Abstract
In recent years, nontraditional mental healthcare services and tools (e.g., mobile apps, peer counselors, online support groups) have been developed to increase access to and utilization of behavioral health services. This study investigates how adolescents and younger adults use and perceive various nontraditional mental healthcare services in comparison to traditional services and in comparison to each other. A questionnaire-based study was conducted that included 203 participants between the ages of 17 and 37 (M = 25.01, SD = 5.04). Results showed that while usage rates of nontraditional mental health services were considerably high, the highest rates were reported for traditional services. Similarly, participants reported high levels of willingness to use nontraditional services, yet the highest levels of willingness were reported for traditional services. These findings suggest that the integration of nontraditional services with traditional services may be particularly impactful for young people.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11414-020-09746-w.
Introduction
Adolescents and younger adults navigate a crucial developmental period marked by rapid biological and social changes. Almost half of all mental disorders begin in adolescence.1 Today’s adolescents and younger adults report increasingly high levels of depressive symptoms, stress, and loneliness as compared to adolescents and younger adults in older cohorts.2, 3 There are multiple possible explanations for these concerns. First, this trend may be a result of the mentally and emotionally straining aspects of modern culture, including the increased use of technology and a more sedentary lifestyle.4 Second, the reduction in stigma associated with having a mental health condition and/or seeking mental healthcare that has occurred in recent decades may have led to more understanding and identification of mental health needs overall.5 Third, while today’s adolescents and younger adults are navigating a crucial developmental period, they are concurrently responding to the stressors of an economic recession and a global pandemic.6 A combination of developmental changes, high levels of depressive symptomology, and unique stressors related to the current events of the world suggest that this population may have different mental health needs compared to other age groups.
Despite the increasing number of people in need of services, the US Department of Health and Human Services estimates that there is a shortage of mental healthcare providers—something which will only progress in the upcoming years.7 Subsequently, researchers have called for the development and uptake of nontraditional mental health services. Projections from nearly a decade ago noted that the traditional model of delivering services (i.e., one-on-one sessions with a mental health provider) could not possibly keep up with the demand for care.8 In response to this gap in care, many nontraditional services and tools have been introduced in recent years to either support or replace traditional care. The most common include mobile applications (“apps”), online support communities, self-help books, and peer counseling.9–12
While these services and tools have been widely studied for their efficacy, there is a lack of research investigating how adolescents and younger adults perceive them: (1) in comparison to traditional mental health services or (2) in comparison to each other. In previous research, young adults (ages 18–25) reported a preference to speak to their general practitioner or doctor about mental health concerns rather than mental health professionals.13 Similarly aged cohorts also endorsed a preference for speaking to mental health professionals over using digital mental health tools when seeking mental health–related information and treatment for mental health difficulties.14, 15 Beyond these noted preferences, there is a need to investigate how this population feels about nontraditional mental health services and tools.
Furthermore, there is limited research in the mental health field on the differences between Millennials (born between 1981 and 1996) and Generation Z’s (born between 1997 and 2012), although the topic is gaining more interest.16, 17 While Millennials adopted a widespread technology, such as mobile apps and online social media in their adolescence and adulthood, Generation Z’s have been familiar with these technologies since childhood.18 Compared to Millennials, Generation Z’s spend more time using electronic communication and less time engaging in face-to-face interactions.17 These generational differences could have implications regarding healthcare service utilization, with Generation Z’s potentially being more willing than Millennials to use digital tools over face-to-face services.
This study was designed to fill in the gaps in the literature by examining the mental healthcare preferences of adolescents and younger adults (i.e., Millennials and Generation Z’s). There were three main goals: (1) determine how willing adolescents and younger adults are to use nontraditional services or tools, (2) determine what barriers may be keeping them from using nontraditional services or tools, and (3) identify any major differences between the preferences of Millennials and Generations Z’s.
Methods
Participants
This study used data from a survey conducted in Chicago during November and December of 2019. A total of 203 participants between the ages of 17 and 37 (M = 25.01, SD = 5.04) who were fluent in English participated in the survey. For the purposes of this study, adults up to age 37 were included to fully represent the Millennial generation (born between 1981 and 1996). The subset of individuals between ages 18 and 37 is referred to as “younger adults” so as to distinguish them from adults in older generations (e.g., Generation X and Baby Boomers) and what is typically defined as a young adult cohort (i.e., 18–25 years of age).
Participants were recruited using convenience sampling strategies. Recruitment took place through print advertisements posted in community areas, posts on online community boards (i.e., Craigslist and Reddit), mass emails on ResearchMatch, and through direct contact with local college and university student organizations. All study procedures were approved by the Northwestern University Institutional Review Board (IRB) before enrolling participants, and all participants provided informed consent.
Survey
Participants were asked to complete a survey that was designed by study staff at Northwestern University. The survey asked all participants questions regarding demographics, perceived accessibility and reliability of services/tools, self-reported willingness to use services/tools, and comparative rankings of services/tools. Participants aged 18 and older were asked about their mental health history. Due to IRB concerns about the reliability of information from participants under the age of 18, that subset of participants was not asked questions regarding their mental health status. However, participants that were under the age of 18 and willing to provide data outside of mental health status were still included in the present analyses so as to gather as much information about the preferences of individuals from Generation Z. These participants answered all questions in the survey besides those inquiring about mental health history.
The mental healthcare services/tools examined included mental health professionals (e.g., psychiatrists, psychologists, and licensed counselors), primary care providers (e.g., medical doctors, nurse practitioners, and physician assistants), self-help books, mobile apps, online support communities (e.g., Tumblr, Reddit), and peer counselors. Participants were provided with a detailed description of each service/tool included in the survey (e.g., “Peer counselors are individuals without a formalized degree or certification who offer support for mental health concerns by providing active listening and problem-solving services”) prior to their completion of the survey.
Perceived accessibility and reliability of services/tools
Participants indicated how accessible they believed each mental health service/tool to be on a 5-point Likert scale (i.e., 1 = very accessible to 5 = very inaccessible; see Supplementary Materials for full item list). Participants indicated how much they agreed with statements regarding barriers to care for each mental health service/tool (e.g., “Cost of care keeps me from talking to my primary care provider about stress or mental health”) on a 5-point Likert scale (i.e., 1 = strongly agree to 5 = strongly disagree). To represent both attitudinal and structural barriers to care, three main barriers were assessed: cost, time constraints, and fear of judgment. These barriers are among the most commonly reported by individuals as impeding their ability to receive traditional care.19 Participants indicated how reliable they believed information about stress or mental health is coming from each mental health service/tool on a 5-point Likert scale (i.e., 1 = very reliable to 5 = very unreliable).
