Abstract
Extensively drug resistant typhoid fever is a major public health concern in Pakistan. During the COVID-19 pandemic, poor sanitation is leading typhoid cases to a surge and obsolete diagnostic methods are paving the way towards ir-rational pharmacotherapy. In particular, the overuse of azithromycin for the treatment of COVID-19 might impair one of the few remaining regimens against XDR. Facing COVID-19 and XDR at the same time can lead to a catastrophy, unless the government, the stakeholders and healthcare workers take joint action to improve sanitation, educate the public, vaccinate vulnerable groups and establish good diagnostic and management practices.
Keywords: Typhoid, XDR strain, COVID-19, Pakistan
1. Introduction
Pakistan, a developing country, has been navigating the second wave of COVID-19 since October 28, 2020. With low levels of compliance to the lockdown measures, due to fatigue and socio-economic dysfunction, the consequences of the second wave appear quite concerning. What appears also quite concerning but has not been widely addressed so far is the potential overlap of COVID-19 with typhoid fever (see Fig. 1).
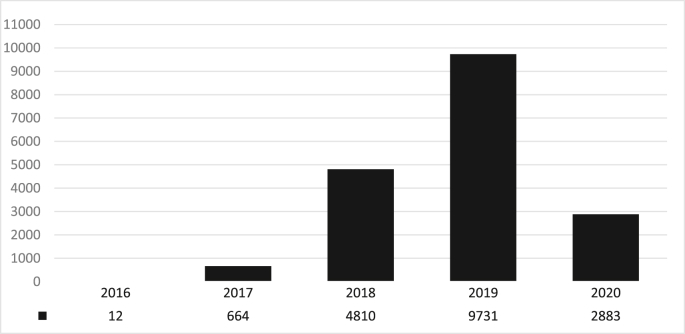
Fig. 1.
XDR typhoid cases in Sindh province of Pakistan, as of September 12, 2020 (13).
Indeed, the extensively drug resistant (XDR) typhoid fever represents a major public health concern in Pakistan and other low and middle – income countries. Not only the poor hygienic conditions and waste management, which are aggravated with the lockdown restrictions, but also the overuse of azithromycin can cause havoc.
In terms of clinical presentation, the symptoms of XDR include fever, loss of appetite, nausea, headache, constipation and sometimes diarrhea and are usually non-specific and undistinguishable from other febrile illnesses and even COVID-19. According to the WHO, between 11 and 21 million cases are recorded worldwide annually, out of whom and 128,000 to 161,000 people succumb. Vulnerable populations and even entire communities lacking scheduled vaccination, adequate sanitation and safe drinking water are most vulnerable to get infected from typhoid. In particular areas of Pakistan where these conditions have been observed, the prevalence of XDR typhoid has risen from 7/100,000 to 15/100,000 [1]. A growing body of literature warning for the implications of infections afflicting communities amid the pandemic on healthcare and society. Hence, a critical reflection on XDR in Pakistan is necessary, to increase vigilance and nurture evidence based interventions.
1.1. XDR in Pakistan
In the past few years, a frequently multidrug-resistant (MDR) haplotype of Salmonella typhi (H58) has spread worldwide and notablyin Asia and some parts of Africa. First line of antibiotics, namely ampicillin, chloramphenicol, and trimethoprim-sulfamethoxazole according to the WHO, are invariably ineffective in treating MDR typhoid patients. MDR and quinolone-resistant strains of S. Typhi have a devastating impact on the health sector in Pakistan.
A study from 2001 to 2006 at Aga Khan University in Pakistan concluded that the multidrug resistance rate for S. Typhi strains has increased from 34.2% to 48.5%, and resistant strains against quinolones spiked from 1.6% to 64.1% [2]. Third-generation cephalosporins, such as ceftriaxone, are being optimized for the treatment after the increase in fluoroquinolone-resistant Salmonella typhi strains. However, from November 2016, there has been a spike in the ceftriaxone-resistant cases of typhoid infections. It is proposed that S. Typhi can acquire a plasmid to convert from MDR to XDR clade and render all recommended lines of treatment useless. Thereby, the outburst of typhoid infections was attributed to the H58 variant. The harboring of its XDR variant on IncY plasmids and the bla CTX-M-15 gene, lead to fluoroquinolone and ceftriaxone resistance respectively [3].
