Abstract
Background
Mask wearing has been shown to be an effective strategy for slowing the spread of COVID-19. While early studies have uncovered some evidence of racial and ethnic differences in mask-wearing behavior, critical gaps remain. We begin to address these gaps by (1) more comprehensively investigating the role of race and ethnicity on mask wearing during the COVID-19 pandemic and (2) examining whether gender intersects with race and ethnicity to differently influence mask-wearing patterns.
Methods
Data were drawn from the COVID-19 Impact Survey, a cross-sectional, nationally representative survey of adults living in the U.S. Data were pooled from three time points that ranged from late April 2020 to early June 2020. The final analytic sample consisted of 4688 non-institutionalized adults living in the U.S. A series of logistic regression models with robust standard errors were used to estimate differences in mask-wearing patterns.
Results
Compared with White respondents, results revealed Black, Latina/o, and Asian respondents were more likely to report wearing a mask in response to the coronavirus. Moreover, results show White men were least likely to wear a mask from late April 2020 to early June 2020.
Conclusion
Overall, findings demonstrate mask-wearing patterns during the COVID-19 pandemic are differently shaped by racial and ethnic background and gender. Findings from this study can inform targeted strategies designed to increase mask-wearing adherence among U.S. adults.
Keywords: COVID-19, Mask wearing, Race and ethnicity, Gender
Introduction
Evidence of a new highly pathogenic coronavirus emerged in Wuhan, China, in late December 2019. The novel virus, now known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes coronavirus disease 2019 (COVID-19), quickly spread to other countries after the first cluster of cases was discovered. On March 11, 2020, the World Health Organization (WHO) declared COVID-19 to be a pandemic, and by October 12, 2020, there were more than 37 million confirmed cases and 800,000 deaths worldwide. The first U.S. case of COVID-19 was reported on January 20, and as of late October 2020, the U.S. had the highest number of confirmed cases and deaths compared with other countries [1].
In response to the rising rates of COVID-19 cases in the U.S., public health experts, government agencies, and elected officials promoted and, in some cases, enforced a myriad of community mitigation strategies designed to curb the rate of infections and deaths. For instance, mask wearing, a relatively low-cost mitigation strategy, was mandated in some states beginning in early April [2]. Mask wearing has been a part of health and safety guidance messages during previous infectious disease outbreaks [3, 4] and has been shown to be an effective strategy in reducing the spread of respiratory droplets containing coronaviruses [5–7]. Recent forecasts show near-universal mask wearing could prevent approximately 74,000 deaths from mid-October to late February 2021 [8].
Although mask wearing is widely considered an effective strategy in slowing the spread of COVID-19, some state and local officials have been reluctant to issue mask-wearing mandates, citing civil liberty and enforcement concerns. For instance, at the time of this article, only 33 states had issued policies requiring face coverings in public spaces [2]. To further compound this challenge, many states and localities with face-covering mandates have been unable to achieve widespread adherence. Reports of patrons and activist groups protesting facemask policies continue to emerge throughout the U.S. [9–12].
Public health policies perceived by some to be invasive and disruptive to social life can be difficult to implement, given that they require a great deal of trust in government and health officials [13]. Understanding which groups are more or less likely to comply with mask-wearing recommendations and mandates is vital to slowing and stopping the spread of COVID-19. Early research suggests that racial background shapes mask-wearing patterns during the COVID-19 pandemic. For instance, using a sample of adults living in California, Texas, and Florida in April 2020, Papageorge and colleagues [14] find Black Americans were more likely to wear masks when compared with their White counterparts. While not a central focus on their study, Capraro and Barcelo [15] find older adults, along with Black and Asian respondents, report a greater intention of wearing a face covering. While these findings provide interesting insights into the role of race on mask-wearing adherence patterns during the COVID-19 pandemic, the dearth of research in this area has yet to examine broader racial and ethnic differences in mask-wearing adherence, focusing exclusively on Black-White differences or excluding other important ethnic groups, such as Latina/os.
A large body of scholarship suggests potentially stark differences in mask-wearing adherence by race and ethnicity during infectious disease outbreaks. In the U.S., racial and ethnic divides permeate every aspect of social life, including risk and response during a pandemic [16, 17]. Divisions along racial and ethnic lines appeared early in the COVID-19 pandemic as residents of Asian descent were largely blamed for rising infection rates and deaths [18]. Moreover, historically marginalized racial and ethnic groups have been disproportionally impacted by the pandemic [19]. According to the CDC [20], Black and Latina/o adults are more likely to become infected, be hospitalized due to severe illness, and die from COVID-19 complications when compared with White people. While Asian Americans do not present an increased risk of death from COVID-19, virologic surveillance data indicate Asian Americans are more likely to be become infected and be hospitalized when compared with White people.