Self-reported willingness to use services/tools
For each mental health service/tool, participants indicated how much they agreed with statements regarding their willingness to use the service/tool for mental health concerns (e.g., “If I had a mental health condition, I would be willing to talk to a peer counselor about it”) on a 5-point Likert scale (i.e., 1 = strongly agree to 5 = strongly disagree).
Comparative rankings of services/tools
Participants ranked which of the services/tools they would most prefer to use to manage mental health conditions on a 6-point Likert scale (e.g., 1 = most preferred to 6 = least preferred).
Data analysis
Descriptive statistics were used to characterize the study sample and to report participants’ current use of nontraditional services/tools, their reported willingness to use each service/tool, and their rankings for which services/tools they preferred most. For each mental health service/tool, Kendall’s Tau correlation analyses were used to test the strength of the relationship between reported willingness to use the service/tool and the following five variables: perceived accessibility, perceived reliability, perceived time barrier, perceived cost barrier, and perceived stigma barrier. Kendall’s Tau was used due to (1) the Likert-type questions producing ordinal data 20 and (2) its ability to handle ties.21 Wilcoxon-Mann-Whitney tests were conducted to determine if there were significant differences in reported willingness to use services/tools, perceived reliability of services/tools, or perceived barriers between Millennials and Generation Z’s. Participants were divided into generations based on their date of birth. As such, participants born between 1981 and 1996 were considered Millennials, while participants born during or after 1997 were considered Generation Z’s.18 Wilcoxon-Mann-Whitney tests were also conducted to determine if there were significant differences in reported willingness to use services/tools, perceived reliability of services/tools, or perceived barriers between participants who indicated they had at least one diagnosed mental health condition and participants who indicated they did not have any mental health conditions.
Results
Participant characteristics
Participants included 203 adolescents and younger adults between the ages of 17 and 37 (M = 25.01, SD = 5.04). The majority of participants indicated they were assigned “female” at birth (76.35%). One participant indicated they were assigned “intersex” at birth (0.49%), and the rest indicated they were assigned “male” (23.15%). The majority of participants identified their gender as either “female” (70.94%) or “male” (23.15%). The sample was predominantly white (79.8%) and non-Hispanic (90.64%). Participants over the age of 18 (n = 198) were asked to report whether or not they had a mental health condition. Therefore, mental health data was not assessed for five participants who were 17 at the time of the data collection. About half (52.53%) of participants over the age of 18 indicated that they had a mental health condition. Of those participants (n = 104), the most commonly reported condition was generalized anxiety disorder (GAD; 36.45%), followed by major depressive disorder (MDD; 23.15%).
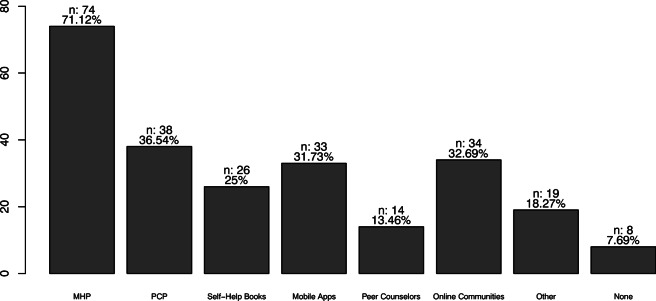
Current treatment methods
Participants who indicated that they did have a mental health condition (n = 104) were asked about current treatment methods. Most participants (82.73%) indicated using multiple methods within the past 6 months to treat and/or manage their mental health (see Fig. 1 for care method frequencies). The most commonly reported method was working with a mental health professional (71.12%). Nearly one-third of participants indicated engaging with mobile apps (31.73%) and online communities (32.69%) to treat and/or manage their condition. “Other” methods included breathing exercises, medication, journaling, and listening to mental health podcasts. A small minority (7.69%) reported not using any methods to manage and/or treat their condition.
Figure 1.
Methods used within the last 6 months to treat and/or manage mental health conditions. PCP primary care providers, MHP mental health professionals
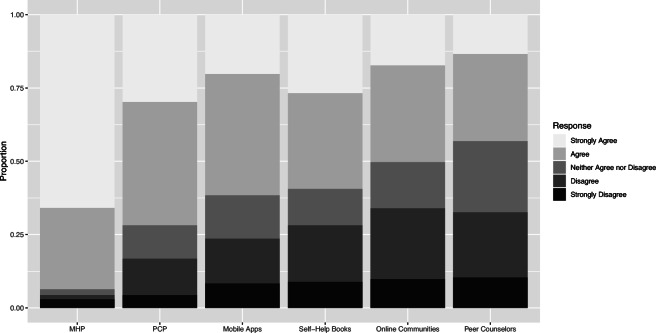
Willingness to use services
With the exception of peer-counseling, the majority of participants indicated willingness to use nontraditional services to treat and/or manage mental health conditions. The highest levels of willingness were reported for traditional services (i.e., working with a mental health professional), with 93.5% of participants having either agreed or strongly agreed that they would be willing to work with a mental health professional. Following mental health professionals, 71.8% of participants indicated they were willing to work with their primary care provider, 61.6% indicated that they were willing to use apps, 59.4% indicated that they were willing to use self-help books, 50.2% indicated that they were willing to use online communities, and 43.1% indicated they were willing to work with peer counselors (see Table 1 and Fig. 2).
Table 1.
Willingness to use services/tools
| PCPa (%) | MHPb (%) | Books (%) | Apps (%) | Onlinec (%) | Peerd (%) | |
|---|---|---|---|---|---|---|
| Strongly Agree | 29.7 | 65.8 | 26.7 | 20.2 | 17.2 | 13.4 |
| Agree | 42.1 | 27.7 | 32.7 | 41.4 | 33.0 | 29.7 |
| Neither | 11.4 | 2.0 | 12.4 | 14.8 | 15.8 | 24.3 |
| Disagree | 12.4 | 1.5 | 19.3 | 15.3 | 24.1 | 22.3 |
| Strongly Disagree | 4.5 | 3.0 | 8.9 | 8.4 | 9.9 | 10.4 |
aPrimary care providers
bMental health professionals
cOnline communities
dPeer counselors
Figure 2.
