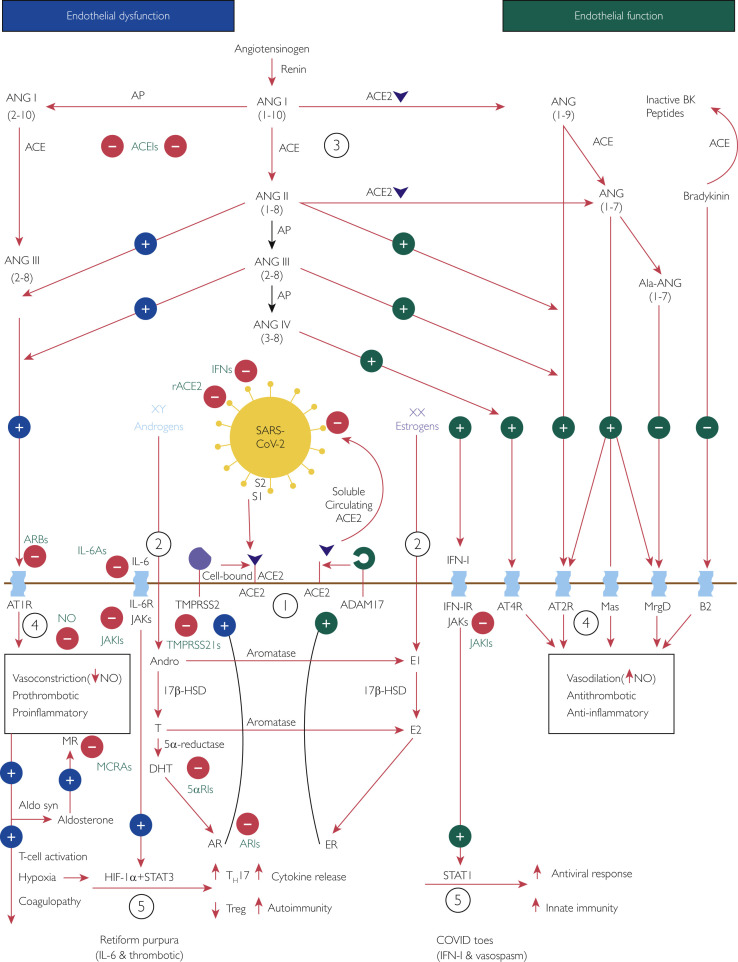
Figure 3.
Interplay of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), angiotensin-converting enzyme (ACE) 2 (ACE2), the renin-angiotensin-aldosterone system (RAAS), sex hormones, and the immune response: a potential mechanism of coronavirus disease (COVID) toes. Used with permission of M.A. Cappel, MD. Circled numbers indicate steps in the mechanism. Step 1: The cellular receptor ACE2 is critically important in SARS-CoV-2 infection.64,65 In addition, transmembrane protease serine 2 (TMPRSS2) is essential because by cleaving cell-bound ACE2 and SARS-CoV-2 spike protein subunit 1 (S1) from spike protein subunit 2 (S2), it facilitates viral cellular entry.65,66,69Step 2: Androgens and estrogens have generally opposing downstream effects on ACE2 processing, providing an explanation for more severe coronavirus disease 2019 (COVID-19) in male patients. TMPRSS2 activity increases with androgen sensitization through dihydrotestosterone activation of the androgen receptor (AR).82 On the contrary, estrogens increase the expression of a disintegrin and metalloproteinase 17 (ADAM17),81 which competes for processing of ACE2 and releases a circulating form of active ACE2.68,69 Therefore, increased ADAM17 activity may be protective in female patients, resulting in an increased proportion of circulating ACE2 that binds any circulating SARS-CoV-2 and prevents further cell infection. Step 3: When cells are infected by SARS-CoV-2, the resulting virus-receptor internalization results in the decreased cell expression of ACE2 and a relative deficiency of ACE2.67 In the RAAS, a delicate balance exists between ACE and ACE2. ACE converts angiotensin (ANG) I (ANGI) to ANGII and, with aminopeptidase, to ANGIII, both of which contribute to endothelial dysfunction through binding the angiotensin type 1 receptor (AT1R).136 On the contrary, ACE2 converts ANGI to ANG1-9 and ANGII to ANG1-7, both of which promote healthy endothelial function through binding the AT2R.136 At baseline, because of sex hormone differences, the ACE–ANGII–AT1R pathway is favored in male patients whereas the ACE2‒ANG1-7‒AT2R pathway is favored in female patients.76Step 4: These RAAS predilections may account for increased endothelial dysfunction in male patients compared with female patients; AT1R stimulation decreases nitric oxide (NO) and is vasoconstricting, prothrombotic, and pro-inflammatory; AT2R stimulation increases NO and is vasodilatory, antithrombotic, and anti-inflammatory.136 Angiotensin II–AT1R activation also potentiates endothelial dysfunction by stimulating aldosterone synthesis and subsequent mineralocorticoid receptor activation, with similar vasculopathic and pro-inflammatory effects.126Step 5: Aldosterone stimulates mineralocorticoid receptors on dendritic cells, and ANGII stimulates AT1Rs on T cells and on dendritic cells; all these actions promote T-cell activation and proliferation.123 This leads to activation of interleukin 6 family (IL-6) cytokine receptors (IL-6Rs), which signal through the Janus kinase (JAK)‒signal transducer and activator of transcription (STAT) 3 pathway,124 and activation of the type I interferon (IFN-I) receptor (IFN-IR), which signals through the JAK-STAT1 pathway.125,128 Tissue hypoxia from the related AT1R-induced endothelial dysfunction may also contribute through hypoxia-inducible factor 1α subunit (HIF-1α) in conjunction with STAT3 to increase pro-inflammatory helper T cell 17s (TH17s) and decrease anti-inflammatory regulatory T cells (Tregs).130 Owing to sex hormone and genetic differences, female patients have a more robust IFN-I‒STAT1 response than do male patients.86,87 Younger individuals have a stronger IFN-I response,94 which favors the development of COVID toes; in older individuals the IL-6 pathway may predominate, which is associated with more severe COVID-19.97 5αRI, 5α-reductase inhibitor; 17β-HSD, 17β-hydroxysteroid dehydrogenase; ACEI, angiotensin-converting enzyme inhibitor; Ala, alamandine; Aldo syn, aldosterone synthase; Andro, androstenedione; AP, aminopeptidase; ARB, angiotensin receptor blocker; ARI, androgen receptor inhibitor; B2, bradykinin receptor B2; BK, bradykinin; DHT, dihydrotestosterone; E1, estrone; E2, estradiol; ER, estrogen receptor; IFN, interferon; IL-6A, IL-6 antagonist; JAKI, Janus kinase inhibitor; Mas, G protein‒coupled receptor Mas receptor; MCRA, mineralocorticoid receptor antagonist; MR, mineralocorticoid receptor; MrgD, Mas-related G protein‒coupled receptor member D; rACE2, recombinant angiotensin-converting enzyme 2; T, testosterone; TMPRSS2I, transmembrane protease serine 2 inhibitor; XX, 2 X chromosomes (genetic female); XY, 1 X chromosome and 1 Y chromosome (genetic male).