Abstract
Purpose
The coronavirus disease 2019 (COVID-19) pandemic has had an immense impact on the healthcare industry. Oral and maxillofacial surgery (OMS) clinical practice uniquely exposes providers to COVID-19. The purpose of the present study was to understand the effect of the COVID-19 pandemic on OMS residency training programs (OMSRTPs): 1) training and education; 2) availability and use of personal protective equipment (PPE); 3) experience with, and use of, screening and viral testing; 4) resident experience; and 5) program director (PD) experience and observations of the immediate and future effects on OMSRTPs.
Materials and Methods
OMS residents and PDs in OMSRTPs in the United States were invited to participate in the present cross-sectional study from April 1, 2020 to May 1, 2020. A 51-question survey was used to evaluate the effects of COVID-19 on OMSRTPs and to assess the 5 specific aims of the present study.
Results
A total of 160 residents and 13 PDs participated in the survey, representing 83% of US states or territories with OMSRTPs. Almost all residents (96.5%) reported modifications to their training program, and 14% had been reassigned to off-service clinical rotations (eg, medicine, intensive care unit). The use of an N95 respirator mask plus standard PPE precautions during aerosol-generating procedures varied by procedure location, with 36.8% reporting limited access to these respirators. Widespread screening practices were in use, with 83.6% using laboratory-based viral testing. Residents scheduled to graduate in 2022 were most concerned with the completion of the graduation requirements and with decreased operative experience. Most residents (94.2%) had moved to web-based didactics, and a plurality (47%) had found increased value in the didactics.
Conclusions
Sweeping alterations to OMS clinical practice have occurred for those in OMSRTPs during the COVID-19 pandemic. Although the overall OMSRTP response has been favorable, residents' concerns regarding the ubiquitous availability of appropriate PPE, operative experience, and completion of graduation requirements requires further deliberation.
In late December 2019, coronavirus disease 2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus (SARS-CoV-2 [SC2]) virus emerged. In January 2020, it was reported that Washington State had the first reported case and death in the United States. However, new data have suggested that the virus was present in the United States as early as December 2019.1, 2, 3 The World Health Organization officially declared a pandemic due to SC2 on March 11, 2020.4 The disease has left no facet of humanity untouched; it has not only contributed to a colossal loss of life but has also, secondarily, brought turmoil to the financial markets around the globe.
The healthcare industry, in particular, has been overwhelmed by the effect of COVID-19 on healthcare resources. This has been underscored by providers concerned about emotional strain and physical exhaustion, access to personal protective equipment (PPE) and medical equipment, workplace exposure to COVID-19, disease transmission to family members, anxiety regarding the assumption of new or unfamiliar roles, and limited access to mental health services.5 While the pandemic has continued to evolve, the healthcare industry has had to adapt, understanding that the nature of certain specialties will predispose certain providers to elevated risk. Oral-maxillofacial surgery (OMS) is one such specialty whose physicians are uniquely at risk of exposure to SC2 owing to the proximity of providers managing disease in and around the oro- and nasopharynx. With organizations worldwide, including the Centers for Disease Control and Prevention, cautioning against the performance of aerosol-generating procedures (AGPs), concern has been growing among OMS residents, faculty, and staff.6 , 7
In the United States, we have 101 Commission on Dental Accreditation (CODA)–accredited OMS residency training programs (OMSRTPs), with ∼1165 current residents (2018 to 2019).8 Anecdotally, and in response to the suspension of elective surgery by institutions and local jurisdictions, OMSRTPs began to modify their education and training practices to ensure the safety of residents, faculty, and staff and still provide essential healthcare services.7 Many of these changes were instituted proactively by the programs themselves. Others were directed by the OMSRTP-sponsoring institution (eg, university, hospital, dental school) or healthcare systems or by imposed, local, regional, and/or federal regulations. These changes evolved organically, varying from program to program, and their extent has not been well characterized.
The purpose of the present study was to understand the effects of the COVID-19 pandemic on OMSRTPs. The specific aims were to 1) conduct a survey of OMS residents, program directors (PDs), and/or program chairs to identify the impact on and changes made to OMS residency training and education; 2) characterize the availability and use of PPE and airborne infection isolation rooms (AIIRs) in OMSRTPs; 3) understand the experience with, and use of, SC2 screening and testing practices for COVID-19 disease; 4) characterize the subjective experience of residents during the pandemic; and 5) characterize PDs' experience with and observations of the immediate and future effects on OMSRTPs.