Willingness to use services/tools
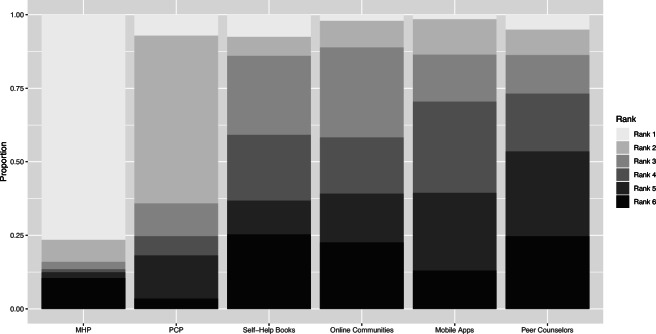
Participants’ rankings for which services they would most prefer to use to manage mental health conditions also showed a preference for mental health professionals (76.5% indicated that it was their first choice). The most popular second choice was working with a primary care provider (see Table 2 and Fig. 3).
Table 2.
Rankings for preferred services/tools
| PCP (%) | MHP (%) | Books (%) | Apps (%) | Online (%) | Peer (%) | |
|---|---|---|---|---|---|---|
| 1 | 7.1 | 76.5 | 7.5 | 1.5 | 5.1 | 2.0 |
| 2 | 57.1 | 7.5 | 6.5 | 12.0 | 8.6 | 9.0 |
| 3 | 11.1 | 2.5 | 26.9 | 16.0 | 13.1 | 30.7 |
| 4 | 6.6 | 1.0 | 22.4 | 31.0 | 19.7 | 19.1 |
| 5 | 14.6 | 2.0 | 11.4 | 26.5 | 28.8 | 16.6 |
| 6 | 3.5 | 10.5 | 25.4 | 13.0 | 24.7 | 22.6 |
Figure 3.
Rankings for preferred services/tools
Relationships between willingness to use services and perceived barriers
For each service, results showed a significant positive correlation between the perceived accessibility of the service and willingness to use the service (p’s < 0.01). Additionally, for each service, results showed a significant positive correlation between the perceived reliability of the service and willingness to use it (p’s < 0.001; see Table 3). Correlations were generally weak (r’s < 0.5), but stronger correlations were identified for (1) perceived reliability and willingness to use self-help books (r = 0.41, p < 0.001) and 2) perceived reliability and willingness to use online communities (r = 0.41, p < 0.001).
Table 3.
Correlations
| Service/tool | Correlation | Result |
|---|---|---|
| Primary care providers | Accessibility and willingness | r = 0.31, p < 0.05*** |
| Reliability and willingness | r = 0.29, p < 0.05*** | |
| Cost and willingness | r = − 0.09, p > 0.05 | |
| Time and willingness | r = 0.06, p > 0.05 | |
| Stigma and willingness | r = − 0.35, p < 0.05*** | |
| Mental health professionals | Accessibility and willingness | r = 0.18, p < 0.05** |
| Reliability and willingness | r = 0.29, p < 0.05*** | |
| Cost and willingness | r = − 0.17, p < 0.05** | |
| Time and willingness | r = − 0.03, p > 0.05 | |
| Stigma and willingness | r = − 0.41, p < 0.05*** | |
| Self-help books | Accessibility and willingness | r = 0.29, p < 0.05*** |
| Reliability and willingness | r = 0.41, p < 0.05*** | |
| Cost and willingness | r = 0.09, p > 0.05 | |
| Time and willingness | r = 0.15, p < 0.05* | |
| Stigma and willingness | r = − 0.03, p > 0.05 | |
| Online communities | Accessibility and willingness | r = 0.29, p < 0.05*** |
| Reliability and willingness | r = 0.41, p < 0.05*** | |
| Cost and willingness | r = − 0.002, p > 0.05 | |
| Time and willingness | r = 0.05, p > 0.05 | |
| Stigma and willingness | r = − 0.03, p > 0.05 | |
| Mobile apps | Accessibility and willingness | r = 0.26, p < 0.05*** |
| Reliability and willingness | r = 0.28, p < 0.05*** | |
| Cost and willingness | r = 0.10, p > 0.05 | |
| Time and willingness | r = 0.12, p < 0.05* | |
| Stigma and willingness | r = − 0.14, p < 0.05* | |
| Peer counselors | Accessibility and willingness | r = 0.28, p < 0.05*** |
| Reliability and willingness | r = 0.31, p < 0.05*** | |
| Cost and willingness | r = 0.08, p > 0.05 | |
| Time and willingness | r = 0.13, p < 0.05* | |
| Stigma and willingness | r=−0.21, p<0.05*** |
*p < 0.05
**p < 0.01
***p < 0.001
Results showed significant negative correlations between perceived stigma and willingness to use the service for primary care providers (r = − 0.35, p < 0.001), mental health professionals (r = − 0.41, p < 0.001), mobile apps (r = − 0.14, p < 0.05), and peer counselors (r = − 0.21, p < 0.001). A significant negative correlation was also identified for perceived cost and willingness to see a mental health professional (r = − 0.17, p < 0.01). A perceived time barrier was found to positively correlate with willingness to use self-help books (r = 0.15, p < 0.05), mobile apps (r = 0.12, p < 0.05), and peer counselors (r = 0.13, p < 0.05; Table 3).
