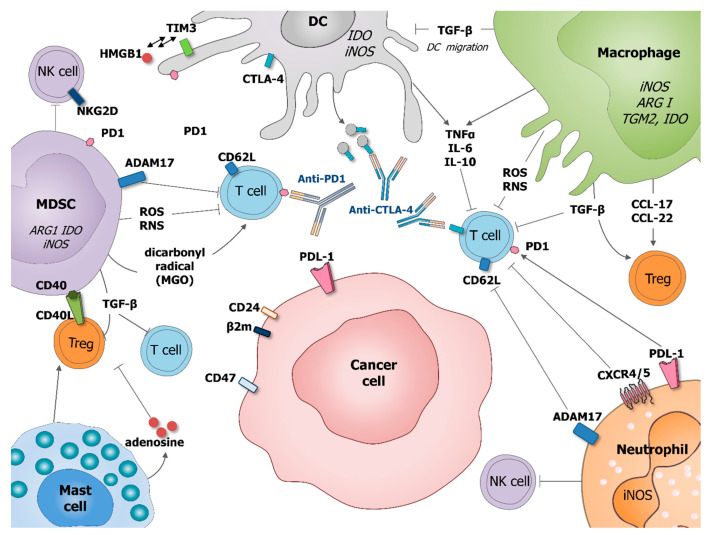
Figure 2.
Role of tumor-associated myeloid cells in cancer cells immune-escape and therapy resistance. Macrophages and MDSC produce transforming growth factor beta (TGF-β) which inhibits DC migration at the tumor site, promote regulatory T cells (Treg) and block T cell activation. Macrophages potentiate Treg activation by production of chemokines CCL-17 and CCL-22. DC express immune checkpoint receptors, such as cytotoxic T-lymphocyte-associated protein 4 (CTLA-4), which can be released on the surface of microvesicles that could block costimulatory molecules, such as CD80/86. DC express also programmed cell death protein 1 (PD-1) and T cell immunoglobulin and mucin domain-containing protein 3 (Tim-3) interacting with HMGB1. MDSC suppress T cell functions by producing ROS and RNS inducing the nitration of TCR and MHC-I, as well as producing dicarbonyl radical methylglyoxal in the TME inhibiting CD8 T cells. MSDC express CD40 interacting with is ligand CD40L present on the surface of Treg. Mast cells can stimulate Treg numbers and secrete adenosine, which inhibits T cell proliferation. Neutrophil, as MDSC, expresses a disintegrin and metalloproteinase 17 (ADAM17) that cleaves the ectodomain of L-selectin (CD62L) on T cells. Neutrophil and cancer cells might express PD1 ligand (PDL-1) which inhibits activation of T cells expressing PD1. Neutrophils express CRCR4/5 leading to the immunosuppression of T-cell proliferation. MDSC and neutrophils, are also able to suppress NK cell cytotoxicity. By diminishing the response of various immune cells, tumor-associated myeloid cells can also negatively influence outcome of anti-cancer therapies, especially various immunotherapies.