To understand racial inequalities in the context of COVID-19 infections, hospitalizations, and deaths, it is important to consider broader racialized social structures that have historically created differential access to resources, opportunities, and risks [21, 22]. More specifically, racism, as a structured system of domination designed to justify and perpetuate a racial hierarchy, has enabled White people to amass a set of flexible resources (e.g., power, prestige, wealth, and social capital) that drive health disparities. For example, Black Americans and Latina/os have less wealth [23], lower household median income [24], higher rates of unemployment [25], and are less likely to receive a college degree [26] when compared with their White counterparts. Historically marginalized racial and ethnic groups also tend to receive poorer-quality health care and less intensive care than White people, even when accounting for socioeconomic status, age, and health condition [27].
The deep and persistent inequities in social and economic resources, coupled with pervasive discriminatory practices in economic, educational, and healthcare sectors, place substantial limits on the type and amount of resources historically marginalized racial groups can access to avoid disease, receive effective treatments, and engage in healthy lifestyles [28]. As a result, we argue that the continued racial and ethnic inequities in COVID-19 infections, hospitalizations, and deaths, in addition to the broad spectrum of structural inequities that limit access to superior social, economic, and health resources, may lead to greater mask-wearing adherence for historically marginalized groups when compared with White people. Using pooled data from the COVID Impact Survey, we test this assertion by examining whether mask wearing significantly differ across racial and ethnic background from late April to early June 2020.
There is also early evidence that gender shapes mask-wearing adherence. For instance, during the SARS-COV-1 outbreak in 2003, research indicates that men exhibited poorer mask-wearing practices when compared with their female counterparts [29]. With respect to the COVID-19 pandemic, Haischer and colleagues [30] found, among shoppers in Wisconsin, women were more likely to wear masks during the month of June, July, and early August. Moreover, Capraro and Barcelo [15] found that men are more likely to view mask wearing as “shameful,” “not cool,” a “sign of weakness,” and a “stigma” when compared with women. Intersectional scholars have theorized and empirically demonstrated that due to structured systems that systematically disadvantage minoritized groups, both race and ethnicity and gender jointly and simultaneously shape economic, social, and health disparities. By applying this framework to emerging evidence that gender plays a role in mask wearing, we also examine whether gender intersects with race and ethnicity to influence mask-wearing patterns during the COVID-19 pandemic.
Methods
Data
Our analyses used pooled data from the COVID Impact Survey (CIS). Funded and managed by the Data Foundation, the CIS is a cross-sectional, nationally representative household survey designed to provide estimates for preventative behaviors, physical and mental health, economic security, and other social dynamics during the COVID-19 pandemic. CIS data were collected using the AmeriSpeak Panel, a probability-based panel distributed by NORC at the University of Chicago. U.S. households were sampled with a known, non-zero probability of selection from the NORC National Sample Frame and then contacted by U.S. mail, e-mail, telephone, and field interviewers. Once CIS samples were selected, fielded, and finalized, an iterative raking process was used to adjust for any survey non-response, as well as any under- or oversampling resulting from the study-specific sample design. At the time of the manuscript, CIS data from three time points were available: time 1 (April 20–26, n = 2190), time 2 (May 4–10, n = 2238), and time 3 (May 30–June 8, n = 2047). The analytic sample included respondents from all three time points. Listwise deletion was used to obtain our final sample (n = 4688). We applied appropriate longitudinal sampling weights to account for the complex design of the CIS. When weighted, data were representative of non-institutionalized adults residing in the U.S.
Measures
Dependent Variable
Our primary outcome for this study is mask-wearing adherence from late April, 2020 to early June, 2020. Across all three time points, the CIS captured self-reports of whether respondents wore a mask in response to the coronavirus. Responses were coded such that Yes = 1 and No = 0.
Independent Variables
Race/ethnicity is measured using a respondent’s self-reported racial and ethnic identity, which includes categories for White (reference), Black, Latina/o, and Asian/Asian American. Gender is measured using a dummy variable for female, with male as the reference. Control variables included time of interview, age, household income, level of education, marital status, region, work status, health insurance, and self-reported physical health.
Analytic Strategy
We begin by providing descriptives statistics for all measures included in the study. We then provide logistic regression estimates that assess the role of racial and ethnic background on mask-wearing adherence during the COVID-19 pandemic. Finally, we included eight dummy variables (White men, White women, Black men, Black women, Latina/o men, Latina/o women, Asian men, Asian women) to investigate race/ethnic/gender differences in mask-wearing adherence. All logistic regression models present coefficients in odds ratios with robust standard errors in parentheses.
