Abstract
Ultrasonographic measurement of optic nerve sheath diameter (ONSD) has been validated to detect and monitor the increased intracranial pressure (IICP) in neurosurgical field. Especially, the ONSD has been known to reflect well the ICP in case of intracranial hemorrhage (ICH) occurring in the anterior circulation of intracranial vascular system, however it has not been well elucidated the role of ONSD in the posterior circulating vascular problems. A 43-year-old man presented with a subarachnoid hemorrhage with intraventricular hemorrhage due to rupture of dissecting aneurysm at right vertebral artery, and immediately performed the stent-assisted coil embolization. Two day after coil embolization, he became nearly alert without definite neurologic deficits. The ONSD was reduced from 5.8 mm to 5.5 mm. The 10th postoperative days, the patient suddenly changed into stuporous mentality due to rebleeding of aneurysm. The ONSD was enlarged to 6.7 mm. We report a case of intimate relationship between ONSD and IICP after rupture of dissecting aneurysm located in posterior circulation.
Keywords: Optic nerve sheath diameter, Intracranial pressure, Ultrasonography
INTRODUCTION
Accurately measuring changes in intracranial pressure (ICP) has become a very important issues in the clinical setting for the diagnosis and management in neurosurgical field. There are multiple techniques and several devices to measure ICP: invasive and noninvasive [6]. When neurosurgical treatment is needed to control the increased ICP (IICP), ICP measuring can be undertaken in several anatomical spaces by putting the devices into the spaces: intraventricular, intraparenchymal, epidural, subdural, and subarachnoidal [6,14]. However, as non-invasive neurosurgical treatment such as coil embolization has recently been developed and expanded, non-invasive methods of measuring serial ICP during operation have become increasingly necessary.
Optic nerve sheath diameter (ONSD) has been explored as an indirect and alternative diagnostic method for detection of IICP [4,10,16,17]. Helmke and Hansen first introduced the correlation between intracranial hypertension and increase of ONSD, as measured with a linear ultrasonography [7]. Anatomically, optic nerve is surrounded by arachnoid membrane, the inside of which is filled with the cerebrospinal fluid (CSF). Under normal ICP, adequate CSF flows around the optic nerve, but in the case of an IICP, the ONSD get bigger and bigger as the CSF fills the subarachnoid space.
Because the optic nerve is mainly located in anterior cranial fossa, ONSD can well reflect the ICP in case of intracranial hemorrhage (ICH) occurring in the anterior circulation of intracranial vascular system [11], however there has not been known whether IICP from the posterior circulation system quickly and accurately reflect the real time change of the ONSD or not. Although the basal cisterns were connected each other, the cerebrum and cerebellum were separated by tentorium. I wondered how the IICP caused by posterior circulation lesion affects the ONSD.
We report a case of intimate relationship between ONSD and IICP after ruptured dissecting aneurysm located in posterior circulation.
Case Illustration
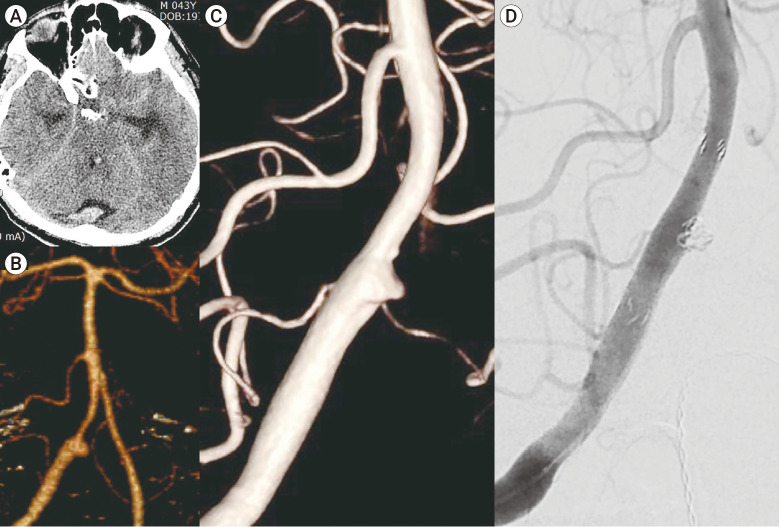
A 43-year-old previously healthy man patient was presented to emergency department due to stuporous mental change after sudden headache. He had no history of trauma or medication. Brain computed tomographic (CT) scan showed a subarachnoid hemorrhage (SAH) in perimesencephalic and ambient cisterns mainly and intraventricular hemorrhage (IVH) at both lateral and 4th ventricles due to aneurysmal rupture in right distal vertebral artery (VA) (Fig. 1A, B). Digital subtraction angiography (DSA) revealed a broad-necked small aneurysm with triangular shape in the right VA, indicating a spontaneous dissecting aneurysm (Fig. 1C). The size of aneurysm measured 3.5 (width)×2.7 (height)×3.6 mm (neck). I planned the stent-assisted coil embolization to save the posterior inferior cerebellar artery (PICA) emerging at opposite site of dissecting aneurysm in right vertebral artery. I checked the bilateral ONSD of patient and measured average 5.7 mm preoperatively.