Materials and Methods
We designed and implemented a cross-sectional study that included a 51-question survey designed to accomplish the 5 specific aims of the present study. The project was considered exempt by the University of Washington (UW) institutional review board [protocol no. 45 CFR 46.101(b)(2) or ID 00009980].
The 51-question survey included open- and closed-ended questions (Supplementary Appendix). A link to the survey was e-mailed by the American Association of Oral and Maxillofacial Surgeons (AAOMS) to all OMS faculty in a faculty newsletter distributed in April 2020. The survey link was also e-mailed to members of the American College of Oral and Maxillofacial Surgeons (ACOMS). The survey was addressed to current OMS residents, OMSRTP PDs, and/or program chairs who might also have been serving as a PD. The online survey was available for responses from April 1, 2020 to May 1, 2020. The results of the survey were anonymous.
The demographic variables were gender (male, female, other, decline to report), type of respondent (noncategorical resident, OMS certificate program resident, MD/OMS certificate program resident, or PD or program chair), type of residency training program (OMS certificate [single degree], or MD/OMS program [double degree]), level of training, and program location (city, state).
The primary variables included the responses to the survey questions (Supplementary Appendix) and were grouped into the following categories: 1) impact on and changes made to OMS residency training and education; 2) availability and use of PPE and AIIRs in OMSRTPs; 3) experience with, and use of, SC2 screening and testing practices for COVID-19; 4) resident experience; and 5) PD experience with and observations of the immediate and future effects on OMSRTPs.
An electronic survey host (Google Surveys) was used to generate a web-based platform for the responses, and the responses were retrieved from the online, electronic survey portal. A letter of invitation stated the study aims and measures, described the survey anonymity, and provided the option to opt out of any part of the survey. Furthermore, a free text response section was available at the end of the survey.
The responses were compiled, collated, and transferred to the Statistical Analysis Software package (SAS Institute, Inc, Cary, NC) for analysis using counts, percentages, cross-tabulations, and frequency reporting of the survey results. Because the responses to each question were optional, some variation occurred in the response rate for each survey question. Descriptive statistics were computed to provide an overview of the study sample.
Results
Demographics of Survey Respondents
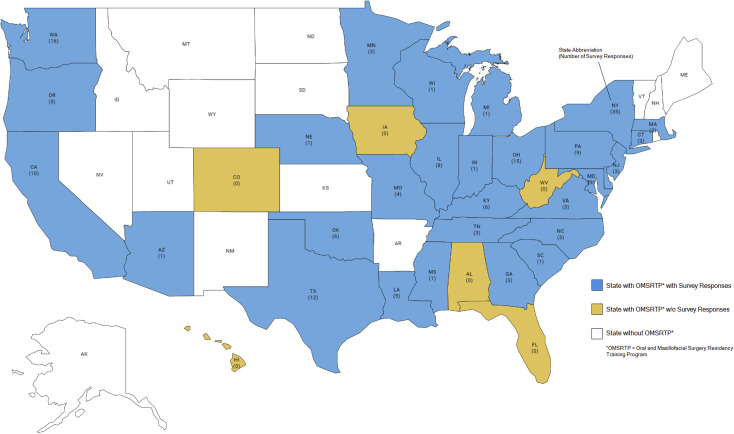
A total of 174 individuals completed the survey from April 1, 2020 to May 1, 2020, including 161 OMS residents and 13 OMS PDs or program chairs (Fig 1 ). The demographics of the survey participants are listed in Table 1 . Overall, the survey participants reflected the gender composition of the current OMS residents in the United States, with 78.2% identifying as male. The survey responses captured residents at each training level and type of program. Specifically, 80 residents were in OMS certificate programs (46.2%) and 73 were in MD/OMS certificate programs (42.2%). Geographically, the responses encompassed 30 of the 36 states, districts, and/or territories that have CODA-accredited OMSRTPs (Fig 2 ).9
Figure 1.
Map of states with oral and maxillofacial surgery residency training programs and number of survey responses stratified by state.
Table 1.