Results
The weighted descriptive statistics for all measures included in this study are presented in Table 1. Results indicate that the majority of respondents (84%) reported wearing a mask in response to the coronavirus. With respect to racial and ethnic background, the largest proportion of the sample was White (67%), followed by Latina/os (18%), Black (13%), and Asian (3%) respondents. The pooled sample consisted primarily of observations collected at time 1 (43%) followed by observations at time 2 (38%) and time 3 (20%). Approximately half of the respondents were female (51%), married (50%), and employed (52%). Respondents between the ages of 18 and 29 years represented 14% of the sample, and those between 30 and 44 years were 30% of the sample. People 45 years and older but younger than 60 were 23% of the sample, and those 60 years or older were 33% of the sample. Most of the sample either had earned a college degree (35%) or completed some college level courses (41%). Regarding household income, 36% of respondents reported an income of less than $40,000, 29% reported an income between $40,000 and $75,000, and 35% reported an income of greater than $75,000. Finally, most of the sample had health insurance (91%) and reported good or excellent health (84%).
Table 1.
Descriptive statistics (n = 4688)
| Variable | Mean | S.D. |
|---|---|---|
| Mask wearing | 0.84 | 0.36 |
| Race and ethnicity | ||
| Black | 0.13 | 0.33 |
| Latina/o | 0.18 | 0.38 |
| Asian | 0.03 | 0.17 |
| White | 0.67 | 0.47 |
| Gender | ||
| Male | 0.49 | 0.50 |
| Time points | ||
| Time 1 | 0.43 | 0.49 |
| Time 2 | 0.38 | 0.48 |
| Time 3 | 0.20 | 0.40 |
| Age | ||
| 18–29 | 0.14 | 0.35 |
| 30–44 | 0.30 | 0.46 |
| 45–59 | 0.23 | 0.42 |
| 60+ | 0.33 | 0.47 |
| Household income | ||
| < $40,000 | 0.36 | 0.48 |
| $40,000–> $75,000 | 0.29 | 0.45 |
| $75,000–150,000+ | 0.35 | 0.48 |
| Education | ||
| No high school diploma | 0.05 | 0.22 |
| High school diploma | 0.18 | 0.39 |
| Some college | 0.41 | 0.49 |
| College graduate | 0.35 | 0.48 |
| Marital status | ||
| Married | 0.50 | 0.50 |
| Region | ||
| Northeast | 0.15 | 0.36 |
| Midwest | 0.24 | 0.42 |
| South | 0.36 | 0.48 |
| West | 0.26 | 0.44 |
| Employment status | ||
| Employed | 0.52 | 0.50 |
| Retired/not interested in working | 0.31 | 0.46 |
| Unemployed due to COVID | 0.11 | 0.32 |
| Unemployed before COVID/looking | 0.06 | 0.25 |
| Insured | 0.91 | 0.29 |
| Poor mental health | 7.61 | 3.30 |
| Self-rated health | 0.84 | 0.36 |
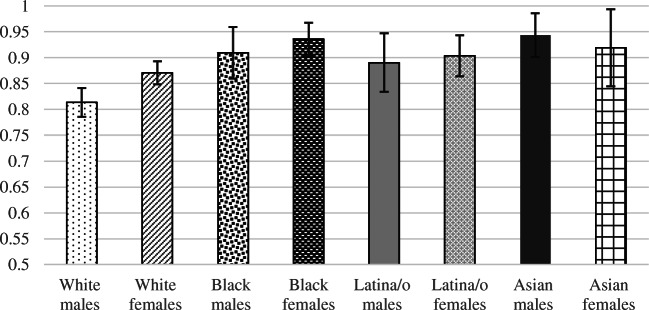
Table 2 contains logistic regression estimates that assess racial and ethnic differences in mask wearing during the COVID-19 pandemic. After adjusting for confounding variables, results demonstrate that racial and ethnic background plays a significant role in mask wearing from late April to early June 2020. Compared with White respondents, Black (OR = 2.24, p < .001), Latina/o (OR = 1.62, p < .05), and Asian (OR = 2.87, p < .001) respondents are more likely to wear a mask in response to the coronavirus pandemic. To more clearly illustrate our findings, the results of this analysis are presented in Fig. 1 as predicted probabilities. With control variables at their observed values, Asian respondents had the highest average probability of mask wearing (0.94), followed by Black (0.92), Latina/o (0.89), and White (0.84) respondents. Consistent with prior studies, estimates from Table 2 also show males (OR = 0.69, p < .01) were less likely than females to report wearing a mask.
Table 2.