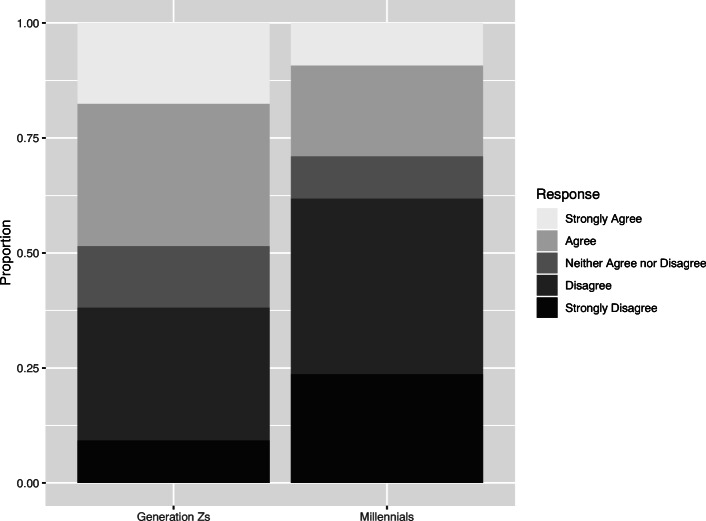
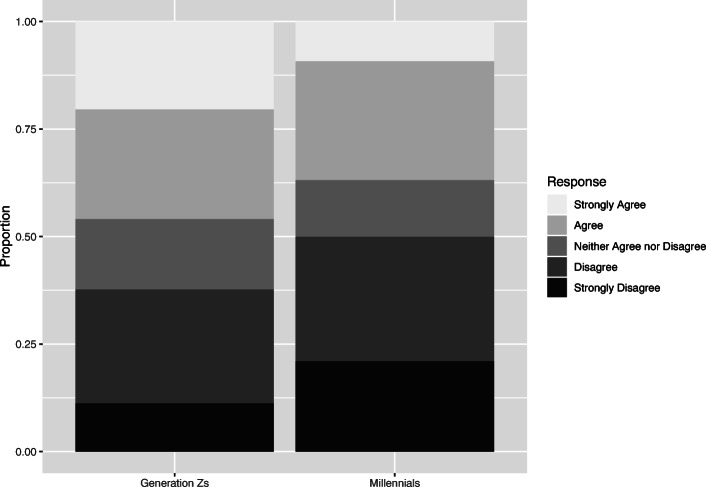
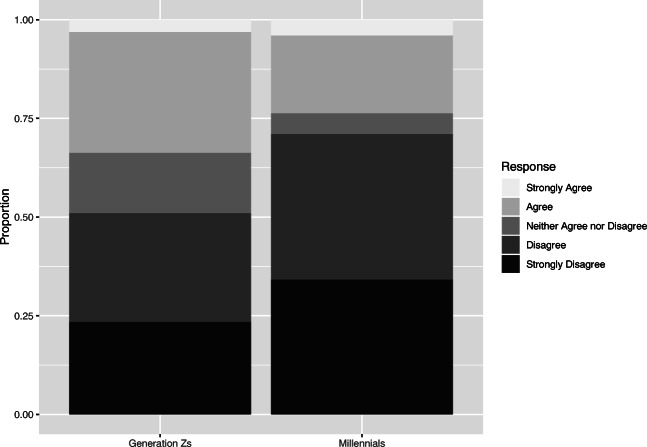
Differences between generations
Participants were divided into generations based on age. Ninety-eight participants were categorized as “Generation Z’s” (mean age = 21.38, SD = 1.59), 76 participants were categorized as “Millennial” (mean age = 29.71, SD = 3.97), and 30 participants were excluded from these analyses because of missing data on age. Wilcoxon-Mann-Whitney analyses revealed a significant difference between Millennials and Generation Z’s in perceived stigma as a barrier to working with primary care providers (W = 4725, p < 0.05, r = 0.25), using peer counselors (W = 4390.5, p < 0.05, r = 0.16), and using online communities (W = 4407.5, p < 0.05, r = 0.16). For all significant differences, Millennials were less likely to identify stigma as a barrier than Generation Z’s (p’s < 0.05; Figs. 4, 5, and 6). There was no evidence to suggest additional differences between Millennials and Generation Z’s.
Figure 4.
Perceived stigma as a barrier to using primary care providers: differences between Generation Z’s and Millennials
Figure 5.
Perceived stigma as a barrier to using peer counselors: differences between Generation Z’s and Millennials
Figure 6.
Perceived stigma as a barrier to using online communities: differences between Generation Z’s and Millennials
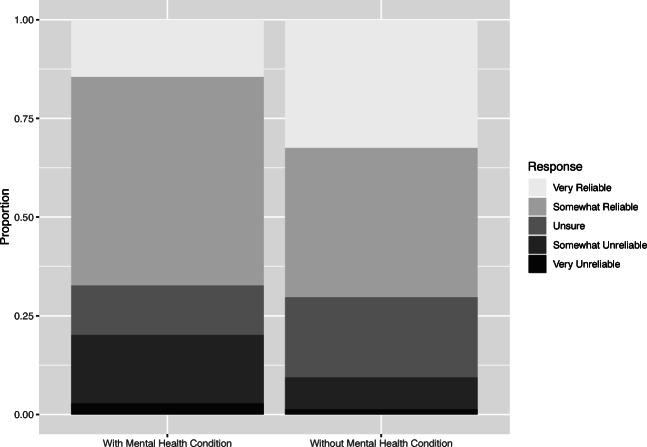
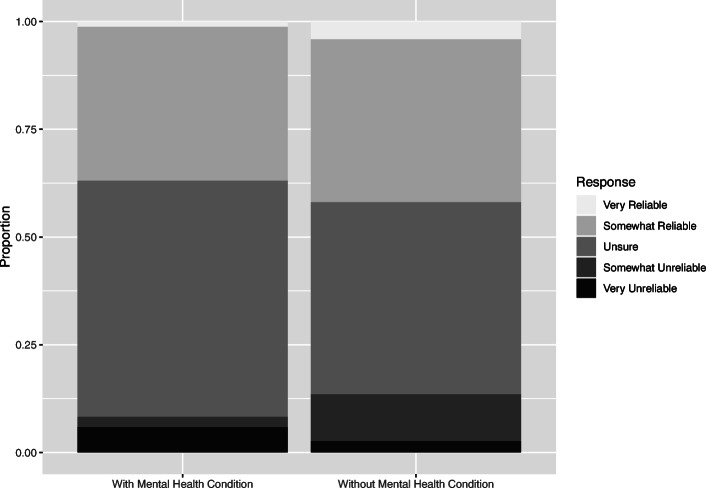
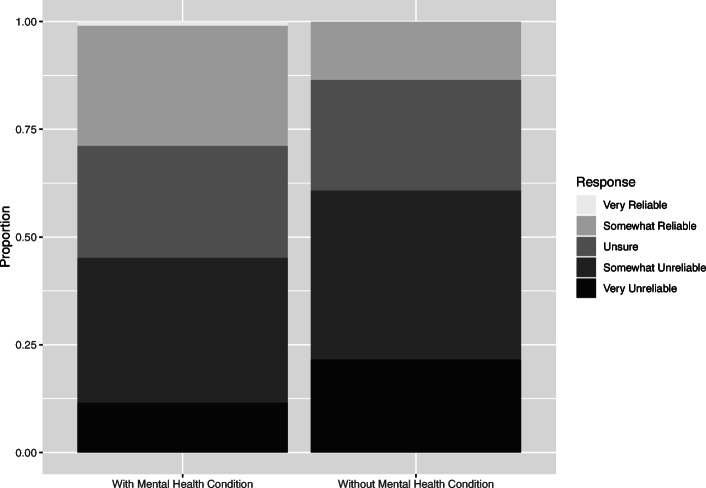
Differences between participants with and without a self-disclosed mental health condition
Participants who were 18 years or older were asked to self-disclose whether or not they had a diagnosed mental health condition. One hundred and four participants indicated that they did have a mental health condition. Wilcoxon-Mann-Whitney analyses revealed significant differences between participants with and without a mental health condition in perceived reliability of primary care providers (W = 4524, p < 0.05, r = 0.16), peer counselors (W = 4557.5, p < 0.05, r = 0.17), and online communities (W = 2986, p < 0.01, r = 0.19). Participants with a mental health condition were less likely to rate primary care providers and peer counselors as reliable (p’s < 0.05; Figs. 7 and 8). However, participants with a mental health condition were more likely to rate online communities as reliable (p < 0.01; Fig. 9). There was no evidence to suggest additional differences between participants with and without a mental health condition.
