Abstract
A 66-year-old gentleman with no prior cardiac history presented with dyspnea on exertion and chest pain for 1 month. His workup included a transthoracic echocardiogram, which demonstrated findings suggestive of cor triatriatum (C-TAT) with uncertain degree of hemodynamic obstruction. In addition, mild left ventricular systolic dysfunction and segmental wall motion abnormalities suggestive of coronary artery disease were noted. The patient then underwent transesophageal echocardiography (TEE) to define better the structural characteristics and hemodynamic significance of the C-TAT, left and right heart catheterization to assess pressure gradients between the upper and lower left atrial chambers by simultaneous measurement of pulmonary capillary wedge and left ventricular end-diastolic pressures, and coronary angiography. Multiplane 2-dimensional TEE demonstrated an atrial membrane extending from the inferior portion of the interatrial septum to the superior aspect of the lateral atrial wall. This membrane exhibited a medial large oval opening with bidirectional flow and a ≤2 mm Hg gradient. Three-dimensional TEE imaging re-demonstrated this obliquely oriented membrane; however, of most importance, it revealed that the membrane divided the atria into a medial funnel and C-shaped cavity with a large distal oval shape opening and an even larger lateral atrial cavity. These findings were inconsistent with a true C-TAT and rather demonstrated what we defined as a pseudo-C-TAT membrane. Simultaneous right and left heart catheterization confirmed a minimal gradient of 3 to 5 mm Hg and coronary angiography demonstrated severe 3-vessel coronary disease as the primary cause of the patient’s clinical syndrome.
Keywords: cardiology, diagnostic testing, radiology, imaging
Cor triatriatum (C-TAT) is a rare congenital heart defect (0.1% to 0.4% in postmortem series) in which the left or rarely the right atrium is subdivided into 2 atrial chambers by a tissue membrane.1 Typically, the tissue membrane subdivides the atrium into a more proximal or superior, and a more distal or inferior compartment. It is typically diagnosed in infancy as many of these membranes effect hemodynamics, presenting as a supravalvular mitral stenosis.
In this article, we present the case of an elderly patient with dyspnea on exertion and chest pain who was found to have a left atrial membrane suggestive of C-TAT. This membrane was investigated to define its structural and hemodynamic characteristics as there was concern for it causing the patient’s clinical syndrome.
A 66-year-old gentleman with no relevant prior cardiac history presented with dyspnea on exertion and chest pain. The dyspnea on exertion and chest pain started 10 hours prior to being seen in the emergency department. The pain was described as both dull and sharp and it was mainly right sided on presentation. In the emergency department, the patient had 2 sets of negative troponins, a negative chest X-ray, and a negative electrocardiogram. A D-dimer was drawn, which was elevated. Due to chronic kidney disease, the patient underwent a VQ scan that showed intermediate probability of pulmonary embolism and then was admitted to medicine for further diagnostic testing and care.
As part of his workup, the patient underwent a transthoracic echocardiogram (TTE). His TTE demonstrated findings suggestive of C-TAT with an uncertain degree of hemodynamic obstruction (Figure 1A and B) in addition, mild left ventricular systolic dysfunction, and segmental wall motion abnormalities suggestive of underlying coronary artery disease (CAD) were noted. To better determine the hemodynamic significance of patient’s apparent C-TAT and underlying CAD, the patient underwent a transesophageal echocardiogram (TEE) followed by right and left heart catheterization. Multiplane 2-dimensional TEE demonstrated an atrial membrane extending from the inferior portion of the interatrial septum to the superior aspect of the lateral atrial wall with a large medial inferior opening (Figure 1C and D) with bidirectional flow and mild (≤2 mm Hg) gradient (Figure 1E-G). By this technique, the left and right upper pulmonary veins appeared to enter the medial atrial cavity (Figure 1H and I) and their normal flow patterns (systolic to diastolic flow velocities ratio of >1) further supported normal left atrial pressure. However, the entrance of the left and right lower pulmonary veins could not be determined. Three-dimensional (3D) TEE imaging demonstrated a curvilinear membrane extending from the inferomedial to superior aspects of the atria and therefore dividing the atria into a medial funnel and C-shaped cavity with a large distal and oval shape opening, and a larger lateral atrial cavity (Figure 2A-D). Also, these 3D TEE images clearly show the membrane attaching to the anteromedial and posteromedial, but not to the inferomedial aspects of the atrial wall. Altogether, these findings are inconsistent with a true C-TAT and rather are consistent with what we defined as a pseudo-C-TAT membrane.
