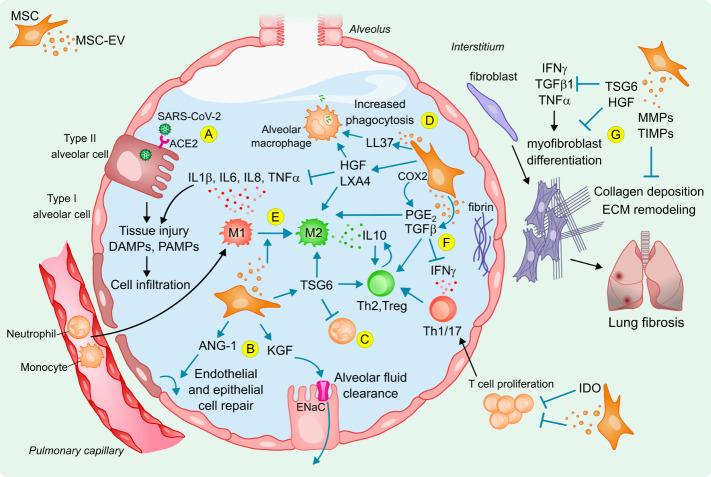
Figure 2.
Potential mechanisms of action of MSCs and derived EVs to reduce lung injury in acute respiratory distress syndrome following SARS-CoV-2 infection. (A) SARS-CoV-2 infection causes cell and tissue injury, release of DAMPs, PAMPs and inflammatory mediators that are sensed by neighbouring cells and alveolar macrophages that amplify an inflammatory response in the alveolus, promoting immune cell infiltration and accumulation of protein-rich alveolar oedema fluid. Infused MSCs and derived EVs can reduce inflammation and trigger tissue repair by (B) increasing alveolar fluid clearance and have anti-apoptotic and anti-oxidative effects to restore injured alveolar, epithelial and endothelial cells; (C) reducing neutrophil activation, which also decreases inflammatory cell infiltration; (D) enhancing phagocytosis and viability of alveolar macrophages; (E) reducing inflammation and inducing M2 polarisation of monocytes that results in IL-10 production to induce (F) regulatory T cells and Th2 switch from Th1 and Th17 responses, together with a modulation of T-cell proliferation; (G) protecting from lung fibrosis. ANG-1, angiopoietin-1; COX2, cyclooxygenase-2; DAMPs, danger-associated molecular patterns; ECM, extracellular matrix; ENaC, epithelial sodium channel; HGF, hepatocyte growth factor; IDO, indoleamine 2,3-dioxygenase; IFNγ, interferon gamma; IL, interleukin; KGF, keratinocyte growth factor; LL37, antimicrobial peptide β-cathelicidin; LXA4, lipoxin A4; MMP, matrix metalloproteinase; MSC, mesenchymal stem cell; MSC-EV, MSC-derived extracellular vesicles; PAMPs, pathogen-associated molecular patterns; PGE2, prostaglandin E2; TGFβ, transforming growth factor beta; TIMP, tissue inhibitor of MMP; TNF-α, tumour necrosis factor alpha; Treg, regulatory T-cell; TSG-6, TNF‐stimulated gene 6 protein.