Abstract
Objective
To evaluate the impact of coronavirus disease 2019 (COVID‐19) on emergency medical services (EMS) use for time‐sensitive medical conditions. We examined EMS use for cardiac arrest, stroke, and other cardiac emergencies across Massachusetts during the peak of the COVID‐19 pandemic, evaluating their relationship to statewide COVID‐19 incidence and a statewide emergency declaration.
Methods
A retrospective analysis of all EMS calls between February 15 and May 15, 2020 and the same time period for 2019. EMS call volumes were compared before and after March 10, the date of a statewide emergency declaration.
Results
A total of 408,758 calls were analyzed, of which 49,405 (12.1%) represented stroke, cardiac arrest, or other cardiac emergencies. Average call volume before March 10 was similar in both years but decreased significantly after March 10, 2020 by 18.7% (P < 0.001). Compared to 2019, there were 35.6% fewer calls for cardiac emergencies after March 10, 2020 (153.6 vs 238.4 calls/day, P < 0.001) and 12.3% fewer calls for stroke (40.0 vs 45.6 calls/day, P = 0.04). Calls for cardiac arrest increased 18.2% (28.6 vs 24.2 calls/day, P < 0.001). Calls for respiratory concerns also increased (208.8 vs 199.7 calls/day, P < 0.001). There was no significant association between statewide incidence of COVID‐19 and EMS call volume.
Conclusions
EMS use for certain time‐sensitive conditions decreased after a statewide emergency declaration, irrespective of actual COVID‐19 incidence, suggesting the decrease was related to perception instead of actual case counts. These findings have implications for public health messaging. Measures must be taken to clearly inform the public that immediate emergency care for time‐sensitive conditions remains imperative.
1. BACKGROUND
1.1. Background
Since its emergence in December 2019, coronavirus disease 2019 (COVID‐19) has spread rapidly across the globe. In the United States, cases of COVID‐19 began rising sharply in March 2020, with a national emergency declared on March 13. Yet despite the substantial morbidity caused by this global pandemic, US emergency department (ED) visits decreased significantly throughout March 2020, irrespective of local COVID‐19 prevalence. 1 Similarly, emergency medical services (EMS) experienced an over 25% decrease in call volume nationally between early March and mid‐April despite a near‐doubling of EMS‐reported on scene deaths. 2
1.2. Importance
Certain time‐sensitive conditions including cardiac emergencies and stroke require rapid evaluation and prompt management, and EMS is often the first link in this chain of survival. Yet despite the importance of rapid medical evaluation for these time sensitive conditions, ED visits for stroke and myocardial infarction decreased suddenly and sharply after week 10 of 2020, 3 suggesting an impact of both stay‐at‐home orders and a growing public fear of engaging the health care system. During the peak of the pandemic in Italy, acute presentations for ST elevation myocardial infarction decreased by 37% with a similar pattern seen in Madrid. 4 In addition, ED visits for low‐acuity stroke decreased in Italy, with more severe strokes on presentation and patients having worse outcomes. 5 Decreased use of emergency services for time‐sensitive conditions during a public health emergency suggests an impact of stay‐at‐home advisories and public fear of engaging the health care system and has implications for public health messaging.
1.3. Goals of this investigation
The goal of this investigation was to determine if EMS contact for time‐sensitive conditions was affected by COVID‐19. In the Commonwealth of Massachusetts, community spread was described beginning in early March, with a State of Emergency declared on March 10 and a “stay‐at‐home” advisory issued on March 24, 2020. We evaluated EMS usage patterns for time‐sensitive conditions including cardiovascular emergencies and stroke across Massachusetts during peak growth in COVID‐19 cases and examined its relationship with statewide incidence of COVID‐19. We hypothesized that EMS contact for these time‐sensitive conditions would decrease proportionally to incidence of COVID‐19 as patients hoped to avoid the ED in the wake of the state's increasing COVID‐19 case counts.
The Bottom Line
This statewide retrospective study evaluated emergency medical services (EMS) usage patterns for time‐sensitive pathologies during peak growth of COVID‐19 in Massachusetts. The authors found a decrease in EMS for cardiac and stroke but an increase in cardiac arrest. This decrease may be because of delay in care for heart attack and stroke.