Figure 7.
Perceived reliability of primary care providers: differences between participants with and without a mental health condition
Figure 8.
Perceived reliability of peer counselors: differences between participants with and without a mental health condition
Figure 9.
Perceived reliability of online communities: differences between participants with and without a mental health condition
Discussion
There is an increasing need to look for cost-effective and scalable services outside of traditional face-to-face mental health services. Indeed, serious psychological distress increased 71% among young adults between 2008 and 2017 and rates of major depressive episodes increased 63% among young adults between 2009 and 2017.3 To the authors’ knowledge, this study is the first to examine how adolescents and younger adults perceive multiple types of nontraditional services, in comparison to traditional services and in comparison to each other. It is also the first study to examine what differences might exist between the nontraditional care preferences of Millennials (born between 1981 and 1996) and Generation Z’s (born between 1997 and 2012).
The present findings indicate that the majority of participants are willing to use nontraditional services (with the exception of peer counseling) to treat and/or manage mental health conditions, but that traditional mental health services are preferred as a first-choice treatment. This is consistent with a previous work indicating a preference for traditional services.14, 15, 22 At the same time, most participants with a mental health condition indicated using multiple methods to treat and/or manage their condition. These results add to a growing body of literature suggesting that young people are not interested in nontraditional services as a replacement for traditional services, but as a supplement or enhancement to care.23, 24
Results showed high rates of willingness to speak with a primary care provider about mental health, potentially supporting the use of collaborative care models to connect individuals in need with both traditional and nontraditional services.25 Results showed lower rates of willingness to use peer counseling services than other services or tools. This could be in part due to the perceived stigma associated with disclosing mental health information to a peer. The results did indicate a significant relationship between perceived stigma and willingness to use peer counselors, but the effect size was weak. Alternatively, while there are multiple types of peer counseling and peer specialist services available in various settings, it could be possible that participants were not previously exposed to peer counseling and not familiar with it. Only 13.46% of participants with a mental health condition indicated using peer counselors within the past 6 months. Furthermore, nearly one-fourth of participants answered “neither agree nor disagree” when asked about peer counselors, possibly indicating a lack of knowledge.
When peer counseling was first developed and studied, it was primarily within university and K-12 settings, suggesting that individuals not enrolled in school would not be likely to access peer counselors.26–28 In recent years, however, peer counseling and peer specialist services have expanded to other settings including inpatient, outpatient, and online settings.12, 29, 30 While peer counseling may not be as widely accessible or familiar to individuals in younger generations as traditional services, there is evidence to suggest that peer counselors are likely to become more widely available in the next few years, particularly as mental healthcare provider shortages increase.31 In populations which are exposed to peer counselors, acceptability is generally high, suggesting that willingness could increase as individuals in younger generations become more exposed.32 Future research may examine how usage and perception of peer counselors in younger generations changes as services become more available.
Accessibility was expected to impact participants’ perceptions of services. For this reason, it is not surprising that perceived accessibility positively correlated with willingness to use each evaluated service. This finding supports the literature surrounding perceived accessibility as a facilitator to treatment.33, 34 Previous research has found stigma to be a barrier to mental health treatment for young people.35 Results showed negative correlations between perceived stigma and willingness for multiple services, but there was a particularly strong correlation for mental health professionals. This could confirm the hypothesis that nontraditional services serve to minimize the stigma around mental health treatment.14, 22
Perceived reliability was associated with willingness to engage with each service; this effect was strong for self-help books and online communities. Concerns over the reliability of the information presented in both self-help books and online communities have previously been voiced.36, 37 The current findings suggest that participants may be aware of these concerns and take them into consideration when determining their willingness to use these tools. Results also indicated significant differences between participants with a mental health condition and participants without a mental health condition in perceived reliability of primary care providers, peer counselors, and online communities. Participants with a mental health condition were less likely to rate primary care providers and peer counselors as reliable, but more likely to rate online communities as reliable.
It is possible that participants may expect information about mental health coming from online communities to be more realistic or unembellished, while information from peer counselors or primary care providers is framed to serve a specific clinical purpose. Previous research suggests that online communities are perceived as helpful for finding information from others with first-hand experience with health problems.38 In an ideal model, peer counselors have first-hand experience with mental health concerns, giving them credibility over the subject matter and a sense of connection to others with a mental health condition.39 However, peer counselors still generally operate in a professional capacity, which could alienate them from clients. It is also possible that the participants in this sample with mental health conditions had previous negative experiences discussing mental health concerns with primary care providers or peer counselors, which could have impacted their reported perceptions. For each of these findings, effect sizes were relatively small. Future work should attempt to determine if these findings are consistent across multiple studies.
There were surprisingly few differences between Millennials and Generation Z’s. The differences that did emerge were related to perceived stigma, with Generation Z’s being more likely to identify perceived stigma as a barrier than Millennials. This contrasts with the suggestion that mental health stigma is decreased in Generation Z, compared to other generations.40 It is worth noting, however, that the effect sizes were relatively small. Another potential explanation could be that perceived stigma is more directly related to age or education level (e.g., older generations may have completed their education, whereas Generation Z may still be enrolled as students) than to generational differences. Future research should investigate the interplay between generational status and mental health stigma as a barrier to treatment.