Logistic regression estimates predicting mask-wearing adherence in response to the coronavirus (n = 4688)
| OR(SE) | |
|---|---|
| Race and ethnicity | |
| Black | 2.24 (0.48)*** |
| Latina/o | 1.62 (0.34)* |
| Asian | 2.87 (0.95)*** |
| Gender | |
| Male | 0.69 (0.08)** |
| Timing | |
| Wave 2 | 1.23 (0.16) |
| Wave 3 | 1.79 (0.29)*** |
| Age | |
| 30–44 | 1.08 (0.20) |
| 45–59 | 1.21 (0.24) |
| 60+ | 1.95 (0.45)** |
| Income | |
| $40,000–> $75,000 | 1.13 (0.17) |
| $75,000–150,000+ | 1.54 (0.26)** |
| Education | |
| No high school diploma | 0.90 (0.27) |
| High school diploma or equivalent | 0.70 (0.12)* |
| Some college | 0.74 (0.10)* |
| Marital status | |
| Married | 1.01 (0.13) |
| Region | |
| Midwest | 2.91 (0.74)*** |
| South | 0.64 (0.11)** |
| West | 0.62 (0.10)** |
| Work status | |
| Retired/not interested in working | 1.07 (0.17) |
| Unemployed due to COVID | 1.00 (0.21) |
| Unemployed before COVID/looking | 1.09 (0.27) |
| Health insurance | |
| Insured | 1.05 (0.21) |
| Poor mental health | 1.05 (0.03) |
| Self-reported physical health | |
| Good-to-excellent health | 1.06 (0.18) |
*p < .05; **p < .01; ***p < .001
Fig. 1.
Predicted probability of mask wearing by race and ethnicity
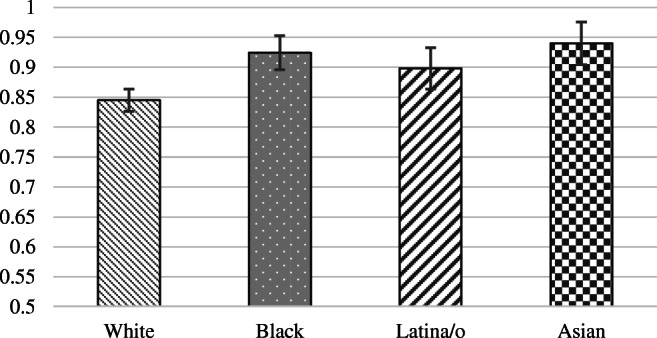
Table 3 presents logistic regression estimates for the relationships between race/ethnic/gender combinations and mask-wearing adherence during the COVID-19 pandemic. Results demonstrate, when compared with White men, the odds of mask use to prevent the spread of the coronavirus were higher for White women (OR = 1.54, p < .001), Black men (OR = 2.30, p < .01), Black women (OR = 3.34, p < .001), Latina/o men (OR = 1.86, p < .05), Latina/o women (OR = 2.15, p < .01), and Asian men (OR = 3.83, p < .001). The difference between White men and Asian women is only marginally significant (OR = 2.61, p < .10). To further illustrate differences in mask wearing by race/ethnicity/gender combinations, Fig. 2 depicts the predicted probability of mask-wearing adherence for each race/ethnicity/gender combination. Results indicate that, when compared with White men, the predicted probability of wearing a mask was almost 13 percentage points higher for Asian men, 12 percentage points higher for Black women, 10 percentage points higher for Black men, 9 percentage point higher for Latinas, and 8 percentage points for Latinos. We also observe notable differences between White men and women—with White women demonstrating a 6% greater probability of wearing a mask.
Table 3.
Logistic regression estimates predicting mask wearing by race/ethnicity/gender combinations (n = 4688)
| OR (SE) | |
|---|---|
| Race and ethnicity | |
| White women | 1.54 (0.20)*** |
| Black men | 2.30 (0.73)** |
| Black women | 3.34 (0.94)*** |
| Latina/o men | 1.86 (0.58)* |
| Latina/o women | 2.15 (0.54)** |
| Asian men | 3.83 (1.59)*** |
| Asian women | 2.61 (1.36)+ |
| Timing | |
| Time point 2 | 1.23 (0.16) |
| Time point 3 | 1.79 (0.29)*** |
| Age | |
| 30–44 | 1.08 (0.20) |
| 45–59 | 1.21 (0.24) |
| 60+ | 1.95 (0.45)** |
| Income | |
| $40,000–> $75,000 | 1.13 (0.17) |
| $75,000–150,000+ | 1.54 (0.26)** |
| Education | |
| No high school diploma | 0.90 (0.27) |
| High school diploma or equivalent | 0.70 (0.12)* |
| Some college | 0.74 (0.10)* |
| Marital status | |
| Married | 1.01 (.13) |
| Region | |
| Midwest | 2.91 (0.74)*** |
| South | 0.64 (0.11)** |
| West | 0.62 (0.10)** |
| Work status | |
| Retired/not interested in working | 1.07 (0.17) |
| Unemployed due to COVID | 1.00 (0.21) |
| Unemployed before COVID/looking | 1.09 (0.27) |
| Health insurance | |
| Insured | 1.05 (0.21) |
| Poor mental health | 1.05 (0.03) |
| Self-reported physical health | |
| Good-to-excellent health | 1.06 (0.18) |
*p < .05; **p < .01; ***p < .001
Fig. 2.