2. METHODS
2.1. Design
We performed a retrospective analysis of the Massachusetts Ambulance Trip Record Information System (MATRIS), maintained by the Massachusetts Department of Public Health (MADPH) with statutory reporting by all EMS agencies in the state. All EMS data entered into MATRIS is NEMSIS 9.0 compliant. This study was approved by the Mass General Brigham Human Research Committee.
2.2. Setting and selection of patients
All 911 calls originating in Massachusetts for which patient contact was made between February 15 and May 15, 2020 were included. We also included the same time period in 2019.
2.3. Exposure
On March 10, 2020 the Governor of Massachusetts declared a statewide public health emergency. This time point was used to delineate “pre‐COVID‐19″ and “post‐COVID‐19″ periods for 2020.
2.4. Outcomes
Our primary outcomes of interest were EMS calls for the time‐sensitive conditions of stroke, cardiac arrest, and other cardiac emergencies. A secondary analysis evaluated EMS calls for respiratory illness. To determine the reason for each EMS call, we used a hierarchical schema based on previously published methods. 6 Clinical impressions were recoded into 34 categories. If no clinical impression was entered, dispatch reason was used as the reason for the call. Cardiac arrest was not included in the cardiac emergencies category. Specific categorization details are provided in Appendix 1. COVID‐19 case counts were obtained from publicly available data maintained by MADPH.
2.5. Data analysis
Chi‐square tests and t tests examined associations between EMS call volumes and variables related to COVID‐19 including statewide incidence and the enactment of relevant policy. We conducted an interrupted time series analysis using a linear first‐order autoregressive model to evaluate the change in daily EMS call volume after March 10. This approach was designed to evaluate both changes in level and trend associated with the declaration of emergency in Massachusetts. Pearson correlation coefficients were calculated to evaluate the association between overall EMS call volume and both new COVID‐19 cases and cumulative cases at the statewide level on a weekly basis. This association was examined from March 10 through May 15 to mitigate the added effect of the state of emergency declared on March 10. Statistical analysis was performed using Stata IC 15.1 (StataCorp, College Station, TX) and R version 3.6.2 (R Foundation for Statistical Computing, Vienna, Austria).
3. RESULTS
After removing 503 cases with incomplete data 408,758 calls were included, with 190,838 (46.7%) occurring in 2020. Stroke and cardiac emergencies accounted for 12.1% (49,405) of calls. Average daily call volume from February 15 through March 10 was similar in both years (2453 calls/day, 95% confidence interval [CI], 2379‐2527 in 2020 compared to 2414 calls/day, 95% CI, 2342‐2485 in 2019, mean difference 39 calls/day, 95% CI, ‐61 to 139). Daily call volume decreased significantly after March 10, 2020 by 18.7% (1,970 calls/day, 95% CI, 1928‐2011 in 2020 compared to 2424 calls/day, 95% CI, 2386‐2462 in 2019, mean difference ‐454 calls/day, 95% CI, ‐510 to ‐398).
There was a significant level change in daily call volume on March 10, 2020 (‐389 calls/day, 95% CI, ‐616 to ‐163). Thereafter, there was no significant change in daily calls (95% CI, ‐6.0 to 0.5 calls/day) (Figure 1). There was no significant association between EMS call volume and weekly statewide new COVID‐19 case incidence from March 10 through May 15 (r(8) = ‐0.56, P = 0.09). Similarly, there was no association between EMS call volume and cumulative COVID‐19 case counts at the statewide level (r(8) = ‐0.25, P = 0.49).
FIGURE 1.
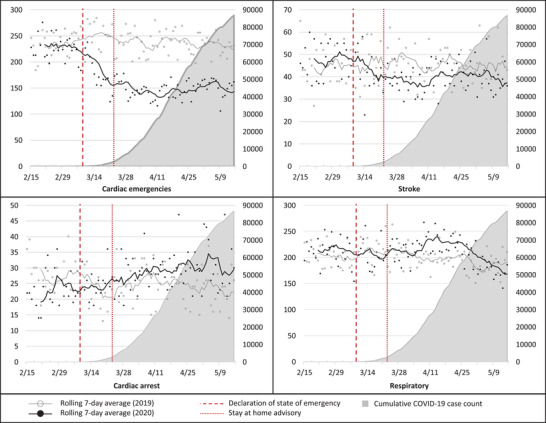
Emergency medical services (EMS) calls for specific medical conditions in 2020 compared to 2019 (left) as a function of statewide cumulative COIVD‐19 case counts (right)
In the pre‐COVID‐19 period, there were no significant differences between the 2020 and 2019 groups in calls for stroke, cardiac emergencies, or respiratory concerns. There were significantly fewer calls for cardiac arrest during this time period in 2019 compared to 2020 (22.9 calls/day, 0.9% of calls for 2020 vs 27.9 calls/day, 1.2% of calls for 2019, mean difference ‐5.0 calls/day, 95% CI, ‐9.2 to ‐1.8).