Fig. 1.
(A, B) A 43-year-old man presented with subarachnoid hemorrhage and intraventricular hemorrhage due to ruptured aneurysm at vertebral artery (VA) on CT angiography. (C) Digital subtraction angiography (DSA) revealed a broad-necked small aneurysm with triangular shape in the right VA, indicating a spontaneous dissecting aneurysm. (D) Double overlapping stent assisted coil embolization was performed successfully using Enterprise stent 4.5 x 23 mm, resulting in complete aneurysmal occlusion.
After guiding catheter insertion, a microcatheter was placed through the dissection segment in the right VA. The other microcatheter was guided into the small sac of the dissecting aneurysm carefully. After making a frame with detachable coil 2.5×35 mm, the Enterprise stent (CERENOVUS, Irvine, CA, USA) 4.5×23 mm was deployed to cover the broad aneurysm neck. Subsequently, detachable coils 2×30 mm and 1×30 mm were inserted into the aneurysm, but a portion of the last coil loop was protruded into the VA. Double overlapping stent assisted coil embolization was performed successfully using Enterprise stent 4.5×23 mm, resulting in complete aneurysmal occlusion (Fig. 1D).
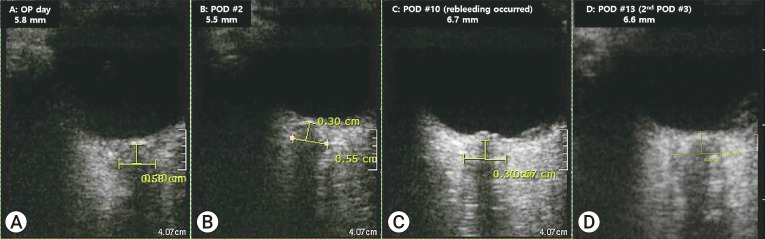
Immediately after coil embolization, I checked the bilateral optic nerve sheath diameter (ONSD) and it was measured average 5.8 mm (Fig. 2A). Subsequently, the patient was transferred to the intensive care unit and lumbar puncture was done to measure ICP and drain the CSF. The ICP was measured at 37 cmH2O.
Fig. 2.
Measurements of optic nerve sheath diameter in a 43-year-old man with subarachnoid hemorrhage due to dissecting aneurysm at vertebral artery. (A) US showed the enalarged optic nerve sheath diameter (ONSD) in first visit day. (B) In postoperative 2 days, the ONSD on US was decreased from 5.7 to 5.5 mm. (C) Postoperative 10 days of aneurysm rebleeding, emergent US measured value of ONSD increased to 6.7 mm. (D) Postoperative 13 days, ONSD was measured 6.6 mm.
Postoperative 2 day after coil embolization, he became nearly alert without definite neurologic deficits. The ONSD was reduced from 5.8 mm to 5.5 mm (Fig. 2B).