Predicted probability of mask wearing by race and ethnicity and gender
Given that there are limited studies on mask-wearing adherence during the COVID-19 pandemic, it is worthwhile to highlight to a few key patterns that emerged from our covariates. Results from Table 3 show that respondents surveyed at time point 3 (May 30–June 8) were more likely (OR = 1.79, p < .001) to wear a mask compared with those surveyed at time point 1 (April 20–26). We also find respondents over the age of 60 years were more likely than the youngest group of respondents (18 to 29 years) to wear a mask (OR = 1.95, p < .01). With respect to household income, the odds of a respondent in the highest income bracket ($75,000+) wearing a mask were greater than the odds of those in the lowest income bracket (< $40,000) (OR = 1.54, p < .01). We also observe clear differences in mask wearing across educational background. Compared with those with a college degree, respondents with a high school diploma (OR = 0.70, p < .05) and those who completed some college courses (OR = 0.74, p < .05) were less likely to wear a mask. Finally, we find that when compared with respondents living in the northeast region of the U.S., respondents living in the Midwest (OR = 2.91, p < .001) were more likely to report mask usage, whereas respondents living in the southern (OR = 0.64, p < .01) and western (OR = 0.62, p < .01) regions of the U.S. were less likely to report using a mask in response to the coronavirus.
Discussion
Evidence consistently suggests that wearing a face covering can significantly reduce COVID-19 infection rates, as well as hospitalizations and death related to the novel coronavirus. To slow the spread of COVID-19, government and public health officials have promoted, and in some cases, enforced the use of facemasks in public spaces. Despite overwhelming evidence that face coverings reduce the spread of coronaviruses, the U.S. has been unable to achieve widespread adherence to this preventative behavior. As a result, identifying groups that are more or less likely to comply with mask-wearing recommendations and mandates is vital to slowing and stopping the spread of COVID-19 [31].
Our first objective was to evaluate to what extent variation in mask wearing during the COVID-19 pandemic is shaped by racial and ethnic background. Drawing on pooled nationally representative data from COVID-19 Impact Survey, we find racial and ethnic background to be an essential driver of mask wearing during the COVID-19 pandemic. Findings demonstrate that all three historically marginalized groups (Black, Latina/o, and Asian) included in this study were more likely to report wearing a mask during this time period. There are a number of potential mechanisms that may explain the greater reluctance among White people, and in particular White men, to wear masks when compared with other racial and ethnic groups. First, when compared with other racial and ethnic groups, White people are the least likely to become infected, to be hospitalized, and to die from COVID-19 [32]. Thus, White people may be less likely to believe that they are at risk of infection and death due to COVID-19 and, therefore, choose not to wear masks. Second, while there is no evidence White people possess biological or genetic advantages with respect to COVID-19, White people often have fewer underlying health conditions that are tied to serious illness from COVID-19. Milder symptoms among White people may, again, reinforce the belief that COVID-19 is not a major threat to health, and thus the use of a mask is unnecessary. Third, White people are less likely to work in sectors of the labor markets that increase the risk of exposure to the novel coronavirus by failing to adopt occupational health protections [33]. That is, White workers are often less likely to be exposed to COVID-19 on the job and, consequently, may opt out of wearing a mask. Finally, White people have greater access to social and economic resources that can be utilized in the event that someone within the family becomes infected and/or hospitalized with COVID-19. The ability to rely on social and economic resources may lessen the pressure to wear a face mask for protection.
Our second objective was to determine whether the intersections of race and ethnicity and gender played a significant role in mask wearing. Our regression estimates show substantial race and ethnicity and gender differences in mask wearing from late April 2020 to early June 2020. White men had the lowest probability of wearing mask, while Asian men had the highest probability of wearing a mask. Moreover, White women had the second lowest probability, followed by Latina/o men, Latina/o women, Black men, and Black women. Overall, these findings show that racial and ethnic differences in mask wearing are not equivalent across gender, with White men showing the greatest reluctance to mask wearing during the COVID-19 pandemic.
