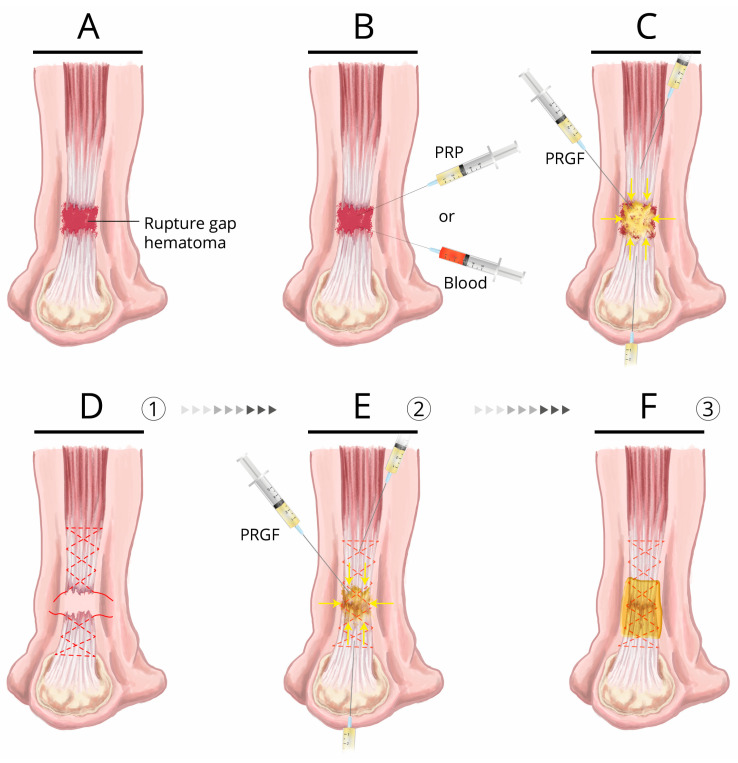
Figure 3.
Achilles tendon rupture treatment: conservative and surgical treatment assisted by autologous blood or blood-derived products (PRP). (A) Achilles tendon rupture, rupture gap, and hematoma. (B) Conservative treatment: a single injection of either PRP or autologous blood injected into the gap hematoma. (C) Conservative treatment proposal (in patients with a low functional demand, or for whom surgery is contraindicated). Ultrasound-guided injection of 4 mL of liquid plasma rich in growth factors (PRGF) in close proximity to the apparently healthy tendon tissue at each stump of the tendon and 4–6 mL of liquid PRGF into the gap hematoma; a procedure to be repeated over 2 or 3 consecutive weeks (D–F) Surgical treatment proposal: after the suture is performed with a non-reabsorbable suture material that has been bathed in liquid PRGF (D), 4–6 mL of liquid PRGF is injected in close proximity to the apparently healthy tendon tissue at each stump, as well as into the sutured area (E) within the time window of 10 to 15 min following PRGF activation with CaCl2. This window encompasses the time when the fibrin scaffold is still macroscopically liquid is but undergoing microscopic jellification. Liquid PRGF can extensively permeate through areas that surround the injection site and anchor to the collagen and other ECM proteins exposed in damaged tissue margins through the activated platelets conveyed by the fibrin clot, as a 3D fibrin–extracellular matrix-like malleable structure [17], thereby bridging the gap of injured areas. The time window of 1–5 min is the result of the gel point or clotting time, meaning the change from liquid to solid undergone by the matrix when 15–20% of the fibrinogen has been incorporated into the gel by branching points (approximately 4 min 50 s) [46]. After closing the paratenon and prior to closing the overlying skin, the peritendinous regions are also infiltrated with PRGF; finally, the entire affected area of the tendon is covered with a fibrin membrane of PRGF (F). As general recommendation, we suggest the use of 10 mL Luer lock-type syringes with 21G needles, since the use of small syringes means that large pressures are exerted on the ECM of the tissue during infiltration, thereby accounting for the focalized disruption of the ECM components (a desirable effect in some treatment protocols aimed at disrupting the neovascularization and neoinnervation present in some chronic tendinopathies) [7,42]. Upon infiltration, the needle should be oriented as closely as possible parallel to, and longitudinal with, the tendon fascicles for an optimal diffusion of PRGF [42].