Demographics of Survey Respondents
| Characteristic | Respondents (n; %) |
|---|---|
| Overall | 174 (100) |
| Gender | |
| Male | 136 (78.2) |
| Female | 36 (20.7) |
| Other | 0 (0.0) |
| Declined to report | 2 (1.1) |
| Year in training | |
| PGY 1 | 25 (14.6) |
| PGY 2 | 21 (12.3) |
| PGY 3 | 38 (22.8) |
| PGY 4 | 43 (25.1) |
| PGY 5 | 18 (10.5) |
| PGY 6 | 14 (8.2) |
| Other | 11 (6.4) |
| Type of respondent | |
| Noncategorical resident | 7 (4.0) |
| OMS certificate program resident | 73 (42.2) |
| MD/OMS certificate program resident | 80 (46.2) |
| Program director/chair | 13 (7.5) |
| Enrollment in medical school | |
| Yes | 24 (17.9) |
| No | 110 (82.1) |
| Program location (states, districts, territories) | 29 (NA) |
Abbreviations: NA, not available; OMS, oral-maxillofacial surgery; PGY, postgraduate year.
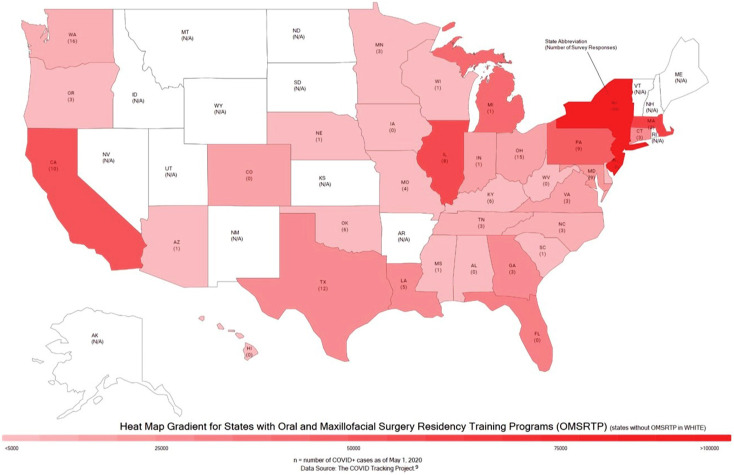
Figure 2.
Heat map of coronavirus disease 2019-positive cases in states with oral and maxillofacial surgery residency training programs, including the number of survey responses by stratified by state.
Data from https://covidtracking.com/data.9
The survey responses, categorized by the 5 aims they addressed, are presented in Table 2 and summarized below.
Table 2.
Survey Responses
| Survey Question | Respondents (n; %) |
|---|---|
| Effect on OMS residency training programs | |
| Resources for information | |
| AAOMS | 98 (57.3) |
| ADA | 60 (35.1) |
| UpToDate | 39 (22.8) |
| Institution | 133 (77.8) |
| State resources | 81 (47.4) |
| Department resources | 82 (48.0) |
| Other | 18 (10.7) |
| Have modifications been made to your training program? | |
| Yes | 167 (96.5) |
| No | 6 (3.5) |
| Changes to programs were directed by | |
| Department | 154 (90.6) |
| Institution | 149 (87.6) |
| State regulations | 135 (79.4) |
| Unknown | 8 (4.7) |
| Modifications to scheduling of elective cases | |
| Yes | 173 (100.0) |
| No | 0 (0.0) |
| Performance of elective cases | |
| Yes | 4 (2.3) |
| No | 168 (97.7) |
| Modifications to scheduling of urgent and emergent cases | |
| Yes | 143 (83.6) |
| No | 28 (16.4) |
| Changes to resident rotation assignments | |
| Yes | 117 (68.0) |
| No | 55 (32.0) |
| Assigned to off-service site | |
| Yes | 24 (14.0) |
| No | 148 (86.0) |
| Availability and use of PPE and AIIR | |
| Modifications to use of PPE | |
| Yes | 163 (95.3) |
| No | 8 (4.7) |
| Access to AIIR | |
| Yes | 70 (41.9) |
| No | 53 (31.7) |
| Do not know | 44 (26.3) |
| SC2 screening and testing practices for COVID-19 | |
| Screening patients for COVID-19 | 157 (95.7) |
| Screening procedures | |
| Signs and symptoms before arrival | 150 (95.5) |
| Preoperative COVID testing for surgical cases | 80 (51.0) |
| Other | 5 (3.2) |
| Performing laboratory-based SC2 testing | |
| Yes | 136 (83.6) |
| No | 27 (16.4) |
| Availability of test results | |
| >24 hours | 80 (54.1) |
| <24 hours | 68 (45.9) |
| Resident experience and perceptions | |
| Areas of resident concern | |
| Anesthesia cases | 25 (32.1) |
| Ambulatory anesthesia/deep sedation | 15 (43.6) |
| Off-service anesthesia | 34 (19.2) |
| Pathology | 20 (34.6) |
| Trauma | 27 (25.6) |
| Orthognathic surgery | 43 (55.1) |
| Reconstructive and cosmetic surgery | 33 (42.3) |
