–31]. A recent systematic review concluded that serious adverse events of intrathecal administered MRI contrast agents are highly dose-dependent; the observed serious adverse events were seen after administration of 2 mmol or higher doses [10]. Non-serious adverse events, primarily headache, occurred following doses of 1 mmol or lower, but they were not able to conclude about the cause since headache occurs post lumbar puncture in about 49% of patients [10]. Headache also was the most common non-serious adverse event in the present study. In comparison, intrathecal gadopentetic acid caused headache in 10/36 (27%) iNPH patients [26] and in 6/20 (30%) patients with arachnoid cysts [31].
The available evidence points to a small gap between advantageous diagnostic effects and neurotoxic effects of intrathecal MRI contrast agents. From our experience, intrathecal gadobutrol in a dose of 0.5 mmol or less is safe, which in an adult with a brain weighing 1400 g represents an exposure 0.36 μmol/g gadobutrol to brain. Intrathecal gadobutrol in a dose of 2.0 mmol or higher may cause neurotoxic effects. It was previously reported in humans that overdose of gadopentetic acid (6–20 times normal dose) could be neurotoxic [32, 33]. One individual who by accident received 20 mmol gadopentetic acid (7.0 μmol/g brain) developed neurological deficits (speech problems, visual impairment, fatigue, and psychotic symptoms) lasting 2 weeks, but symptoms had disappeared after 2 months [34]. Intrathecal gadobutrol in a dose of 2.0 mmol caused spastic pain of the lower extremities [35]. Recently, another study reported fatal outcome in a 67-year-old person who by accident received 2.0 mmol gadoteridol, corresponding to a concentration 2.3 μmol/g brain [36]. The authors reviewed the literature about neurotoxic effects of intrathecal gadolinium; the literature reports no neurological complications after doses causing concentration of < 1.0 μmol/g brain [36].
Taken together, the existing data suggest intrathecal gadobutrol in a dose of 0.5 mmol (corresponding to a dose of 0.36 μmol gadobutrol per gram brain) to be safe. Nevertheless, the present study provides preliminary data that gadobutrol in a dose of 0.25 mmol causes less severe nausea than 0.5 mmol. Since only five individuals received 0.25 mmol, this need to be further studied. We further note that intrathecal gadobutrol in a dose of 0.25 mmol provided strong enrichment within CSF of cisterna magna, though the CSF tracer level was significantly lower than 3, 6, and 48 h after a dose of 0.5 mmol. Nevertheless, a dose of 0.25 mmol may be considered sufficient for diagnosis of CSF leaks from the spinal canal or at the skull base. We will explore the clinical utility of this dose in future studies where intrathecal gadobutrol is used as CSF tracer to assess the glymphatic system and craniospinal molecular clearance capacity.
It should be noted that the present comparison of different administration protocols was hampered by the diagnostic categories allocated to the respective administration protocols. The frequency of non-serious adverse events heavily depended on the clinical indication for intrathecal gadobutrol. It is well recognized that IIH and symptomatic pineal gland cysts may sometimes be accompanied with severe symptoms such as headache, nausea, and dizziness [37, 38], which overlap with symptoms typically seen after intrathecal contrast agent injections. Furthermore, headache is a predominant symptom in individuals with symptomatic arachnoid cysts [39]. Adding iohexanol as in protocol #1 would be expected to increase occurrence of adverse events [40]. This effect was, however, not seen here, probably related to the substantial contribution of symptoms from the diagnoses pineal gland cyst, IIH, and arachnoid cyst to the adverse event profile. Taken together, given the high proportion of individuals with a pineal cyst or IIH in protocol #2 (42%) than in protocol #1 (30%; Table 1), this probably explains the higher frequency of the non-serious adverse events headache, nausea, and dizziness in days 1–3 with protocol #2.