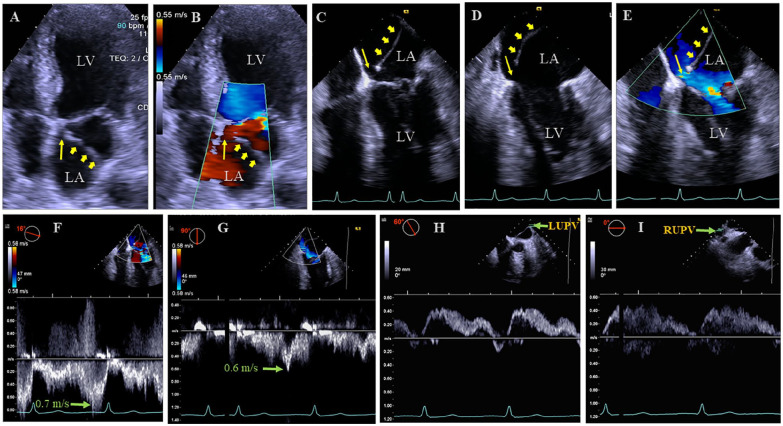
Figure 1.
(A) This transthoracic echocardiogram (TTE) 4-chamber view shows the apparent C-TAT membrane (wide arrows) with a medial opening (thin arrow). (B) This TTE 4-chamber view with color Doppler shows flow across the membrane (wide arrows) medial opening (thin arrow). (C and D) These transesophageal echocardiogram (TEE) 4- and 2-chamber views demonstrate the atrial membrane (wide arrows) extending from the inferomedial to the superolateral aspect of the left atrium (LA) with a large medial opening (thin arrows). (E) This TEE 4-chamber view with color Doppler shows flow across the medial opening of membrane (thin arrow). (F and G) These TEE 4- and 2-chamber views with pulsed wave Doppler sampling across the medial opening of the membrane shows bidirectional flow with very low peak velocities up to 0.7 m/s, equivalent to a very low gradient of ≤2 mm Hg (4 × [0.7]2). (H and I) This TEE views with pulsed wave Doppler demonstrate the entrance of the left (H) and right (I) upper pulmonary veins into the medial aspect of the LA. LV, left ventricle; LUPV and RUPV, left and right upper pulmonary veins, respectively.
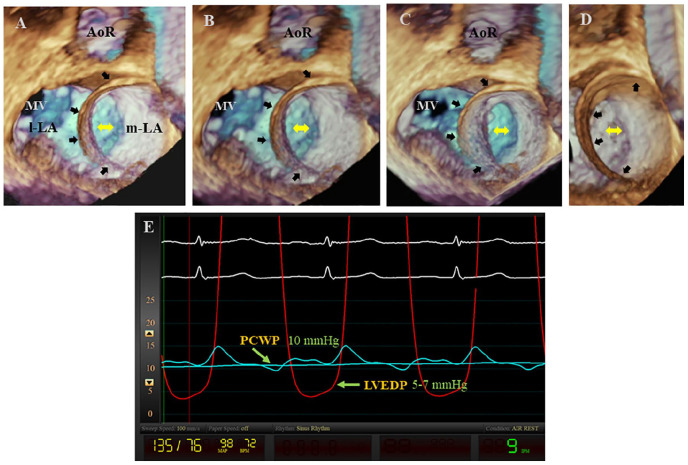
Figure 2.