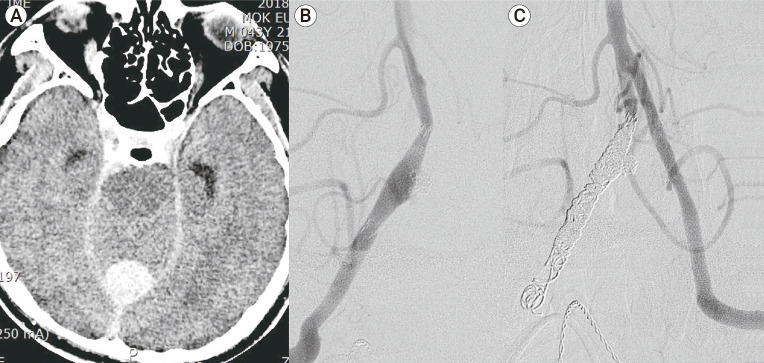
The 10th postoperative days, the patient suddenly changed into stuporous mentality. In order to rule out whether the cause of mental change was an IICP or epileptic seizure, the ONSD was measured before arranging the CT chamber. It was measured 6.7 mm (Fig. 2C). Brain CT scan showed a more increased subarachnoid hemorrhage (SAH) in perimesencephalic and ambient cisterns and intraventricular hemorrhage (IVH) at 4th ventricles and cisterna magna mainly (Fig. 3A). There was no reopening of aneurysm sac, however, fusiform dilatation was seen on the right distal VA about 12 mm length×4.3 mm width, suggesting that dissection of VA had progressed on cerebral angiography (Fig. 3B). The patient underwent emergent trapping of VA dissection using detachable coils (Fig. 3C). In order to control IICP, subsequent emergent extraventricular drainage (EVD) catheter insertion was done after trapping. I checked the elevated ICP of 40 cmH2O. The 13th postoperative days, ONSD on US was measured average 6.6 mm (Fig. 2D).
Fig. 3.
(A) The 10th postoperative days, Brain CT scan showed a more increased subarachnoid hemorrhage (SAH) in perimesencephalic and ambient cisterns and intraventricular hemorrhage (IVH) at 4th ventricles and cisterna magna mainly. (B) Fusiform dilatation was seen on the right distal VA about 12 mm (length)×4.3 mm (width), suggesting that dissection of VA had progressed on cerebral angiography. (C) The patient underwent emergent trapping of VA dissection using detachable coils.
ONSD measurement protocol
The ultrasonographic measurement was carried out by two neurosurgeons. The ONSD measurement was performed approximately 3 minutes prior to and after coil embolization. The ONSD was measured with the handheld ultrasound (Vscan Extend, GE Healthcare, NY, USA), using a broad-bandwidth linear array probe with 3.3-8.0 MHz. The patient was examined in a supine position. To protect the eyeball cornea, thin and soft transparent silicone tape was applied to periorbital skin (Fig. 4). The probe was gently placed on the mid-portion eyelid with ultrasound gel. In order to detect the suitable angle to display the ONSD into eyeball, the probe was adjusted several times. The Vscan Extend has a mode that supports the requirements of ophthalmic sonography. ONSD measurements were performed at a depth of 3 mm behind eye globe. The first measurement was performed in the transverse section and the second measurement was performed in the vertical section. The reported diameter was calculated by mean of the values.
Fig. 4.
Measurement of the diameter using optic nerve ultrasonography. Gentle apposition of the linear probe on the patient’s closed eyeball under general anesthesia.
DISCUSSION
Non-invasive technique such as transcranial doppler (TCD), tympanic membrane displacement (TMD) and ultrasonography (US) have been applied to detect IICP. The reasons why the study to measure the ICP using US is continuously developed, are able to easily and rapidly check the IICP in emergency situation and to predict the real time change of IICP.
Because the optic nerve and sheath are contiguous with the brain and formed by the dura mater anatomically, cerebrospinal fluid (CSF) can move freely through the subarachnoid spaces (SAS) of intracranial areas. These SAS expand in intraorbital areas. IICP leads to a shift of CSF into the ONS, subsequently resulting in anterior portion enlargement of ONS due to CSF accumulation [7,8,13]. Therefore, ONSD was assessed 3 mm behind the optic globe.