What are the potential sources that can help explain these differences? Racist and sexist structures often overlap, creating a convergence of deepening social, economic, and health inequities that may shape mask-wearing patterns. Recent reports show that White men continue to out earn Black and Latina/o men and women [34]. Moreover, White men have more wealth than White women, and men and women of other racial and ethnic groups [35]. Beyond economic resources, studies also find White men have lower perceptions of risk when compared with women and men from other racial and ethnic groups [36–39]. Lower perceptions of risk may be further compounded by perceptions of what mask wearing represents. Studies find men are more likely to view mask wearing as less masculine, which can potentially act as a deterrent to the preventative behavior when in public [40]. Taken together, the economic advantages coupled with lower perceptions of risk and hegemonic views of masks may help to explain why White men were the least likely to report wearing a mask in response to COVID-19.
Limitations
This study is not without limitations. First, while this is one of the first studies to examine the role of race and ethnicity and gender on mask wearing during the COVID-19 pandemic, the measure capturing mask-wearing adherence is limited in several ways. Most prominently, the questionnaire assessed whether a respondent wore a mask in response to the coronavirus and did not account for frequency of use. Unfortunately, our data source also did not capture other important contextual elements related to mask wearing, such as the setting in which a mask was used (i.e., public or private space), whether a respondent was required to wear a mask in a workplace setting, and/or whether a respondent was living in a state or locality with a mandatory face mask ordinance. Given these limitations, future research should investigate the role of race and ethnicity and gender on more nuanced measures of mask wearing, such as the frequency of use and the context of use.
Second, findings only account for mask0wearing behavior from late April to early June. Since early June, COVID-19 infections and deaths have continued to increase. For example, by early October, the U.S. recorded more than 7.5 million COVID-19 cases, and the number of COVID-19-related deaths exceeded 200,000. Given these realities, future research should investigate whether mask-wearing adherence changed from earlier months and whether changes in mask wearing varied according to race and ethnicity and gender. Third, patterns observed in this study are only reflective of mask use in the U.S. Given the varied countrywide responses to mask wearing, as well as the unique history of race and racism and sexism in the U.S., results from this study may not be applicable to other countries. Finally, future studies should consider other structural, psychological, and behavioral mechanisms that might underlie relationships between race and ethnicity and gender and mask wearing.
Despite these limitations, we advance the understanding of mask-wearing adherence during the COVID-19 pandemic in two central ways. First, our findings show that, on average, historically marginalized racial groups were more likely to engage in mask wearing in response to the COVID-19 pandemic when compared with their White counterparts. Generally, public health education programs and marketing strategies designed to educate people on the importance of mask wearing have targeted the general population. Our results indicate that public health professionals should develop programs that target specific racial and ethnic groups. Second, our results also suggest targeted mask-wearing programs may benefit from adopting an intersectional approach, focusing on the importance of both race and ethnicity and gender. More specifically, given that we find White men were the least likely to engage in mask wearing, public health education programs designed to educate White men on the importance of mask wearing would be well justified.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Brittany N. Hearne and Michael D. Niño shared equal authorship
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Brittany N. Hearne, Email: bnhearne@uark.edu
Michael D. Niño, Email: mdnino@uark.edu
References
- 1.John Hopkins Coronavirus Resource Center. 2020 COVID-19 case tracker. https://coronavirus.jhu.edu/.
- 2.Kim A, Andrew S, Froio J. These are the states requiring people to wear masks when out in public. CNN. 2020. https://www.cnn.com/2020/06/19/us/states-face-mask-coronavirus-trnd/index.html. Accessed 1 Oct 2020.