One concern regarding intrathecal use of MRI contrast agents is the potential for deposition within brain parenchyma. In a previous study, 4 week after one single intrathecal administration of 0.5 mmol gadobutrol, we found no detectable change in normalized T1 signal in any brain region, including basal ganglia indicative of no retention [21]. Moreover, it is important to bear in mind that it is now established that after an ordinary clinical intravenous dose of gadolinium, the contrast agent is present in CSF samples for days and weeks, even despite normal renal function and intact blood-brain barrier [14, 15]. One study of rodents reported that the concentration of MRI contrast agent in CSF exceeded that of blood 4.5 h after intravenous administration [17]. A typical intravenous dose (0.1 mmol/kg in an 80-kg patient = 8 mmol and with half-time in blood being approximately 2 h) may therefore, theoretically, render for a notable passage of contrast agent to CSF, as recently shown in an MRI study [16]. The difference in peak CSF concentration of gadobutrol after conventional intravenous dose compared with intrathecal doses of 0.5 or 0.25 mmol remains to be determined. This may potentially be quantified with MRI using T1-maps, allowing for quantification of gadobutrol concentration in different locations intracranially.
The clinical use of intrathecal MRI contrast agents would require acceptable balance between safety and added diagnostic value, as compared with best available methods. Given the probable small therapeutic index of intrathecal MRI contrast agents, the relative safety and diagnostic advantage need to be further studied.
Conclusion
This prospective study showed that intrathecal administration of 0.5 and 0.25 mmol gadobutrol was safe. Non-serious adverse events were only to a small degree affected by different administration protocols. Preliminary data are given that a lower dose 0.25 mmol of intrathecal gadobutrol may be favorable, but this needs to be further studied. Frequency of non-serious adverse events was highest among patients under work-up for IIH and pineal gland cysts, who typically present with symptoms comparable with some of those reported after intrathecal administration of contrast agents.
Acknowledgements
Open Access funding provided by University of Oslo (incl Oslo University Hospital).
Funding information
This study was funded by the Department of neurosurgery, Oslo University Hospital - Rikshospitalet.
Compliance with ethical standards
This research study was approved by the Institutional Review Board (2015/1868), Regional Ethics Committee (2015/96) and the National Medicines Agency (15/04932-7).
Conflict of interest
Author Geir Ringstad has received a speaker fee from Bayer AG. The other authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
MH and CSE contributed equally to this work.
References
- 1.Iliff JJ, Wang M, Liao Y, Plogg BA, Peng W, Gundersen GA, Benveniste H, Vates GE, Deane R, Goldman SA, Nagelhus EA, Nedergaard M. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid beta. Sci Transl Med. 2012;4(147):147ra111. doi: 10.1126/scitranslmed.3003748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rasmussen MK, Mestre H, Nedergaard M. The glymphatic pathway in neurological disorders. Lancet Neurol. 2018;17(11):1016–1024. doi: 10.1016/s1474-4422(18)30318-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iliff JJ, Lee H, Yu M, Feng T, Logan J, Nedergaard M, Benveniste H. Brain-wide pathway for waste clearance captured by contrast-enhanced MRI. J Clin Invest. 