Blaivas et al. first demonstrated a close correlation between enlargement of ONSD on ocular US and IICP on head CT [3]. As many studies have been conducted on IICP-related ONSD using US, the more than 5.2 mm has been accepted as a cutoff value of IICP [1,5,9,12,15]. In the study for Korean population with moderate hematoma, an optimal cut-off value of ONSD for detecting IICP was 5.6 mm [8].
There is controversy over whether it is well reflected in patients with aneurysmal SAH. Yesilaras et al. reported that assessment of ONSD in head CT taken with spontaneous SAH suspicion may contribute to the diagnoses of spontaneous SAH [17]. Also, in the study by Lee et al., the ONSDs of aneurysmal SAH patients with poor neurological outcome were significantly greater that those with a favorable neurological outcome, meaning that ONSD has the prognostic value in patients with SAH [11]. However, in contrast, recent studies have reported that the ONSD may not reflect IICP in patients with aneurysmal SAH [18]. Bauerle et al. reported that 27 patients with acute aneurysmal SAH did not show any correlations between ONSD by US and IICP [2]. In a study of 20 patients with aneurysmal SAH by Zoerle et al., ONSD measurements using US were related poorly to the ICP measured directly and simultaneously through ventricular catheters [18]. Two studies explained two possible reasons. First is an impaired retraction capacity of the ONS after severe ICP exposure more than 45 mmHq. Second is a restricted CSF circulation along the optic nerve sheath [2].
Researches on how well the ONSD reflects ICP is still ongoing. The factors affecting correlation are not well known. In this study, the ONSD reflected well the change of real time ICP even in the case of aneurysmal SAH happened in the posterior circulation vascular system. If neurosurgeon can easily, quickly and accurately predict the ICP through US, rapid and optical management may be possible. First, it can be of great help in the initial discrimination of causes of mentality change that occur after treatment, whether it is due to an increase of ICP or a change in consciousness due to secondary causes such as medical problems and epilepsy. In this case, I could get help promptly through US that the ICP was elevated by quickly checking ONSD before the CT exam. Second, the change of ICP can be predicted through real-time change of ONSD through US. In particular, it is thought that it is possible to rapidly control the ICP through hybrid surgery when the cerebral aneurysm ruptured during endovascular coiling and the ICP increased above the cut-off value.
CONCLUSIONS
ONSD measurement using Hand-held US is rapid and efficient method to evaluate IICP caused by the posterior circulating vascular problem in emergent situation. More studies are needed to determine whether there is a correlation between IICP and ONSD in patients with SAH.
Acknowledgments
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-2020R1/1A3073930).
Footnotes
Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
REFERENCES
- 1.Amini A, Kariman H, Arhami Dolatabadi A, Hatamabadi HR, Derakhshanfar H, Mansouri B, et al. Use of the sonographic diameter of optic nerve sheath to estimate intracranial pressure. Am J Emerg Med. 2013 Jan;31(1):236–9. doi: 10.1016/j.ajem.2012.06.025. [DOI] [PubMed] [Google Scholar]
- 2.Bauerle J, Niesen WD, Egger K, Buttler KJ, Reinhard M. Enlarged optic nerve sheath in aneurysmal subarachnoid hemorrhage despite normal intracranial pressure. J Neuroimaging. 2016 Mar-Apr;26(2):194–6. doi: 10.1111/jon.12287. [DOI] [PubMed] [Google Scholar]
- 3.Blaivas M, Theodoro D, Sierzenski PR. Elevated intracranial pressure detected by bedside emergency ultrasonography of the optic nerve sheath. Acad Emerg Med. 2003 Apr;10(4):376–81. doi: 10.1111/j.1553-2712.2003.tb01352.x. [DOI] [PubMed] [Google Scholar]