In November 2019, Pakistan became the first-ever country to introduce the typhoid conjugate vaccine, that was approved by the WHO at the time [4]. Out of 16 Asian countries, where typhoid is prevalent, the inhabitants of Sindh and Punjab provinces of Pakistan were found to be the most vulnerable to contract typhoid fever [5]. Extensively drug resistant strain of typhoid (XDR) was reported in Hyderabad on November 2016 [6].
Before COVID-19, from 1 November 2016 to 16 February 2020, public health authorities of Pakistan (NIH) reported a total of 22,571 typhoid cases from the province of Sindh in Pakistan. Sixteen thousands of these patients were found to have extensively drug-resistant typhoid (XDR). The prevalence of typhoid was estimated to be 15.5/10,000 population. XDR typhoid, being resistant to all available antibiotics, has an exceptionally costly and complicated management. The number of infectees has exceeded 19,000, and most of these people come from the province of Sindh, Pakistan where the first case of COVID-19 was reported on February 28, 2020 [7].
1.2. Implications of COVID-19 on XDR strain of typhoid
Since 12 September 2020, 2883 XDR cases of typhoid have been reported in Pakistan [8]. Most of these cases have been treated with Azithromycin and Carbopenems. With the advent of this pandemic, azithromycin has gained ground in the treatment of COVID-19.
On top of prescribed azithromycin, self-medication practices have been very prevalent among the locals. Although relevant evidence from Pakistan is not available to our knowledge, a study in Nigeria reported that the mass use of Azithromycin can also cause resistance to other antibiotics [9].
Hence, the overuse of azithromycin appears as a red flag for the future management of the XDR strain of typhoid. The potential side effects and the high cost of carbopenems, the only available alternative in case of azithromycin – resistant XDR typhoid, are additional factors of consideration.
Additionally, given that the diagnosis of typhoid is in most cases clinical, due to the lack of laboratories, not only overuse of azithromycin is intensified, but also diseases with similar clinical presentation such as dengue, malaria and even COVID-19 can be missed. Another limitation of Typhoid fever diagnosis in Asian countries, especially in Pakistan is the fact that mainstay typhoid testing methods such as Widal test and Typhidot have low sensitivity and specificity. Switching to blood cultures, the most reliable test for the diagnosis of typhoid on hand, with the existing laboratories being overwhelmed by COVID-19 tests appears to be unrealistic [10].
Certainly, beyond the laboratories, the hospitals in total get overwhelmed due to the COVID-19 pandemic, posing a burden for healthcare workers and patients with typhoid. The mutual differential diagnosis of COVID-19 and typhoid is challenging physicians, who have to rely on clinical diagnosis in most cases. What is more troublesome is the likelihood of patients with typhoid being infected with COVID-19.
1.3. An action plan
To control the spread of the virus, the Pakistani authorities have taken profuse measures. The first step of any action plan is awareness, and in this case, it is important that the authorities have realized that mounting cases of COVID-19 and an unprecedented level of pressure on the poorly equipped healthcare facilities bring the country on the verge of collapse.
Imposing strict lockdowns to control the situation is a challenging choice for the government. In case such a decision is made, a considerate investment in time and infrastructure is necessary. Apart from supplying and increasing healthcare facilities, the authorities can take action to improve sanitation and provide clean, filtered water to the public, if they want to prevent rather than treat typhoid.
Vaccination is another key player in the field of typhoid prevention, and hence vaccinating children with the typhoid vaccine should also be prioritized. Statistics from all the regions of Pakistan suggest that children and adolescents account for the majority of typhoid cases. Although young people are more likely to have a favorable outcome, the purpose of vaccination is this population group is twofold. On top of stimulating cellular and humoral immunity, vaccines can generate health literacy. Young people will be the best ambassadors of vaccination to their offsprings within the coming decade. Spreading this kind of health literacy might improve the attitude of the population towards the forthcoming COVID-19 vaccines as well.
Stakeholders and civil society hold also a share on health literacy. Civil society, youth organizations – especially those with a scientific focus – news outlets and even influencers and brands can use their outreach to increase awareness about the positive impact of precautionary measures on the spread of the disease and the devastating after-math of epidemics that go out of control. At the same time, they can facilitate contests and hackathons providing endorsement and networking to individuals or teams with innovative ideas.
The aforementioned strategy will most likely have long-term benefits. Until these benefits come into effect those, healthcare facilities need to be prepared to tackle both COVID-19 and XDR. A regulatory approach in healthcare, would emphasize on the necessity of a concrete diagnosis is needed before prescribing any medications, and particularly broad spectrum antibiotics, to control the already growing antimicrobial resistance. While issuing guidelines is a standard practice, launching informative campaigns and educational sessions for healthcare workers could make the difference.