| Other | 11 (14.3) |
| Changes to didactics | |
| Yes | 133 (77.3) |
| No | 39 (22.7) |
| Current frequency of didactics | |
| Daily | 82 (55.0) |
| Weekly | 64 (43.0) |
| Monthly | 11 (7.4) |
| Change to frequency of didactics | |
| Increased | 124 (78.0) |
| Decreased | 35 (22.0) |
| Using virtual/online didactics | |
| Yes | 162 (94.2) |
| No | 10 (5.8) |
| Change to frequency of virtual/online didactics | |
| Increase | 77 (46.4) |
| Decrease | 27 (37.3) |
| No change | 62 (16.3) |
| Appropriate COVID-19 training by program | |
| Yes | 134 (81.2) |
| No | 31 (18.8) |
| Appropriate and adequate PPE, guidance, information provided by program | |
| Yes | 133 (79.6) |
| No | 34 (20.4) |
| Do you feel safe? | |
| Yes | 129 (76.3) |
| No | 40 (23.7) |
| Postponement or discontinuation of contract negotiations/discussions (all resident respondents) | |
| Yes | 16 (17.0) |
| No | 78 (83.0) |
| Postponement or discontinuation of contract negotiations/discussions (chief resident respondents) | |
| Yes | 11 (28.9) |
| No | 27 (71.1) |
| Program director experience | |
| Residents/faculty with COVID (n) | |
| 0 | 8 (80.0) |
| 1 | 1 (10.0) |
| 2 | 0 (0.0) |
| 3 | 1 (10.0) |
| Access to AIIR | |
| Yes | 7 (53.8) |
| No | 6 (46.2) |
| Conducting virtual didactics | |
| Yes | 13 (100.0) |
| No | 0 (0.0) |
| Change to referral patterns | |
| Increased | 0 (0.0) |
| Decreased | 7 (53.8) |
| No change | 2 (15.4) |
| Do not know | 4 (30.7) |
| Delay to onboarding | |
| Yes | 0 (0.0) |
| No | 10 (76.9) |
| Do not know | 3 (23.1) |
Abbreviations: AAOMS, American Association of Oral and Maxillofacial Surgeons; ADA, American Dental Association; AIIR, airborne infection isolation room; COVID-19, coronavirus disease 2019; PPE, personal protective equipment; SC2, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
Effect on OMS Residency Training and Education
Of the residents, PDs, and program chair respondents, 96.5% had experienced modifications to their training program in response to the pandemic. The respondents indicated that changes were primarily directed by the departments (90.6%), institutions (87.6%), and/or state regulations (79.4%). Additionally, 77.8% of the respondents indicated that they had used institutional resources for guidance on treating patients, with 57.3% using guidelines distributed by the AAOMS.
All the respondents indicated that their programs had made modifications to the scheduling of elective cases, with 97.7% stating their program had stopped performing elective cases altogether. Urgent or emergent cases were also affected, with 83.6% of respondents indicating that changes had been made to the scheduling of these cases.
Of the resident participants, 68% reported modifications to their rotations, with 14% stating that they had been assigned to an off-service site that they would not have otherwise been assigned to before the COVID pandemic. Those who had been reassigned included residents from programs located in Connecticut, Louisiana, Michigan, Missouri, New Jersey, New York, Ohio, and Washington. The reassigned respondents reported being deployed to a medicine or intensive care unit, or a backup call pool.
