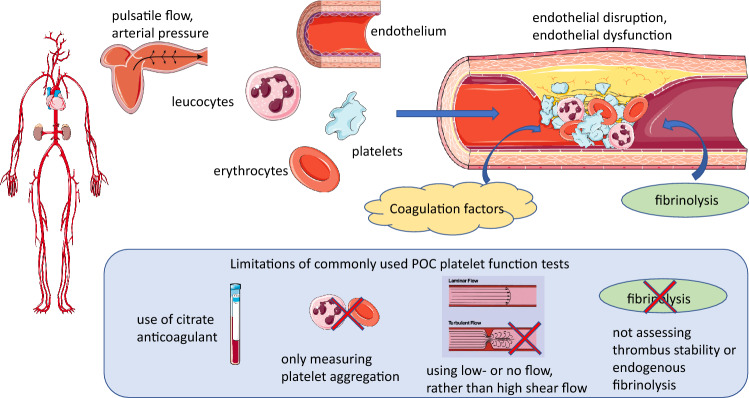
Fig. 1.
Main pathophysiological determinants of arterial thrombosis and limitations of current point-of-care (POC) platelet function tests. Arterial thrombosis under pathological conditions is driven by shear gradient-mediated platelet aggregation and activation of coagulation, resulting in an occlusive fibrin mesh, in which entrapped erythrocytes and leucocytes make important contributions to thrombus stability, as well as fibrinolysis. Rheological flow characteristics and effectiveness of endogenous fibrinolysis determine thrombus stability and lysis. Important limitations of many POC PFTs include (i) use of citrate-anticoagulated blood, which even after recalcification, may result in impaired platelet aggregation and thrombin generation from activated platelets, (ii) not assessing the contribution of erythrocytes, leucocytes and NETs, (iii) use of stagnant conditions or laminar blood flow and therefore not assessing the effect of high shear gradient on platelets and (iv) failing to assess the effect of endogenous thrombolysis