Limitations and future directions
This study had several limitations. First, the current sample appears to be more representative of a help-seeking population rather than a general population of adolescents and younger adults. Approximately half of the participants reported a mental health condition; this rate is nearly double the reported rate of young adults with any mental illness in a national sample.41 It is possible that the participants were more familiar with mental health services than the general population, and expressed a greater willingness to use services as a result. On the other hand, previous research has shown that individuals with a history of a mental health referral are more reliant on avoidant coping strategies such as “distraction” and more self-stigmatizing than those without a history of mental health referral.42 This raises the potential that the current participants were less open to receiving support than the general population. Future research using a more normative sample of both healthy individuals and individuals with an identified mental health condition is needed. Of the conditions reported by participants, major depressive disorder and generalized anxiety disorder were the most common. Another area for future research may be in targeting individuals with serious mental illnesses (e.g., psychosis) to determine if perceptions of nontraditional and traditional services differ from those reported in this study.
Second, many participants were recruited through online registries, such as ResearchMatch, and online communities, such as Reddit. As a result, these findings may be less representative of individuals with low familiarity with digital technology.
Third, there was a small number of participants under the age of 18 (n = 5). Data from incomplete surveys indicated that approximately 40 participants under the age of 18 began the survey, but exited once it requested parental contact information. Future research may benefit from requesting a waiver of parental consent when assessing the treatment preferences of adolescents.
Fourth, the sample was predominantly white and female-identifying. The recruitment methods for this study relied heavily on online recruitment, which have been documented in previous studies as leading to overrepresentation of white and female-identifying populations.43, 44 Furthermore, common mental health problems, such as depression, are diagnosed at nearly twice the rate in women compared to men.45 This study’s findings should be interpreted in light of these concerns. Future investigations can more accurately represent the full population by recruiting a more racially diverse sample and by recruiting more males. Potential strategies include using a stratified recruitment technique, targeting online ads to regions with a higher proportion of minority groups, or partnering with community-based organizations.46 Additionally, a more diverse sample could allow for investigations regarding potential cultural differences in nontraditional service preferences.
Fifth, there was missing information regarding date of birth for several participants, which made detecting differences based on generation more difficult. Sixth, while the survey assessed participants’ self-reported barriers to receiving mental health services, it did not collect data on participants’ insurance status or geographical location, two commonly reported barriers to traditional mental health services.19 Future work may focus on identifying whether a lack of medical insurance or lack of nearby services plays a role in participants’ interest in nontraditional mental health tools.
Lastly, the data included in this study were collected prior to the COVID-19 pandemic and the associated physical distancing and public health measures in the USA. The extent of the pandemic’s impact on young people’s mental health is not yet fully known, but preliminary evidence suggests that the pandemic has resulted in increased stress, anxiety, and depression.47 It can be expected that mental healthcare will be in even higher demand as a result.48 Nontraditional services such as those investigated in the current study could serve to overcome the barriers associated with face-to-face service delivery. It is possible that usage and acceptability of nontraditional services has increased due to the necessity of finding alternatives to traditional care. Future research should investigate how usage and preferences of traditional and nontraditional services have changed since the onset of the pandemic.
Implications for Behavioral Health
Nontraditional services and tools have the potential to improve access to mental healthcare and may be particularly helpful for adolescents and younger adults who are at high risk for developing a mental health condition. The current findings indicate that many young people are willing to use nontraditional services and that these nontraditional services could be used to supplement traditional care. There are multiple methods by which nontraditional and traditional services could be integrated. First, stepped-care models could be implemented to deliver less resource–intensive nontraditional tools to individuals with mild symptoms before advancing to traditional services.49 For example, recent literature suggests self-help workbooks and Internet-based interventions may be effective as early steps in a stepped-care approach.50, 51
Second, nontraditional services and tools could be delivered during periods in which clients are “waiting,” taking advantage of clients’ availability and interest in services. In one study, a mental health app was administered to college students while they were on a waitlist to receive counseling services and was found to be acceptable.52 In another study, researchers used the 2 hours after a slow-release injection medication administration to deliver a peer-led intervention, taking advantage of the “dead time” when patients usually sat in the clinic.53
Lastly, nontraditional and traditional services can be delivered concurrently, with nontraditional tools or services serving to reinforce content, track mood fluctuations, or provide extra support.54, 55 Peer support services, for example, may serve to provide community connection and reinforce content learning alongside traditional treatment.39 The proliferation of peer specialists in a variety of clinical and community contexts over the last several years demonstrates the potential for integrating nontraditional services in a broader system of care.29, 30, 39, 53, 55 Continued research is needed to explore the potential in integrating nontraditional services with traditional services, particularly as rates of mental health concerns continue to rise.
Supplementary Information
(DOCX 19 kb)
Funding
REDCap is supported at FSM by the Northwestern University Clinical and Translational Science (NUCATS) Institute. Research reported in this publication was supported, in part, by the National Institutes of Health’s National Center for Advancing Translational Sciences, Grant Number UL1TR001422. Emily G. Lattie is supported by a grant from the National Institute of Mental Health (K08 MH112878). Colleen Stiles-Shields is supported by a fellowship from the Cohn Family Foundation.