(A-D) These 3-dimensional transesophageal echocardiogram (TEE) views from the left atrium (LA) at different orientations demonstrate a well-defined curvilinear membrane (wide arrows) extending from the inferomedial to the superior regions of the atria and therefore dividing the LA into a funnel and C-shaped medial LA (m-LA) cavity with a large distal and oval shape opening (double-headed arrows) and an even larger and also C-shaped lateral LA (l-LA) cavity. Note that the membrane appears to attach to the anteromedial and posteromedial, but not to the inferomedial aspects of the atrial wall. (E) This simultaneous recording of the pulmonary capillary wedge pressure (PCWP) and left ventricular pressure demonstrate a mean PCWP of 10 mm Hg and a left ventricular end-diastolic pressure (LVEDP) of 5 to 7 mm Hg and, therefore, a differential gradient of 3 to 5 mm Hg. MV, mitral valve; AoR, aortic root.
The differential diagnosis for this patient’s dyspnea on exertion and chest pain included pulmonary embolism as supported by the intermediate probability V/Q scan and elevated D-dimer, acute coronary syndrome (unstable angina), and less likely obstruction from the apparent pseudo-C-TAT membrane. Therefore, the patient underwent treatment for pulmonary embolism and CAD, while further testing occurred to further delineate a diagnosis. In the cardiac catheterization laboratory, simultaneous recording of the mean pulmonary capillary wedge pressure of 10 mm Hg and left ventricular end-diastolic pressure of 5 to 7 mm Hg (Figure 2E) verified a minimal differential gradient of 3 to 5 mm Hg. As this gradient was considered either physiologically normal or minimally elevated, it was determined that this membrane was not obstructive and therefore not contributing to the patient’s symptoms. Coronary angiography demonstrated severe 3 vessel CAD as the primary cause of patient’s clinical syndrome.
Due to the patient’s possible pulmonary embolism, he was treated with oral anticoagulation for a minimum of 3 months, after which the patient underwent uncomplicated coronary bypass surgery with left internal mammary artery to the left anterior descending artery and saphenous vein bypass grafts to 2 obtuse marginal branches and his right coronary artery. The patient was discharged home as he symptomatically and clinically improved. Expectedly, no intervention is currently planned for the patient’s atrial membrane mimicking C-TAT.
Cor triatriatum is a rare congenital heart defect that typically presents earlier in life with symptomatic heart failure.2,3 It has been rarely reported in the adult and elderly population.4,5 It is surmised that this patient had a curvilinear membrane extending from the inferomedial to the superior aspects of the atria dividing the atrium into a left or lateral and right or medial chambers with a large distal opening in the medial chamber and therefore leading to a physiologic to minimally elevated gradient of no hemodynamic consequences. These findings are inconsistent with a true C-TAT. To our knowledge, this is the first case of a pseudo C-TAT detected and best characterized by 3D TEE imaging. Therefore, adult or elderly patients with cardiovascular symptoms and an atrial membrane suggestive of C-TAT on TTE should undergo 3D TEE imaging to better define the anatomy and hemodynamic consequences of the membrane. This would better classify patients as having a true versus pseudo-C-TAT.
Footnotes
Authors’ Note: This case was presented in part and in abstract form at the Scientific Sessions of the American College of Cardiology in New Orleans, Louisiana, March 12, 2019.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: Our institution does not require ethical approval for reporting individual cases or case series.
Informed Consent: Verbal informed consent was obtained from the patient for his anonymized information to be published in this article.
References
- 1. Raheja H, Namana V, Moskovits N, Hollander G, Shani J. Cor triatriatum sinistrum. Arq Bras Cardiol. 2018; 110:101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Joseph I, Jester G, Lo MC. Cor triatriatum as an uncommon cause of recurrent syncope. J Gen Intern Med. 2018;33:1201-1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rudienė V, Hjortshøj CMS, Glaveckaitė S, et al. Cor triatriatum sinistrum diagnosed in the adulthood: a systematic review. Heart. 2019;105:1197-1202. [DOI] [PubMed] [Google Scholar]
- 4. Fuchs MM, Connolly HM, Said SM, Egbe AC. Outcomes in patients with cor triatriatum sinister. Congenit Heart Dis. 2018;13:628-632. [DOI] [PubMed] [Google Scholar]
- 5. Naimo PS, Konstantinov IE. Cor triatriatum sinister: is it less sinister in older patients? J Thorac Cardiovasc Surg. 2015;150:e77-e78. [DOI] [PubMed] [Google Scholar]