2013;123(3):1299–1309. doi: 10.1172/jci67677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang L, Kress BT, Weber HJ, Thiyagarajan M, Wang B, Deane R, Benveniste H, Iliff JJ, Nedergaard M. Evaluating glymphatic pathway function utilizing clinically relevant intrathecal infusion of CSF tracer. J Transl Med. 2013;11:107. doi: 10.1186/1479-5876-11-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eide PK, Vatnehol SAS, Emblem KE, Ringstad G. Magnetic resonance imaging provides evidence of glymphatic drainage from human brain to cervical lymph nodes. Sci Rep. 2018;8(1):7194. doi: 10.1038/s41598-018-25666-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ringstad G, Eide PK. Cerebrospinal fluid tracer efflux to parasagittal dura in humans. Nat Commun. 2020;11(1):354. doi: 10.1038/s41467-019-14195-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eide PK, Valnes LM, Pripp AH, Mardal KA, Ringstad G (2019) Delayed clearance of cerebrospinal fluid tracer from choroid plexus in idiopathic normal pressure hydrocephalus. J Cereb Blood Flow Metab:271678x19874790. 10.1177/0271678x19874790 [DOI] [PMC free article] [PubMed]
- 8.Mallio CA, Rovira À, Parizel PM, Quattrocchi CC. Exposure to gadolinium and neurotoxicity: current status of preclinical and clinical studies. Neuroradiology. 2020;62:925–934. doi: 10.1007/s00234-020-02434-8. [DOI] [PubMed] [Google Scholar]
- 9.Kanal E (2020) A reality check on intrathecal gadolinium-based contrast agents. Radiology:202819. 10.1148/radiol.2020202819 [DOI] [PubMed]
- 10.Patel M, Atyani A, Salameh JP, McInnes M, Chakraborty S (2020) Safety of intrathecal administration of gadolinium-based contrast agents: a systematic review and meta-analysis. Radiology:191373. 10.1148/radiol.2020191373 [DOI] [PubMed]
- 11.Kanda T, Ishii K, Kawaguchi H, Kitajima K, Takenaka D. High signal intensity in the dentate nucleus and globus pallidus on unenhanced T1-weighted MR images: relationship with increasing cumulative dose of a gadolinium-based contrast material. Radiology. 2014;270(3):834–841. doi: 10.1148/radiol.13131669. [DOI] [PubMed] [Google Scholar]
- 12.Gulani V, Calamante F, Shellock FG, Kanal E, Reeder SB. Gadolinium deposition in the brain: summary of evidence and recommendations. Lancet Neurol. 2017;16(7):564–570. doi: 10.1016/s1474-4422(17)30158-8. [DOI] [PubMed] [Google Scholar]
- 13.Radbruch A, Haase R, Kieslich PJ, Weberling LD, Kickingereder P, Wick W, Schlemmer HP, Bendszus M. No signal intensity increase in the dentate nucleus on unenhanced T1-weighted MR images after more than 20 serial injections of macrocyclic gadolinium-based contrast agents. Radiology. 2017;282(3):699–707. doi: 10.1148/radiol.2016162241. [DOI] [PubMed] [Google Scholar]
- 14.Berger F, Kubik-Huch RA, Niemann T, Schmid HR, Poetzsch M, Froehlich JM, Beer JH, Thali MJ, Kraemer T. Gadolinium distribution in cerebrospinal fluid after administration of a gadolinium-based MR contrast agent in humans. Radiology. 2018;288(3):703–709. doi: 10.1148/radiol.2018171829. [DOI] [PubMed] [Google Scholar]
- 15.Nehra AK, McDonald RJ, Bluhm AM, Gunderson TM, Murray DL, Jannetto PJ, Kallmes DF, Eckel LJ, McDonald JS. Accumulation of gadolinium in human cerebrospinal fluid after gadobutrol-enhanced MR imaging: a prospective observational cohort study. Radiology. 2018;288(2):416–423. doi: 10.1148/radiol.2018171105. [DOI] [PubMed] [Google Scholar]