Compliance with Ethical Standards
Conflict of Interest
Emily G. Lattie is supported by a grant from the National Institute of Mental Health (K08 MH112878). Colleen Stiles-Shields is supported by a fellowship from the Cohn Family Foundation.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health in publications relating to this project.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Jones PB. Adult mental health disorders and their age of onset. The British Journal of Psychiatry. 2013;202(54):4–10. doi: 10.1192/bjp.bp.112.119164. [DOI] [PubMed] [Google Scholar]
- 2.Twenge JM. Time Period and Birth Cohort Differences in Depressive Symptoms in the U.S., 1982–2013. Social Indicators Research. 2015;121(2):437–454. doi: 10.1007/s11205-014-0647-1. [DOI] [Google Scholar]
- 3.Twenge JM, Cooper AB, Joiner TE, et al. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005-2017. Journal of Abnormal Psychology. 2019;128(3):185–199. doi: 10.1037/abn0000410. [DOI] [PubMed] [Google Scholar]
- 4.Hoare E, Milton K, Foster C, et al. The associations between sedentary behaviour and mental health among adolescents: a systematic review. International Journal of Behavioral Nutrition and Physical Activity. 2016;13(1):108. doi: 10.1186/s12966-016-0432-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Segal DL, Coolidge FL, Mincic MS, et al. Beliefs about mental illness and willingness to seek help: A cross-sectional study. Aging & Mental Health. 2005;9(4):363–367. doi: 10.1080/13607860500131047. [DOI] [PubMed] [Google Scholar]
- 6.Odgers C, Robb MB. Tweens, teens, tech, and mental health: Coming of age in an increasingly digital, uncertain, and unequal world, 2020. San Francisco, CA: Common Sense Media; 2020. [Google Scholar]
- 7.Health Resources and Services Administration . National Projections of Supply and Demand for Behavioral Health Practitioners: 2013-2025. National Center for Health Workforce Analysis: Rockville; 2015. [Google Scholar]
- 8.Kazdin AE, Rabbitt SM. Novel models for delivering mental health services and reducing the burdens of mental illness. Clinical Psychological Science. 2013;1(2):170–191. doi: 10.1177/2167702612463566. [DOI] [Google Scholar]
- 9.Mohr DC, Tomasino KN, Lattie EG, et al. IntelliCare: An Eclectic, Skills-Based App Suite for the Treatment of Depression and Anxiety. Journal of Medical Internet Research. 2017;19(1):e10. doi: 10.2196/jmir.6645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lal S, Nguyen V, Theriault J. Seeking mental health information and support online: experiences and perspectives of young people receiving treatment for first-episode psychosis. Early Intervention in Psychiatry. 2018;12(3):324–330. doi: 10.1111/eip.12317. [DOI] [PubMed] [Google Scholar]
- 11.Hanson K. Positive Psychology for Overcoming Symptoms of Depression: A Pilot Study Exploring the Efficacy of a Positive Psychology Self-Help Book versus a CBT Self-Help Book. Behavioural and Cognitive Psychotherapy. 2019;47(1):95–113. doi: 10.1017/S1352465818000218. [DOI] [PubMed] [Google Scholar]
- 12.Bernecker SL, Banschback K, Santorelli GD, et al. A Web-Disseminated Self-Help and Peer Support Program Could Fill Gaps in Mental Health Care: Lessons From a Consumer Survey. JMIR Mental Health. 2017;4(1):e5. doi: 10.2196/mental.4751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hickie IB, Luscombe GM, Davenport TA, et al. Perspectives of young people on depression: awareness, experiences, attitudes and treatment preferences. Early Intervention in Psychiatry. 2007;1(4):333–339. doi: 10.1111/j.1751-7893.2007.00042.x. [DOI] [PubMed] [Google Scholar]
- 14.Horgan A, Sweeney J. Young students’ use of the Internet for mental health information and support. Journal of Psychiatric and Mental Health Nursing. 2010;17(2):117–123. doi: 10.1111/j.1365-2850.2009.01497.x. [DOI] [PubMed] [Google Scholar]
- 15.March S, Day J, Ritchie G, et al. Attitudes Toward e-Mental Health Services in a Community Sample of Adults: Online Survey. Journal of Medical Internet Research. 2018;20(2):e59. doi: 10.2196/jmir.9109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Curtis BL, Ashford RD, Magnuson KI, et al. Comparison of Smartphone Ownership, Social Media Use, and Willingness to Use Digital Interventions Between Generation Z and Millennials in the Treatment of Substance Use: Cross-Sectional Questionnaire Study. Journal of Medical Internet Research. 2019;21(4):e13050. doi: 10.2196/13050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Twenge JM, Spitzberg BH, Campbell WK. Less in-person social interaction with peers among U.S. adolescents in the 21st century and links to loneliness. Journal of Social and Personal Relationships. 2019;36(6):1892–1913. doi: 10.1177/0265407519836170. [DOI] [Google Scholar]
- 18.Dimock M. Defining generations: Where Millennials end and Generation Z begins. Pew Research Center. Available online at https://www.pewresearch.org/fact-tank/2019/01/17/where-millennials-end-and-generation-z-begins/. Accessed on January 17, 2020.
- 19.Kazdin AE. Addressing the treatment gap: A key challenge for extending evidence-based psychosocial interventions. Behaviour Research and Therapy. 2017;88:7–18. doi: 10.1016/j.brat.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 20.Jamieson S. Likert scales: how to (ab)use them. Medical Education. 2004;38(12):1217–1218. doi: 10.1111/j.1365-2929.2004.02012.x. [DOI] [PubMed] [Google Scholar]
- 21.Field A, Miles J, Field Z. Discovering Statistics Using R. Thousand Oaks, CA: SAGE Publications; 2012. [Google Scholar]
- 22.Bradford S, Rickwood D. Adolescent’s preferred modes of delivery for mental health services. Child and Adolescent Mental Health. 2014;19(1):39–45. doi: 10.1111/camh.12002. [DOI] [PubMed] [Google Scholar]
- 23.Lungu A, Sun M. Time for a Change: College Students’ Preference for Technology-Mediated Versus Face-to-Face Help for Emotional Distress. Telemedicine and E-Health. 2016;22(12):991–1000. doi: 10.1089/tmj.2015.0214. [DOI] [PubMed] [Google Scholar]
- 24.Younes N, Chollet A, Menard E, et al. E-mental health care among young adults and help-seeking behaviors: a transversal study in a community sample. Journal of Medical Internet Research. 2015;17(5):e123. doi: 10.2196/jmir.4254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lake J, Turner MS. Urgent Need for Improved Mental Health Care and a More Collaborative Model of Care. The Permanente Journal. 2017;21:17–24. doi: 10.7812/TPP/17-024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dooley D. Assessing nonprofessional mental health workers with the GAIT. An evaluation of peer ratings. American Journal of Community Psychology. 1975;3(2):99–110. doi: 10.1007/BF00877785. [DOI] [PubMed] [Google Scholar]
- 27.Hamburg BA, Varenhorst BB. Peer counseling in the secondary schools: a community mental health project for youth. American Journal of Orthopsychiatry. 1972;42(4):566–581. doi: 10.1111/j.1939-0025.1972.tb02523.x. [DOI] [PubMed] [Google Scholar]
- 28.Jones F, Najera GA. The helping network: reactions and actions stimulated by students’ acute mental illness in a university community. Journal of American College Health Association. 1976;24(4):198–202. [PubMed] [Google Scholar]