Availability and Use of PPE and AIIRs
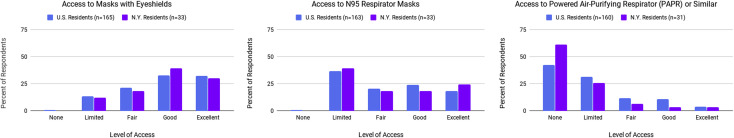
Regarding PPE, 95.3% of the respondents stated that their program had made modifications to PPE use. Most residents reported that their access to masks with eye shields was good (32.7%) or excellent (32.1%); however, 36.8% indicated that their access to N95 respirator masks was limited. Also, 42.5% of the respondents stated that they had no access to a powered air-purifying respirator (PAPR) or similar device. Although the overall distribution was similar, a larger percentage (61.2%) of respondents in New York reported no access to PPARs (Fig 3 ). Most respondents were using N95 respirator masks plus standard PPE precautions for AGPs in the clinic, operating room, and emergency department (72.7, 81.3, and 69.6%, respectively). Of the residents, 41.9% indicated that they had access to AIIRs, 31.7% reported no access to AIIRs, and 26.3% were unaware of such access. Access to PPE and AIIRs did not clearly follow a geographic distribution, and variation was found among residents at the same OMSRTPs.
Figure 3.
Access to personal protective equipment stratified by type showing a comparison of US oral-maxillofacial surgery (OMS) residents versus New York OMS residents.
SC2 Screening and Testing Practices for COVID-19
Almost all programs (95.7%) has been screening patients for COVID-19 symptoms. This was most frequently performed by hospital screening (65.2%) or front desk staff (62.2%). Of the respondents, 83.6% indicated that their program was using laboratory-based SC2 testing for patients, with 54.1% of respondents reporting that the tests required longer than 24 hours for a result.
Resident Experience and Perceptions
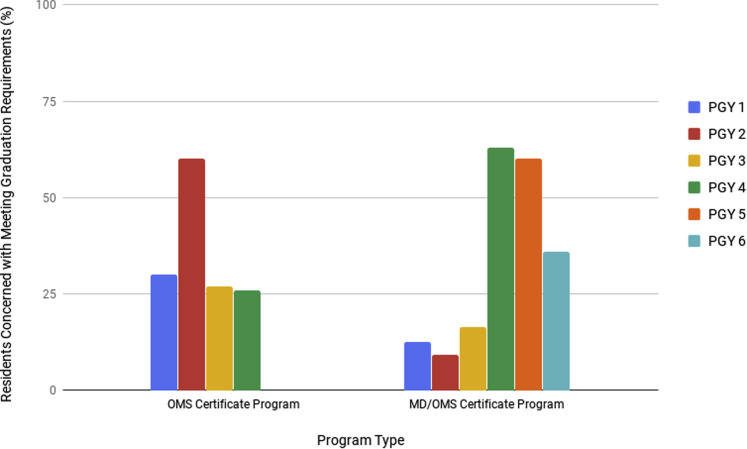
Resident training in both operative experience and didactic training practices has been altered. Most residents (66%) were not concerned with meeting the current CODA graduation requirements. Concern, however, was greatest for residents entering their second to last year of training (ie, those residents scheduled to graduate in June 2022), with 60% of these residents expressing concern (Fig 4 ). The residents were most concerned with orthognathic surgical experience (55.1%), experience with ambulatory anesthesia and deep sedation (43.6%), reconstructive and cosmetic surgery (42.3%), and overall anesthesia experience (32.1%). Most residents (88.8%) indicated that their operative experience had been affected, with an average decrease in operative experience of 67%.
Figure 4.
Percentage of residents concerned with meeting graduation requirements by stratified by program type and level of training. OMS, oral-maxillofacial surgery; PGY, postgraduate year.
Most respondents (94.2%) indicated that their program was using virtual (online) didactics and that the frequency of didactics, in general, had increased. A plurality of residents (46.4%) reported that virtual didactics were of increased value compared with their previous didactics. However, others reported decreased value (37.3%), and 16.3% reported no change in value of their didactics. Variations were found in the perceived value among residents of the same OMSRTP, and no clear association was found with geographic location.
Of all residents responding, 17% reported that contract negotiations or discussions regarding future employment after completion of their residency had been postponed or discontinued. This number was greatest for those residents currently in their last year of training (28.9%).