After excluding out‐of‐hospital cardiac arrest, there were 35.6% fewer calls for cardiac emergencies between March 10 and May 15, 2020 compared to 2019 (153.6 calls/day, 7.8% of calls in 2020 vs 238.4 calls/day, 9.8% of calls in 2019, mean difference ‐84.8 calls/day, 95% CI, ‐92.9 to ‐76.7) and 12.3% fewer calls for stroke in during this same time period for 2020 (40.0 calls/day, 2.0% of calls in 2020 vs 45.6 calls/day, 1.9% of calls in 2019, mean difference ‐5.6 calls/day, 95% CI, ‐8.2 to ‐3.0). Calls for cardiac arrest increased 18.2% (28.6 calls/day, 1.5% of calls in 2020 vs 24.2 calls/day, 1.0% of calls in 2019, mean difference 4.4 calls/day, 95% CI, 2.2‐6.5) though rates of return of spontaneous circulation decreased (16.2% vs 5.5%, difference ‐9.2%, 95% CI, ‐12.5 to ‐6.30%, P < 0.001).
Calls for respiratory concerns also increased from 2019 to 2020 (208.8 calls/day, 10.6% of calls in 2020 vs 199.7 calls/day, 8.2% of calls in 2019, mean difference 9.1 calls/day, 95% CI, 0.1‐18.1). Calls for respiratory concerns peaked from April 6–12 at 12.5% of all calls, about 1 week before the April 21 peak of COVID‐19 hospitalizations. EMS calls for specific medical conditions in 2020 compared to 2019 are shown in Figure 1.
There were small but significant changes in demographics. In the pre‐COVID‐19 period, there were no significant differences in mean age (51.0, 95% CI, 50.7‐51.2 in 2020 vs 51.3, 95% CI, 51.0‐51.5 in 2019) or sex (48.7% male, 95% CI, 48.3%‐49.1% in 2020 vs 48.1% male, 95% CI, 47.7%‐48.5% in 2019). In the 2020 COVID‐19 period, patients were significantly older (mean age 51.8, 95% CI, 51.7‐52.0 vs 50.8, 95% CI, 50.7‐50.9) and there were more male patients (51.1% male, 95% CI, 50.8%‐51.4% vs 48.2% male, 95% CI, 48.0%‐48.5%). Results are presented in Table 1.
TABLE 1.
Comparison of Massachusetts statewide emergency medical services runs for the defined periods of 2019 and 2020. Specific medical concerns are presented as average calls per day and the percentage of daily calls for that condition for the defined time period
| Pre‐COVID‐19 (15 Feb–9 Mar) | Post‐COVID‐19 (10 Mar–15 May) | |||||
|---|---|---|---|---|---|---|
| 2019 | 2020 | Difference (95% CI) | 2019 | 2020 | Difference (95% CI) | |
| Age | 51.3 | 51 | −0.3 (−0.6‐0.03) | 50.8 | 51.8 | 1.0 (0.8‐1.2) |
| (95% CI) | (51.0‐51.5) | (50.7‐51.2) | (50.7‐50.9) | (51.7‐52.0) | ||
| Male | 48.1% | 48.7% | 0.6% (0‐1.2%) | 48.2% | 51.1% | 2.9% (2.5‐3.2%) |
| (95% CI) | (47.7%‐48.5%) | (48.3%‐49.1%) | (48.0%‐48.5%) | (50.8%‐51.4%) | ||
| Calls/day | 2,414 | 2,453 | 39 (−61‐139) | 2,424 | 1,970 | −454 (−510 to‐398) |
| (95% CI) | (2342‐2485) | (2379‐2527) | (2386‐2462) | (1928‐2011) | ||
| Cardiac emergencies (%) | 235.0 (9.7%) | 225.5 (9.2%) | −9.5 (−23.6‐4.7) | 238.4 (9.8%) | 153.6 (7.8%) | −84.8 (−92.9 to ‐76.7) |
| Stroke (%) | 45.2 (1.9%) | 47.5 (1.9%) | 2.3 (−2.5‐7.1) | 45.6 (1.9%) | 40.0 (2.0%) | −5.6 (−8.2 to ‐3.0) |
| Cardiac arrest (%) | 27.9 (1.2%) | 22.9 (0.9%) | −5.0 (−9.2–1.8) | 24.2 (1.0%) | 28.6 (1.5%) | 4.4 (2.2‐6.5) |
| Respiratory (%) | 202.1 (8.4%) | 212.4 (8.7%) | 10.3 (‐3.5‐24.0) | 199.7 (8.2%) | 208.8 (10.6%) | 9.1 (0.1‐18.1) |
CI, confidence interval; COVID‐19, coronavirus disease 2019.