- 3.Blendon RJ, DesRoches CM, Cetron MS, Benson JM, Meinhardt T, Pollard W. Attitudes toward the use of quarantine in a public health emergency in four countries: the experiences of Hong Kong, Singapore, Taiwan, and the United States are instructive in assessing national responses to disease threats. Health Aff. 2006;25(Suppl1):W15–W25. doi: 10.1377/hlthaff.25.w15. [DOI] [PubMed] [Google Scholar]
- 4.McCoy CA. The railway switches of history: the development of disease control in Britain and the United States in the 19th and early 20th century. J Hist Sociol. 2017;30(3):650–673. doi: 10.1111/johs.12099. [DOI] [Google Scholar]
- 5.Leung K, Wu JT, Liu D, Leung GM. First-wave COVID-19 transmissibility and severity in China outside Hubei after control measures, and second-wave scenario planning: a modelling impact assessment. Lancet. 2020;395(10233):1382–1393. doi: 10.1016/S0140-6736(20)30746-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liang M, Gao L, Cheng C, Zhou Q, Uy JP, Heiner K, Sun C. Efficacy of face mask in preventing respiratory virus transmission: a systematic review and meta-analysis. Travel Med Infect Dis. 2020;36:101751. doi: 10.1016/j.tmaid.2020.101751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ma QX, Shan H, Zhang HL, Li GM, Yang RM, Chen JM. Potential utilities of mask-wearing and instant hand hygiene for fighting SARS-CoV-2. J Med Virol. 2020;92(9):1567–1571. doi: 10.1002/jmv.25805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Institute of Health Metrics. COVID-19 death projections. 2020. Retrieved from: https://covid19.healthdata.org/united-states-of-america?view=resourceuse&tab=trend&resource=all_resources. Accessed 10 Oct 2020.
- 9.Mervosh S, Fernandez M, Robertson C. Mask rules expand across U.S. as clashes over the mandates intensify. The New York Times. 2020. https://www.nytimes.com/2020/07/16/us/coronavirus-masks.html. Accessed 1 Oct 2020.
- 10.Moore B. About 150 protesters march against Illinois’ school face mask mandate. The State Journal-Register. 2020. https://www.sj-r.com/news/20200725/about-150-protesters-march-against-illinoisrsquo-school-face-mask-mandate. Accessed 1 Oct 2020.
- 11.Stewart E. Anti-maskers explain themselves. Vox. 2020. https://www.vox.com/the-goods/2020/8/7/21357400/anti-mask-protest-rallies-donald-trump-covid-19. Accessed 1 Oct 2020.
- 12.Rojas R. Masks become a flashpoint in the virus culture wars. Seattle Times. 2020. https://www.nytimes.com/2020/05/03/us/coronavirus-masks-protests.html. Accessed 1 Oct 2020.
- 13.Fukuyama, F. The thing that determines a country’s resistance to the coronavirus. The Atlantic. 2020. https://www.theatlantic.com/ideas/archive/2020/03/thing-determines-howwell-countries-respond-coronavirus/609025/. Accessed 1 Oct 2020.
- 14.Papageorge NW, Zahn MV, Belot M., van den Broek-Altenburg E, Choi S, Jamison JC, Tripodi, E. Socio-demographic factors associated with self-protecting behavior during the COVID-19 pandemic. Institute of Labor Economics (IZA). 2020;1–53. [DOI] [PMC free article] [PubMed]
- 15.Capraro V, Barcelo H. The effect of messaging and gender on intentions to wear a face covering to slow down COVID-19 transmission. J Behav Econ Policy. 2020;4(2):45–55. [Google Scholar]
- 16.Plough A, Bristow B, Fielding J, Caldwell S, Khan S. Pandemics and health equity: lessons learned from the H1N1 response in Los Angeles County. J Public Health Manag Pract. 2011;17(1):20–27. doi: 10.1097/PHH.0b013e3181ff2ad7. [DOI] [PubMed] [Google Scholar]
- 17.Quinn SC, Kumar S, Freimuth VS, Musa D, Casteneda-Angarita N, Kidwell K. Racial disparities in exposure, susceptibility, and access to health care in the US H1N1 influenza pandemic. Am J Public Health. 2011;101(2):285–293. doi: 10.2105/AJPH.2009.188029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tessler H, Choi M, Kao G. The anxiety of being Asian American: hate crimes and negative biases during the COVID-19 pandemic. Am J Crim Justice. 2020;10:1–11. doi: 10.1007/s12103-020-09541-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Raifman MA, Raifman JR. Disparities in the population at risk of severe illness from covid-19 by race/ethnicity and income. Am J Prev Med. 2020;59(1):137–139. doi: 10.1016/j.amepre.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. Health equity considerations and racial and ethnic minority groups. 2020. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html. Accessed 5 Oct 2020.
- 21.Phelan JC, Link BG. Is racism a fundamental cause of inequalities in health? Annu Rev Sociol. 2015;41:311–330. doi: 10.1146/annurev-soc-073014-112305. [DOI] [Google Scholar]
- 22.Williams DR, Sternthal M. Understanding racial-ethnic disparities in health: sociological contributions. J Health Soc Behav. 2010;51(1):S15–S27. doi: 10.1177/0022146510383838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sullivan L, Meschede T. How measurement of inequalities in wealth by race/ethnicity impacts narrative and policy: investigating the full distribution. Race Soc Probl. 2018;10(1):19–29. doi: 10.1007/s12552-017-9217-x. [DOI] [Google Scholar]
- 24.U.S. Census Bureau. real median household income by race and Hispanic origin: 1967-2017. 2020. https://www.census.gov/content/dam/Census/library/visualizations/2018/demo/p60-263/figure1.pdf. Accessed 15 Sept 2020.