- 16.Cao D, Kang N, Pillai JJ, Miao X, Paez A, Xu X, Xu J, Li X, Qin Q, Van Zijl PCM, Barker P, Hua J (2020) Fast whole brain MR imaging of dynamic susceptibility contrast changes in the cerebrospinal fluid (cDSC MRI). Magn Reson Med. 10.1002/mrm.28389 [DOI] [PMC free article] [PubMed]
- 17.Jost G, Frenzel T, Lohrke J, Lenhard DC, Naganawa S, Pietsch H. Penetration and distribution of gadolinium-based contrast agents into the cerebrospinal fluid in healthy rats: a potential pathway of entry into the brain tissue. Eur Radiol. 2017;27(7):2877–2885. doi: 10.1007/s00330-016-4654-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deike-Hofmann K, Reuter J, Haase R, Paech D, Gnirs R, Bickelhaupt S, Forsting M, Heußel CP, Schlemmer HP, Radbruch A. Glymphatic pathway of gadolinium-based contrast agents through the brain: overlooked and misinterpreted. Invest Radiol. 2019;54(4):229–237. doi: 10.1097/rli.0000000000000533. [DOI] [PubMed] [Google Scholar]
- 19.Edeklev CS, Halvorsen M, Lovland G, Vatnehol SAS, Gjertsen O, Nedregaard B, Sletteberg R, Ringstad G, Eide PK. Intrathecal use of gadobutrol for glymphatic MR imaging: prospective safety study of 100 patients. AJNR Am J Neuroradiol. 2019;40(8):1257–1264. doi: 10.3174/ajnr.A6136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ringstad G, Vatnehol SAS, Eide PK. Glymphatic MRI in idiopathic normal pressure hydrocephalus. Brain. 2017;140(10):2691–2705. doi: 10.1093/brain/awx191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ringstad G, Valnes LM, Dale AM, Pripp AH, Vatnehol SS, Emblem KE, Mardal KA, Eide PK (2018) Brain-wide glymphatic enhancement and clearance in humans assessed with MRI. JCI insight 3(13). 10.1172/jci.insight.121537 [DOI] [PMC free article] [PubMed]
- 22.Akbar JJ, Luetmer PH, Schwartz KM, Hunt CH, Diehn FE, Eckel LJ. The role of MR myelography with intrathecal gadolinium in localization of spinal CSF leaks in patients with spontaneous intracranial hypotension. AJNR Am J Neuroradiol. 2012;33(3):535–540. doi: 10.3174/ajnr.A2815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Selcuk H, Albayram S, Ozer H, Ulus S, Sanus GZ, Kaynar MY, Kocer N, Islak C. Intrathecal gadolinium-enhanced MR cisternography in the evaluation of CSF leakage. AJNR Am J Neuroradiol. 2010;31(1):71–75. doi: 10.3174/ajnr.A1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nacar Dogan S, Kizilkilic O, Kocak B, Isler C, Islak C, Kocer N. Intrathecal gadolinium-enhanced MR cisternography in patients with otorhinorrhea: 10-year experience of a tertiary referral center. Neuroradiology. 2018;60(5):471–477. doi: 10.1007/s00234-018-2014-4. [DOI] [PubMed] [Google Scholar]
- 25.Tali ET, Ercan N, Kaymaz M, Pasaoglu A, Jinkins JR. Intrathecal gadolinium (gadopentetate dimeglumine)-enhanced MR cisternography used to determine potential communication between the cerebrospinal fluid pathways and intracranial arachnoid cysts. Neuroradiology. 2004;46(9):744–754. doi: 10.1007/s00234-004-1240-0. [DOI] [PubMed] [Google Scholar]
- 26.Algin O, Hakyemez B, Ocakoglu G, Parlak M. MR cisternography: is it useful in the diagnosis of normal-pressure hydrocephalus and the selection of “good shunt responders”? Diagn Interv Radiol. 2011;17(2):105–111. doi: 10.4261/1305-3825.dir.3133-09.1. [DOI] [PubMed] [Google Scholar]
- 27.Aydin K, Guven K, Sencer S, Jinkins JR, Minareci O. MRI cisternography with gadolinium-containing contrast medium: its role, advantages and limitations in the investigation of rhinorrhoea. Neuroradiology. 2004;46(1):75–80. doi: 10.1007/s00234-003-1004-2. [DOI] [PubMed] [Google Scholar]