3.1. Limitations
Our study has some limitations. Although Massachusetts uses a standardized data collection platform, there may have been some variation in agency reporting over time. Further, misclassification of patient presentations was possible, though unlikely to have changed during the study period. Our statewide data, analyzed in aggregate, may not account for population shifts occurring between 2019 and 2020 and may not be generalizable to all regions. As COVID‐19 case counts are dependent on community testing rates, the actual prevalence of COVID‐19 in our state may not be accurately reflected in publicly available statewide COVID‐19 case counts. Finally, we saw a significant increase in cardiac arrest in the pre‐COVID period of 2020 and further evaluation of the reasons for this finding should be explored in future work.
4. DISCUSSION
Our study demonstrates a significant reduction in EMS calls for cardiac emergencies and stroke after March 10, 2020, corresponding to a statewide declaration of emergency but before any substantial increase in statewide COVID‐19 incidence. Although the statewide declaration of emergency was associated with a sudden decrease in call volume, we found no correlation between statewide COVID‐19 cases and overall EMS contact. The statewide rise in COVID‐19 incidence that followed was not associated with corresponding reductions in EMS contact. These findings suggest that overall EMS contact was likely subject to a greater influence by the public perception of disease threat than by actual estimates of disease incidence reported over time.
Both myocardial infarction and stroke are time‐sensitive conditions for which rapid evaluation and management are paramount. Yet during the peak of the pandemic, ED presentations for both conditions decreased significantly not only in the United States but across the globe. 3 , 4 , 5 , 7 , 8 In both Italy and Hong Kong, emergent presentations of myocardial infarction decreased during an initial COVID‐19 surge but 7 late presentations increased. 4 In addition, presentations for stroke were delayed, leading to compromised patient outcomes. 5 , 9 Our study demonstrates decreased EMS contacts for potentially emergent conditions in the state of Massachusetts after March 10, 2020, suggesting that patients may have had emergent conditions for which they failed to seek timely medical care. It is possible that some of the increased number of cardiac arrests seen in our study represented late presentations of cardiac conditions, although our study was not designed to answer this specific question.
There are several possible explanations for this decrease in EMS contact including decreased population mobility and fear of contracting COVID‐19. During this period of uncertainty, patients seemed to avoid emergency care owing to a perception that encounters with the health care system might increase infection risk. A national survey conducted in April 2020 reported that 4 out of 5 adults were concerned about contracting COVID‐19 in an ED, and 29% avoided or delayed medical care because of concern about contracting COVID‐19. 10 Patient motivation is an important factor in EMS use. 11 The decline in EMS use for these conditions during our study period is concerning and has implications for public health messaging regarding the safety of receiving emergent medical care, especially considering the significant morbidity associated with delays in obtaining that care. Altruism may have also played a role as patients purposefully avoided medical care for fear of further stressing what they believed to be an overburdened health care system, despite low COVID‐19 case counts and existing health care capacity.
