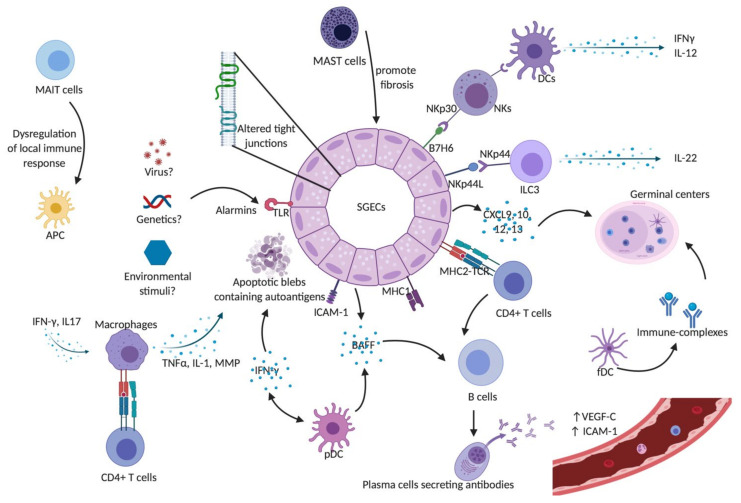
Figure 1.
Innate immunity in Sjögren’s syndrome. SGECs constitute the main target of auto-immunity in pSS, described as an autoimmune epithelitis. SGECs exhibit a subverted architecture mainly characterized by altered tight junctions. In genetic susceptible subjects, environmental stimuli such as viruses may trigger salivary gland epithelial cells (SGECs) through TLR activation. Activated SGECs secrete the BAFF that promotes activation and maturation of B cells. SGECs also produce chemokines such as CXCR9, 10, 11, and 12 that attract immune cells and contribute to the formation of germinal centers. Activated SGECs have the ability to act as non-professional antigen-presenting cells by expressing MHC-I, (HLA-ABC) and MHC-II (HLA-DR), adhesion molecules such as ICAM1 allowing them to activate T cells. TLR activation also contributes to SGEC apoptosis, releasing autoantigens that drive autoimmunity in pSS. Activated macrophages produce inflammatory cytokines such as IL-1, TNFα, and MMPs leading to epithelial cell damage. They can also act as antigenic peptide presenting cells through their MHC-II and interact with antigen-specific CD4+ T cells. pDCs lead to the production of type I IFN that acts through autocrine and paracrine circuits feeding a continuous reinforcing inflammatory loop. It also induces the production of BAFF, production contributing to the activation of B cells into plasma cells. fDCs play an essential part in the structure of ectopic germinal centers and retain on their surface immune-complexes, formed by antigen-antibody-complement. Mast cells contribute to the fibrosis and fatty infiltration of salivary glands (SGs). The aberrant phenotype of MAIT cells in pSS patients may lead to the dysregulation of the local immune responses, which would trigger local damage in SGs and auto-immunity. NK cells express the NKp30 receptor that is recognized by DCs and lead to the production of Th1 cytokines such as IFN-γ and IL-12. SGECs express B7-H6, the ligand for NKp30. Taken together, this may explain the hyperactivity of NK cells and the cross-talk with SGECs and DCs that lead to a subsequent activation of innate and adaptive immunity. A subset of ILC3 was found to be a major source of IL-22 in SGECs. Abbreviations: APC: Antigen presenting cells; BAFF: B-cell activating factor; CXCL9: C-X-C motif chemokine type 9; CXCL10: C-X-C motif chemokine type 10; CXCL12: C-X-C motif chemokine type 12; CXCL13: C-X-C motif chemokine type 13; DCs: dendritic cells; fDCs: follicular dendritic cells; ICAM-1: intercellular adhesion molecule 1; IFN-γ: interferon gamma; IL-: interleukin; ILC3: innate Lymphoid Cells type 3 MAIT: Mucosal-associated invariant T cells; MHC-I: major histocompatibility complex class I; MHC-II: major histocompatibility complex class II; MMPs: metalloproteases; NK: natural killer cells; NKp44L: NKp44 ligand; pDCs: plasmacytoid dendritic cells; SGECs: salivary glands epithelial cells; TCR: T cell receptor; TLR: Toll like receptor; TNFα: tumor necrosis factor alpha; VEGF-C: vascular endothelial growth factor C.