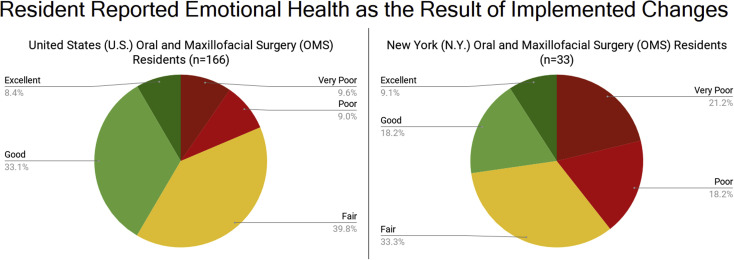
Regarding emotional health, most respondents (72.9%) believed that the changes implemented by their program were generally fair to good (Fig 5 ). Only 8.4% of residents reported that the changes made them feel excellent, and 9 and 9.6% reported that the changes made them feel poor or very poor, respectively. In contrast, a similar percentage of residents from New York reported that the program changes had an excellent effect on their emotional health (9.1%), with 51.5% reporting that the changes made them feel fair to good, and 18.2 and 21.1% reporting that the changes made them feel poor and very poor, respectively (Fig 5). Of the respondents, 81.2% stated that their institution had implemented appropriate training in response to the pandemic. The changes implemented by programs to limit exposure to residents was measured, with most respondents (76.3%) reporting that they believed they were “safe” at their program.
Figure 5.
Resident reported emotional health resulting from implemented changes. Comparison of US oral-maxillofacial surgery (OMS) residents versus New York OMS residents.
Of the respondents, 46 provided free-text comments at the end of the survey. These comments have been summarized using the following statements: concern regarding limited training and clinical and operative experience; concern regarding occupational exposure to residents and transmission to, or exposure of, family members; access for residents to PPE and viral and/or serologic testing should be paramount; and concern regarding the ability to meet graduation requirements.
PD Experience and Assessment of Immediate and Future Effects on OMSRTPs
A total of 13 residency PDs from 11 states responded to the survey. They reported an average of 0.33 resident or faculty testing positive for COVID-19 per program (range, 0 to 3 residents). Of the respondents, 53.8% reported that their facility had access to AIIRs. All the respondents indicated that their programs were using online virtual didactics. Of the PDs, 66% indicated that a resident had left or missed duty hours because of flu-like symptoms, which might or might not have been COVID-19, and 33% reported that a resident had left or missed duty hours because of exposure or potential exposure. The PDs also reported that faculty had left or missed work hours because they were unwilling to treat patients because of potential exposure (22%), unable to treat patients because of previous or potential exposure (33%), were considered “high risk” by their age (>60 years; 44%), or had a preexisting condition that prohibited them from treating patients (22%). Also, 53% of PDs reported that their outside referrals had decreased, 15% reported no change, and 30% reported not knowing whether their referral patterns had changed.
Regarding the future impact on OMSRTPs, 76% of the PDs responded that their institution was not delaying onboarding for incoming July 2020 first-year residents, with 24% unsure. Also, 46% of PDs indicated that incoming July 2020 first-year residents had expressed concern about state board licensing and 38% had expressed concern about dental school graduation requirements. The free-text responses by the PDs showed concern for faculty and residents becoming sick, the risk associated with placing residents in the “line-of-duty,” and future employment prospects for graduating residents.
Discussion
The COVID-19 pandemic has resulted in tremendous morbidity and mortality. The impact to the healthcare system and its providers has been immense. OMS is one healthcare specialty with unique exposure that contributes to an elevated risk for its providers. The purpose of the present study was to understand the effects of the COVID-19 pandemic on OMS residency training. We queried residents, PDs, and department chairs who hold joint PD responsibilities in OMSRTPs. We aimed to identify the changes made to OMS residency training, characterize the availability and use of PPE and AIIRs in OMSRTPs, and determine the experience with, and use of, SC2 screening and testing practices for COVID-19. In addition, we asked residents to characterize their experience and PDs to opine on the immediate and future impact on OMSRTPs.
The respondents to our survey were a representative sample of OMS residents in the United States when stratified by gender, level of training, type of training program, and geographic location. Although only 13 PDs responded to the survey, their responses represented 31% of the states, districts, and territories with CODA-accredited OMSRTPs. We suspect that the low PD response rate was the result of unclear instructions. The PDs were encouraged to pass the survey on to their residents but were also invited to provide their observations. Given the current demands on PDs, the instructions could easily have been missed in the e-mail verbiage regarding the survey.