We did see a small but significant change in demographics during the study period. During the COVID‐19 period of 2020, patients were significantly older and there were more male patients. The clinical significance of this small demographic shift is unclear. Finally, it must be noted that cardiac arrests decreased significantly when comparing the pre‐COVID‐19 time period of 2020 to 2019. This trend was reversed during the COVID‐19 period of 2020, with a significant increase in cardiac arrests. Although the direct effects of COVID‐19 may explain some of this change, it is also possible that some of these cases represent delayed presentations of cardiac emergencies. Further research into the impact of COVID‐19 on rates of cardiac arrest are warranted.
Our results demonstrate a sudden and significant decrease in EMS contact across Massachusetts for cardiac emergencies and stroke, unrelated to cumulative or daily COVID‐19 case counts but temporally associated with a statewide declaration of emergency. When implementing statewide public health policy, measures should be taken to clearly inform the public that emergency care for time‐sensitive conditions remains imperative. Further research is needed to determine the impact of changes in EMS contact during the COVID‐19 outbreak on patient outcomes.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to report.
AUTHOR CONTRIBUTIONS
SAG, RS, and PGG conceived the study. SAG was responsible for data collection and REC, GP, and SAG performed the statistical analysis. All authors contributed to manuscript development and revision. SAG takes responsibility for the manuscript as a whole.
Biography
Scott A. Goldberg, MD, MPH, is Assistant Professor of Emergency Medicine, Brigham and Women's Hospital, Boston, MA.

APPENDIX 1.
Clinical impression and dispatch reason categorizations for primary outcomes of cardiac emergency, cardiac arrest, and stroke
| Cardiac |
|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Cardiac Arrest |
|---|
|
|
|
|
|
|
|
|
|
| Stroke |
|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Stroke |
|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Goldberg SA, Cash RE, Peters G, Weiner SG, Greenough PG, Seethala R. The impact of COVID‐19 on statewide EMS use for cardiac emergencies and stroke in Massachusetts. JACEP Open. 2021;2:e12351 10.1002/emp2.12351
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Supervising Editor: David Wampler, PhD.
REFERENCES
- 1. Hartnett KP, Kite‐Powell A, DeVies J, et al. Impact of the COVID‐19 pandemic on emergency department visits ‐ United States, January 1, 2019‐May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699‐704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lerner EB, Newgard CD, Mann NC. Effect of the Coronavirus Disease 2019 (COVID‐19) pandemic on the U.S. Emergency medical services system: a preliminary report. Acad Emerg Med. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lange SJ, Ritchey MD, Goodman AB, et al. Potential indirect effects of the COVID‐19 pandemic on use of emergency departments for acute life‐threatening conditions ‐ United States, January‐May 2020. MMWR Morb Mortal Wkly Rep. 2020;69(25):795‐800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Roffi M, Guagliumi G, Ibanez B. The obstacle course of reperfusion for ST‐segment‐elevation myocardial infarction in the COVID‐19 pandemic. Circulation. 2020;141(24):1951‐1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Naccarato M, Scali I, Olivo S, et al. Has COVID‐19 played an unexpected “stroke” on the chain of survival? J Neurol Sci. 2020;414:116889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Munjal KG, Silverman RA, Freese J, et al. Utilization of emergency medical services in a large urban area: description of call types and temporal trends. Prehosp Emerg Care. 2011;15(3):371‐380. [DOI] [PubMed] [Google Scholar]
- 7. Tam CF, Cheung KS, Lam S, et al. Impact of Coronavirus Disease 2019 (COVID‐19) outbreak on ST‐segment‐elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13(4):e006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Baracchini C, Pieroni A, Viaro F, et al. Acute stroke management pathway during Coronavirus‐19 pandemic. Neurol Sci. 2020;41(5):1003‐1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wong L, Hawkins J, Langness S, Murrell K, Iris P, Sammann A. Where are all the patients? Addressing COVID‐19 fear to encourage sick patients to seek emergency care. NEJM Catalyst Innovations Care Delivery. 2020;1(3). [Google Scholar]
- 10. Consulting Morning . Public Poll: Emergency Care Concerns Amidst COVID‐19. American College of Emergency physicians; 2020. [Google Scholar]
- 11. Fussman C, Rafferty AP, Lyon‐Callo S, Morgenstern LB, Reeves MJ. Lack of association between stroke symptom knowledge and intent to call 911: a population‐based survey. Stroke. 2010;41(7):1501‐1507. [DOI] [PubMed] [Google Scholar]