- 4.Chen LM, Wang LJ, Hu Y, Jiang XH, Wang YZ, Xing YQ. Ultrasonic measurement of optic nerve sheath diameter: a non-invasive surrogate approach for dynamic, real-time evaluation of intracranial pressure. Br J Ophthalmol. 2019 Apr;103(4):437–41. doi: 10.1136/bjophthalmol-2018-312934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Geeraerts T, Merceron S, Benhamou D, Vigue B, Duranteau J. Non-invasive assessment of intracranial pressure using ocular sonography in neurocritical care patients. Intensive Care Med. 2008 Nov;34(11):2062–7. doi: 10.1007/s00134-008-1149-x. [DOI] [PubMed] [Google Scholar]
- 6.Harary M, Dolmans RGF, Gormley WB. Intracranial pressure monitoring-review and avenues for development. Sensors (Basel) 2018 Feb;18(2):465. doi: 10.3390/s18020465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Helmke K, Hansen HC. Fundamentals of transorbital sonographic evaluation of optic nerve sheath expansion under intracranial hypertension II. Patient study. Pediatr Radiol. 1996 Oct;26(10):706–10. doi: 10.1007/BF01383384. [DOI] [PubMed] [Google Scholar]
- 8.Jeon JP, Lee SU, Kim SE, Kang SH, Yang JS, Choi HJ, et al. Correlation of optic nerve sheath diameter with directly measured intracranial pressure in Korean adults using bedside ultrasonography. PLoS One. 2017 Sep;12(9):e0183170. doi: 10.1371/journal.pone.0183170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim DH, Jun JS, Kim R. Ultrasonographic measurement of the optic nerve sheath diameter and its association with eyeball transverse diameter in 585 healthy volunteers. Sci Rep. 2017 Nov 21;7(1):15906. doi: 10.1038/s41598-017-16173-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Feasibility of optic nerve sheath diameter measured on initial brain computed tomography as an early neurologic outcome predictor after cardiac arrest. Acad Emerg Med. 2014 Oct;21(10):1121–8. doi: 10.1111/acem.12477. [DOI] [PubMed] [Google Scholar]
- 11.Lee S, Kim YO, Baek JS, Ryu JA. The prognostic value of optic nerve sheath diameter in patients with subarachnoid hemorrhage. Crit Care. 2019 Feb 26;23(1):65. doi: 10.1186/s13054-019-2360-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moretti R, Pizzi B. Optic nerve ultrasound for detection of intracranial hypertension in intracranial hemorrhage patients: confirmation of previous findings in a different patient population. J Neurosurg Anesthesiol. 2009 Jan;21(1):16–20. doi: 10.1097/ANA.0b013e318185996a. [DOI] [PubMed] [Google Scholar]
- 13.Morgan WH, Balaratnasingam C, Lind CR, Colley S, Kang MH, House PH, et al. Cerebrospinal fluid pressure and the eye. Br J Ophthalmol. 2016 Jan;100(1):71–7. doi: 10.1136/bjophthalmol-2015-306705. [DOI] [PubMed] [Google Scholar]
- 14.Raboel PH, Bartek J, Jr, Andresen M, Bellander BM, Romner B. Intracranial pressure monitoring: invasive versus non-invasive methods-a review. Crit Care Res Pract. 2012;2012:950393. doi: 10.1155/2012/950393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Soldatos T, Karakitsos D, Chatzimichail K, Papathanasiou M, Gouliamos A, Karabinis A. Optic nerve sonography in the diagnostic evaluation of adult brain injury. Crit Care. 2008;12(3):R67. doi: 10.1186/cc6897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yanamandra U, Gupta A, Yanamandra S, Das SK, Patyal S, Nair V. Bedside ultrasonography as an alternative to computed tomography scan for the measurement of optic nerve sheath diameter. J Neurosci Rural Pract. 2018 Apr-Jun;9(2):252–5. doi: 10.4103/jnrp.jnrp_537_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yesilaras M, Kilic TY, Yesilaras S, Atilla OD, Oncel D, Camlar M. The diagnostic and prognostic value of the optic nerve sheath diameter on CT for diagnosis spontaneous subarachnoid hemorrhage. Am J Emerg Med. 2017 Oct;35(10):1408–13. doi: 10.1016/j.ajem.2017.04.022. [DOI] [PubMed] [Google Scholar]
- 18.Zoerle T, Caccioppola A, D’Angelo E, Carbonara M, Conte G, Avignone S, et al. Optic nerve sheath diameter is not related to intracranial pressure in subarachnoid hemorrhage patients. Neurocrit Care. 2020 Oct;33(2):491–8. doi: 10.1007/s12028-020-00970-y. [DOI] [PubMed] [Google Scholar]