- 25.U.S. Bureau of Labor Statistics. Household data, not seasonally adjusted, quarterly averages: Unemployment rates by age, sex, race, and Hispanic or Latino ethnicity. 2020. https://www.bls.gov/web/empsit/cpsee_e16.htm. Accessed 15 Sept 2020.
- 26.Ogunwole SU, Drewery MP, Rios-Vargas M. The population with a bachelor’s degree or higher by race and Hispanic origin: 2006–2010. United States Census. 2012. https://www2.census.gov/library/publications/2012/acs/acsbr10-19.pdf. Accessed 15 Sept 2020.
- 27.Institute of Medicine . Unequal treatment: confronting racial and ethnic disparities in health care. Washington: National Academy of Press; 2003. [PubMed] [Google Scholar]
- 28.Cockerham WC, Bauldry S, Hamby BW, Shikany JM, Bae S. A comparison of black and white racial differences in health lifestyles and cardiovascular disease. Am J Prev Med. 2017;52(1):S56–S62. doi: 10.1016/j.amepre.2016.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lau JT, Yang X, Tsui HY, Pang E. SARS related preventive and risk behaviours practised by Hong Kong-mainland China cross border travelers during the outbreak of the SARS epidemic in Hong Kong. J Epidemiol Community Health. 2004;58(12):988–996. doi: 10.1136/jech.2003.017483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Haischer MH, Beilfuss R, Hart MR, Opielinski L, Wrucke D, Zirgaitis G, Hunter SK. Who is wearing a mask? Gender-, age-, and location-related differences during the COVID-19 pandemic. MedRxiv.2020; 1–17. [DOI] [PMC free article] [PubMed]
- 31.Van Bavel JJ, Baicker K, Boggio PS, Capraro V, Cichocka A, Cikara M, Drury J. Using social and behavioural science to support COVID-19 pandemic response. Nat Hum Behav. 2020;4(5):460–447. doi: 10.1038/s41562-020-0884-z. [DOI] [PubMed] [Google Scholar]
- 32.Gross CP, Essien UR, Pasha S, Gross JR, Wang SY, Nunez-Smith M. Racial and ethnic disparities in population level Covid-19 mortality. J Gen Intern Med. 2020;35(10):3097–3099. doi: 10.1007/s11606-020-06081-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McClure ES, Vasudevan P, Bailey Z, Patel S, Robinson WR. Racial capitalism within public health: how occupational settings drive COVID-19 disparities. Am J Epiemiol. 2020;189:1244–1253. doi: 10.1093/aje/kwaa126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Patten E. Racial, gender wage gaps persist in U.S. despite some progress. Pew Research Center. 2016. https://www.pewresearch.org/fact-tank/2016/07/01/racial-gender-wage-gaps-persist-in-u-s-despite-some-progress/. Accessed 1 Oct 2020.
- 35.Insight Center for Community Economic Development. Lifting as we climb: women of color, wealth, and America’s future. 2010. https://static1.squarespace.com/static/5c50b84131d4df5265e7392d/t/5c5c7801ec212d4fd499ba39/1549563907681/Lifting_As_We_Climb_InsightCCED_2010.pdf. Accessed 1 Oct 2020.
- 36.Finucane ML, Slovic P, Mertz CK, Flynn J, Satterfield TA. Gender, race, and perceived risk: the white male effect. Health Risk Soc. 2000;2(2):159–172. doi: 10.1080/713670162. [DOI] [Google Scholar]
- 37.Kahan DM, Braman D, Gastil J, Slovic P, Mertz CK. Culture and identity-protective cognition: explaining the white-male effect in risk perception. J Empir Leg Stud. 2007;4(3):465–505. doi: 10.1111/j.1740-1461.2007.00097.x. [DOI] [Google Scholar]
- 38.Kalof L, Dietz T, Guagnano G, Stern PC. Race, gender and environmentalism: the atypical values and beliefs of white men. Race Class Gen. 2002;9(2):112–130. [Google Scholar]
- 39.Palmer C. Risk perception: another look at the white male effect. Health Risk Soc. 2003;5(1):721–783. doi: 10.1080/1369857031000066014. [DOI] [Google Scholar]
- 40.Palmer CL, Peterson RD. Toxic mask-ulinity: the link between masculine toughness and affective reactions to mask wearing in the COVID-19 era. Politics Gen. 2020;9:1–8. [Google Scholar]