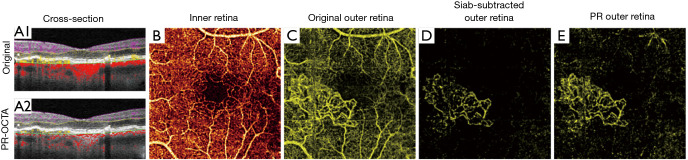
Figure 2.
Choroidal neovascularization as imaged by different methods for projection artifact removal. Cross-sections show flow signal (violet: inner retinal; yellow: outer retinal; red: choroidal flow) overlaid on structural optical coherence tomographic (OCT). (A1) original optical coherence tomographic angiography (OCTA) and (A2) projection-resolved OCTA (PR-OCTA). Artifactual tails that cause vessels to appear as vertical lines, rather than dots in cross-section, are clearly visible in the uncorrected image. (B) The superficial vascular complex slab. (C) Original OCTA angiogram of the outer retina. In a healthy eye, this slab is avascular, but choroidal neovascularization (CNV) is visible here, though heavily obscured by projection artifacts. The projection artifacts mimic the appearance of the superficial vasculature. (D) The same slab, after slab subtraction projection artifact removal. While the projection artifacts are removed, the vessels within the CNV lesion are disrupted, which may hinder some quantification. (E) The same slab viewed with PR-OCTA. While some residual projection artifacts are visible, the vessels in the CNV lesion remain continuous. Slab definitions are SVC: from the nerve fiber layer to 67% of the way through the ganglion cell layer and inner plexiform layer; ICP: from the bottom of the SVC to midway through the inner nuclear layer; DCP: from the bottom of the ICP through the outer plexiform layer; outer retina: from the bottom of the outer plexiform layer to Bruch’s membrane. Collectively the SVC, ICP, and DCP form the inner retina.