- 29.Kumar A, Azevedo KJ, Factor A, et al. Peer support in an outpatient program for veterans with posttraumatic stress disorder: Translating participant experiences into a recovery model. Psychological Services. 2019;16(3):415–424. doi: 10.1037/ser0000269. [DOI] [PubMed] [Google Scholar]
- 30.Pfeiffer PN, King C, Ilgen M, et al. Development and pilot study of a suicide prevention intervention delivered by peer support specialists. Psychological Services. 2019;16(3):360–371. doi: 10.1037/ser0000257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gagne CA, Finch WL, Myrick KJ, et al. Peer Workers in the Behavioral and Integrated Health Workforce: Opportunities and Future Directions. American Journal of Preventive Medicine. 2018;54. [DOI] [PubMed]
- 32.Kohls E, Hug J, Stahl M, et al. Peer counseling in depression care: A pilot study in a psychiatric inpatient setting. Psychiatry Research. 2018;270:698–704. doi: 10.1016/j.psychres.2018.10.058. [DOI] [PubMed] [Google Scholar]
- 33.Pretorius C, Chambers D, Coyle D. Young People’s Online Help-Seeking and Mental Health Difficulties: Systematic Narrative Review. Journal of Medical Internet Research. 2019;21(11):e13873–e13873. doi: 10.2196/13873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reardon T, Harvey K, Baranowska M, et al. What do parents perceive are the barriers and facilitators to accessing psychological treatment for mental health problems in children and adolescents? A systematic review of qualitative and quantitative studies. European Child & Adolescent Psychiatry. 2017;26(6):623–647. doi: 10.1007/s00787-016-0930-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry. 2010;10:113–113. doi: 10.1186/1471-244X-10-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Record RA, Silberman WR, Santiago JE, et al. I Sought It, I Reddit: Examining Health Information Engagement Behaviors among Reddit Users. Journal of Health Communication. 2018;23(5):470–476. doi: 10.1080/10810730.2018.1465493. [DOI] [PubMed] [Google Scholar]
- 37.Redding RE, Herbert JD, Forman EM, et al. Popular self-help books for anxiety, depression, and trauma: How scientifically grounded and useful are they? Professional Psychology: Research and Practice. 2008;39(5):537–545. doi: 10.1037/0735-7028.39.5.537. [DOI] [Google Scholar]
- 38.Armstrong N, Powell J. Patient perspectives on health advice posted on Internet discussion boards: a qualitative study. Health Expectations. 2009;12(3):313–320. doi: 10.1111/j.1369-7625.2009.00543.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Substance Abuse and Mental Health Services Administration. What are Peer Recovery Support Services? HHS Publication No. SMA 09-4454, Rockville, MD: Substance Abuse and Mental Health Services Administration, U.S. Department of Health and Human Services, 2009.
- 40.Bethune S. Gen Z more likely to report mental health concerns. Monitor on Psychology. 2019; 50(1). Available online at https://www.apa.org/monitor/2019/01/gen-z. Accessed on January 29, 2020.
- 41.Substance Abuse and Mental Health Services Administration . Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health. NSDUH Series H-54, HHS Publication No. PEP19-5068. Center for Behavioral Health Statistics and Quality: Rockville, MD; 2019. [Google Scholar]
- 42.Spence R, Owens-Solari M, Goodyer I. Help-seeking in emerging adults with and without a history of mental health referral: a qualitative study. BMC Research Notes. 2016;9(1):415. doi: 10.1186/s13104-016-2227-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Whitaker C, Stevelink S, Fear N. The use of Facebook in recruiting participants for health research purposes: A systematic review. Journal of Medical Internet Research. 2017;19(8):e290. doi: 10.2196/jmir.7071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dworkin J, Hessel H, Gliske K, et al. A comparison of three online recruitment strategies for engaging parents. Family Relations. 2016;65:550–561. doi: 10.1111/fare.12206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Albert PR. Why is depression more prevalent in women? The Journal of Psychiatry & Neuroscience. 2015;40(4):219–221. doi: 10.1503/jpn.150205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pratap A, Neto EC, Snyder P, et al. Indicators of retention in remote digital health studies: a cross-study evaluation of 100,000 participants. npj Digital Medicine. 2020;3(1):21. doi: 10.1038/s41746-020-0224-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Torales J, O’Higgins M, Castaldelli-Maia J, et al. The outbreak of COVID-19 coronavirus and its impact on global mental health. The International Journal of Social Psychiatry. 2020;66(4):317–320. doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- 48.Gruber J, Prinstein M, Abramowitz JS, et al. Mental Health and Clinical Psychological Science in the Time of COVID-19: Challenges, Opportunities, and a Call to Action. Available online at https://psyarxiv.com/desg9. Accessed on August 20, 2020. [DOI] [PMC free article] [PubMed]
- 49.Bower P, Gilbody S. Stepped care in psychological therapies: access, effectiveness and efficiency: Narrative literature review. The British Journal of Psychiatry. 2005;186(1):11–17. doi: 10.1192/bjp.186.1.11. [DOI] [PubMed] [Google Scholar]
- 50.Strauss C, Arbon A, Barkham M, et al. Low-Intensity Guided Help Through Mindfulness (LIGHTMIND): study protocol for a randomised controlled trial comparing supported mindfulness-based cognitive therapy self-help to supported cognitive behavioural therapy self-help for adults experiencing depression. Trials. 2020;21:374. doi: 10.1186/s13063-020-04322-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nicholas J, Ringland KE, Graham AK, et al. Stepping Up: Predictors of ‘Stepping’ within an iCBT Stepped-Care Intervention for Depression. International Journal of Environmental Research and Public Health. 2019;16(23):4689. doi: 10.3390/ijerph16234689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Levin ME, Hicks ET, Krafft J. Pilot evaluation of the stop, breathe & think mindfulness app for student clients on a college counseling center waitlist. Journal of American College Health. 2020. Published online ahead of print March 9, 2020. [DOI] [PubMed]
- 53.Gulliver A, Banfield M, Morse AR, et al. A Peer-Led Electronic Mental Health Recovery App in a Community-Based Public Mental Health Service: Pilot Trial. JMIR Formative Research. 2019;3(2):e12550. doi: 10.2196/12550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kumar D, Tully LM, Iosif AM, et al. A Mobile Health Platform for Clinical Monitoring in Early Psychosis: Implementation in Community-Based Outpatient Early Psychosis Care. JMIR Mental Health. 2018;5(1):e15. doi: 10.2196/mental.8551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dennis CL, Hodnett E, Kenton L, et al. Effect of peer support on prevention of postnatal depression among high risk women: multisite randomised controlled trial. The British Medical Journal. 2009;338:a3064. doi: 10.1136/bmj.a3064. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 19 kb)