All OMSRTPs have had to make alterations, and these changes were influenced by a variety of factors (ie, departmental, institutional, and/or state regulations). Most residents turned to institutional guidelines when treating patients; however, 57% used the guidelines set forth by the AAOMS. Residents have immediate access to numerous web-based data resources via mobile smart telephones; however, almost 60% turned to their national organization. The pandemic has demonstrated the need for national organizations to keep their members up-to-date and informed, as AAOMS has been striving to do.
The responses to the present survey have shown that residents' experience has also been affected. Almost all respondents (96.5%) indicated that their program had discontinued elective surgery, and most residents (68%) had experienced modifications to their rotations. As a result, residents expressed a high level of concern regarding meeting graduation requirements, specifically those entering their second to last year of training and those scheduled to graduate in June 2022. The residents were most concerned with losing experience in the areas of anesthesia, orthognathic surgery, and reconstructive and cosmetic surgery. These findings were not surprising. Most outpatient anesthesia and orthognathic, reconstructive, and cosmetic surgery is elective; these procedures were among those suspended during this crisis because of concerns of performing AGPs and the limited access to PPE.7 During an OMS certificate program, many off-service rotations will be completed during the second year of training. Also, in a combined MD/OMS certificate program, anesthesia rotations are often assigned at the end of, or during, the medical school rotations. Therefore, the responses of the graduating class of 2022 were not surprising.
AAOMS and CODA have been working closely during this pandemic to provide temporary modifications to educational requirements for the graduating class of 2020. Temporary guidance was released to all programs in April 2020.10 , 11 However, the group of residents expressing the most concern regarding graduation was the class of 2022, and the graduation requirements for those scheduled to graduate after 2020 have not yet been formally discussed. Ongoing reassessment regarding the graduation requirements will be essential in the coming months and years. Furthermore, adjustments (eg, scheduling of operative cases, scheduled duty hours, rotation assignments, and scheduling of didactics) should be made, wherever possible, in the preexisting timeline of the individual OMSRTP to ensure that every resident will be able to meet the competency requirements in all areas of OMS practice. Nonetheless, as the COVID-19 pandemic continues to evolve, the future remains very unclear.
With a decrease in operative experience, a concurrent increase in didactic training and in the utilization of virtual didactics has occurred. In addition to the didactic training performed at each individual program, several programs and organizations have offered free didactic opportunities to residents during the pandemic, including University of Pennsylvania Dental Medicine, the Collaborative OMS Virtual Interinstitutional Didactic (COVID) Program, AAOMS, ACOMS, and Arbeitsgemeinschaft für Osteosynthesefragen Craniomaxillofacial (AOCMF), among others. The almost universal transition to virtual didactics was viewed positively by a significant number of residents. On further examination, however, variability in the perceived value of didactics was present for residents within the same OMSRTP. This was also not surprising, given that individual learning styles differ. Although “flipped classrooms” for maxillofacial surgery training have been discussed previously, further research is required regarding virtual learning.12 , 13
One startling finding from our survey was the potential for long-term harm to OMS residents. Almost 1 in 3 graduating residents have had alterations to their postgraduation plans, specifically the postponement or discontinuation of contract negotiations or discussions regarding future employment after completion of their residency. Relevant to this realization is the existing burden of student loan debt, the type of practice setting residents chose to pursue, and the decision for residents to continue residency training or pursue fellowship training. Furthermore, it is unclear whether and when the public will be ready to resume elective surgical cases, which could also affect the earning potential of future graduates. Finally, it is unclear how much of the financial burden oral and maxillofacial surgeons will be required to bear to provide adequate protection to those in their practice.