Overall, COVID-19 and XDR typhoid is a battle that Pakistani healthcare workers, authorities, civil society and civilians should stand united against. Pakistan this year has responded well to epidemics and has managed to control them despite the pandemic but the possible implications of COVID-19 can be long lasting.
Reminiscing the successes of the past and the strategies that turned the tide is quite useful during the current public health crisis. Similar zeal and determination will be required to attenuate the detrimental sequel of the XDR typhoid epidemic and the COVID-19 pandemic in Pakistan.
Funding
None.
Authorship contribution
∗∗.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
We would like to present our deepest gratitude to the respected reviewers for reviewing this manuscript.
Contributor Information
Shoaib Ahmad, Email: shoaibahmad442@gmail.com.
Christos Tsagkaris, Email: chriss20x@gmail.com.
Abdullahi Tunde Aborode, Email: ambassadorabdullah0@gmail.com.
Muhammad Tanzeel Ul Haque, Email: tanzeel.haq97@gmail.com.
Shayan Iqbal Khan, Email: shayan_7125@hotmail.com.
Uzzam Ahmed Khawaja, Email: uzzamahmedkhawaja@gmail.com.
Ana Carla dos Santos Costa, Email: anacsc@ufba.br.
Mohammad Yasir Essar, Email: Yasir.essar@gmail.com.
Don Eliseo Lucero-Prisno, III, Email: don-eliseo.lucero-prisno@lshtm.ac.uk.
References
- 1.Rasheed M.K., Hasan S.S., Babar Z.U., Ahmed S.I. Extensively drug-resistant typhoid fever in Pakistan. Lancet Infect. Dis. 2019;19:242–243. doi: 10.1016/S1473-3099(19)30051-9. [DOI] [PubMed] [Google Scholar]
- 2.National Institute of Health Islamabad . National Action Plan; 2017. Antimicrobial Resistance.http://www.nih.org.pk/wp-content/uploads/2018/08/AMR-National-Action-Plan-Pakistan.pdf [Google Scholar]
- 3.Klemm E.J., et al. Emergence of an extensively drugresistant Salmonella enterica serovar Typhi clone harboring a promiscuous plasmid encoding resistance to fluoroquinolones and third-generation cephalosporins. mBio. 2018;9:e00105–e00118. doi: 10.1128/mBio.00105-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO E.M.R.O. Pakistan first country to introduce new typhoid vaccine into routine immunization programme. 2020. http://www.emro.who.int/pak/pakistan-news/pakistan-first-country-to-introduce-new-typhoid-vaccine-into-routine-immunization-programme.html
- 5.Antillón M., Warren J.L., Crawford F.W., Weinberger D.M., Kürüm E., Pak G.D., et al. The burden of typhoid fever in low- and middle-income countries: a meta-regression approach. PLoS Neglected Trop. Dis. 2017;11 doi: 10.1371/journal.pntd.0005376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention Extensively drug-resistant typhoid fever in Pakistan. 2019. https://wwwnc.cdc.gov/travel/notices/watch/xdr-typhoid-fever-pakistan#:%7E:text=The%20XDR%20strain%20of%20Salmonella,used%20to%20treat%20typhoid%20fever
- 7.National Institute of Health Islamabad Weekly field epidemiology report. 2020. https://www.nih.org.pk/wp-content/uploads/2020/03/07-FELTP-Pakistan-Weekly-Epidemiological-Report-Feb-03-Feb-09-2020.pdf
- 8.National Institute of Health Islamabad Weekly field epidemiology report. 2020. https://www.nih.org.pk/wp-content/uploads/2020/09/37-FELTP-Pakistan-Weekly-Epidemiological-Report-Sep-05-12-2020.pdf
- 9.Doan T., et al. Macrolide and nonmacrolide resistance with mass azithromycin distribution. N. Engl. J. Med. 2020;383:1941–1950. doi: 10.1056/NEJMoa2002606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mehmood K., Sundus A., Naqvi I.H., Ibrahim M.F., Siddique O., Ibrahim N.F. Typhidot - a blessing or a menace. Pakistan J. Med. Sci. 2015;31:439–443. doi: 10.12669/pjms.312.5934. [DOI] [PMC free article] [PubMed] [Google Scholar]