- 28.Aydin K, Terzibasioglu E, Sencer S, Sencer A, Suoglu Y, Karasu A, Kiris T, Turantan MI. Localization of cerebrospinal fluid leaks by gadolinium-enhanced magnetic resonance cisternography: a 5-year single-center experience. Neurosurgery. 2008;62(3):584–589. doi: 10.1227/01.neu.0000317306.39203.24. [DOI] [PubMed] [Google Scholar]
- 29.Jinkins JR, Rudwan M, Krumina G, Tali ET. Intrathecal gadolinium-enhanced MR cisternography in the evaluation of clinically suspected cerebrospinal fluid rhinorrhea in humans: early experience. Radiology. 2002;222(2):555–559. doi: 10.1148/radiol.2222010249. [DOI] [PubMed] [Google Scholar]
- 30.Reiche W, Komenda Y, Schick B, Grunwald I, Steudel WI, Reith W. MR cisternography after intrathecal Gd-DTPA application. Eur Radiol. 2002;12(12):2943–2949. doi: 10.1007/s00330-002-1606-9. [DOI] [PubMed] [Google Scholar]
- 31.Tali ET, Ercan N, Krumina G, Rudwan M, Mironov A, Zeng QY, Jinkins JR. Intrathecal gadolinium (gadopentetate dimeglumine) enhanced magnetic resonance myelography and cisternography: results of a multicenter study. Invest Radiol. 2002;37(3):152–159. doi: 10.1097/00004424-200203000-00008. [DOI] [PubMed] [Google Scholar]
- 32.Li L, Gao FQ, Zhang B, Luo BN, Yang ZY, Zhao J. Overdosage of intrathecal gadolinium and neurological response. Clin Radiol. 2008;63(9):1063–1068. doi: 10.1016/j.crad.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 33.Park KW, Im SB, Kim BT, Hwang SC, Park JS, Shin WH. Neurotoxic manifestations of an overdose intrathecal injection of gadopentetate dimeglumine. J Korean Med Sci. 2010;25(3):505–508. doi: 10.3346/jkms.2010.25.3.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Arlt S, Cepek L, Rustenbeck HH, Prange H, Reimers CD. Gadolinium encephalopathy due to accidental intrathecal administration of gadopentetate dimeglumine. J Neurol. 2007;254(6):810–812. doi: 10.1007/s00415-006-0439-x. [DOI] [PubMed] [Google Scholar]
- 35.Reeves C, Galang E, Padalia R, Tran N, Padalia D. Intrathecal injection of gadobutrol: a tale of caution. J Pain Palliat Care Pharmacother. 2017;31(2):139–143. doi: 10.1080/15360288.2017.1313353. [DOI] [PubMed] [Google Scholar]
- 36.Provenzano DA, Pellis Z, DeRiggi L. Fatal gadolinium-induced encephalopathy following accidental intrathecal administration: a case report and a comprehensive evidence-based review. Reg Anesth Pain Med. 2019;44:721–729. doi: 10.1136/rapm-2019-100422. [DOI] [PubMed] [Google Scholar]
- 37.Eide PK, Pripp AH, Ringstad GA. Magnetic resonance imaging biomarkers indicate a central venous hypertension syndrome in patients with symptomatic pineal cysts. J Neurol Sci. 2016;363:207–216. doi: 10.1016/j.jns.2016.02.038. [DOI] [PubMed] [Google Scholar]
- 38.Fric R, Eide PK. Comparative observational study on the clinical presentation, intracranial volume measurements, and intracranial pressure scores in patients with either Chiari malformation type I or idiopathic intracranial hypertension. J Neurosurg. 2017;126(4):1312–1322. doi: 10.3171/2016.4.JNS152862. [DOI] [PubMed] [Google Scholar]
- 39.Pradilla G, Jallo G. Arachnoid cysts: case series and review of the literature. Neurosurgical focus. 2007;22(2):E7. doi: 10.3171/foc.2007.22.2.7. [DOI] [PubMed] [Google Scholar]
- 40.Palmers Y, Kuhn FP, Petersen D, De Greef D. Comparison in myelography between iodixanol 270 and 320 mgI/ml and iotrolan 300 mgI/ml: a multicentre, randomised, parallel-group, double-blind, phase III trial. Eur Radiol. 2002;12(3):686–691. doi: 10.1007/s003300100881. [DOI] [PubMed] [Google Scholar]