In response to the COVID pandemic, almost all programs have made modifications to the use of PPE. Although the overall distribution of PPE was similar, a larger number of residents in New York reported they did not have access to PPARs. This was not surprising, because New York was not only the COVID-19 epicenter of the United States, but also of the world, and access to PPARs could be expected to be critically low. Of more concern was the residents' assessment of their access to N95 respirator masks, because 36.8% reported they had limited access to these. Furthermore, 1 in 4 residents were unaware whether their program had access to AIIRs or negative-pressure isolation rooms in their facility. No clear geographic association was found, and even residents from within the same program reported varying levels of access to PPE and AIIRs. The latter was not surprising, because many programs have clinical rotations across multiple clinical training sites, and access could differ at each site. Regardless, institutions should provide adequate access to PPE and AIIRs, and PDs should provide guidance on their proper use for each type of clinical situation that might be encountered. In institutions in which access to AIIRs is a shared resource, one should consider access according to the acuity of the clinical problem and/or the results of viral or serologic testing.7 In practice, this will vary widely. At the University of Washington, 3 factors are evaluated to determine the level of PPE required and to ensure provider, patient, and staff safety: 1) acuity of the procedure (emergent or urgent); 2) symptom status; and 3) SC2 test results. All preoperative patients are tested and, if positive, treatment is delayed, unless emergent. Emergent SC2-positive patients are treated in the hospital's main operating rooms with AIIRs and full PPE (PAPR or N95, eye shield or goggles, gown, gloves, surgical cap), with trained observers for the donning and doffing procedures.7
Almost all residents (95.7%) indicated that their program was screening patients for symptoms of COVID-19. Unclear, however, was at what point this screening was performed at each institution. Panesar et al,7 in their discussion on the evolution of the guidelines for OMS patient care at their institution, recommended contacting patients before their clinic visit to ensure the patients were symptom free and discussing any symptoms during their visit and again 1 week after their visit to ensure that asymptomatic patients had not developed symptoms. We recommend that all OMSRTPs consider implementing similar guidelines.
Most respondents (83.6%) were using laboratory-based testing for patients, with 54.1% indicating that the testing required more than 24 hours for the results to be available. However, variability was found among residents at the same program. Again, this was not surprising. OMSRTPs have clinical rotations across multiple in- and outpatient clinical facilities. Future universal access to testing and decreased time for the test results to return should lead to more ubiquitous testing of patients. Furthermore, residents expressed concern regarding access to viral and serologic testing for providers. Moving forward, programs should continue to reassess the value of viral and serologic testing for patients and providers involved in OMS practice in the context of local and regional availability. At the UW, serological testing has been expanded to all UW Medicine employees as of April 28, 2020.14
Residency programs have done well in implementing changes that will ensure the safeguarding of their residents' physical and emotional states. Most residents (81.2%) reported that their institution had implemented appropriate training in response to the pandemic, and a similar number (79.6%) stated they felt safe at their institutions. However, those residents who reported not feeling safe included residents from 15 of the 30 states represented in our survey. The survey results were instructive to us; despite all preparations and discussions, e-mail updates, and virtual meetings, our residents (UW) were among those reporting anxiety and uncertainty about COVID-19. Perhaps the safety issues cannot be fully addressed; however, programs should continue to ensure resident understanding of their institutions' response based on the need to provide a safe workplace in this evolving process.
To decrease the potential exposure to residents and faculty, PDs made alterations to their didactic training by using virtual didactics and to their clinical training by discontinuing elective operations. Although the prevalence of COVID-19 was low among residents and faculty (according to PD knowledge), two thirds of the OMSRTPs had a resident miss duty hours because of flu-like symptoms, and one third of the PDs reported the loss of residency hours owing to exposure or potential exposure. The residency PDs largely shared the concerns of their residents; understanding the uncertainty in employment prospects for graduating residents and the high concern for placing residents and faculty in situations that could expose them to harm. Finally, given the frequency of OMSRTP faculty who missed clinical activity, the availability of supervised clinical training could have been negatively affected.
The limitations of the present study included the sample size, evolving nature of the pandemic and our understanding of it, and evolving response by the OMSRTPs. Although our survey sample included only 174 respondents, the responses represented data from 30 of the 36 states, district, and/or territories (83%) with CODA-accredited OMSRTPs and provided a representative sample of residents in OMSRTPs. The survey did not receive responses from individuals in Alabama, Colorado, Florida, Iowa, West Virginia, or Hawaii. These states combined only encompass 9 of the 101 CODA-accredited programs. Furthermore, the denominator of individuals who received the survey is unclear given the method of distribution. Although we aimed to provide an assessment of the early effects of COVID-19 on OMSRTPs, the pandemic is rapidly evolving. The identification, testing, management, guidance, and regulations have undergone tremendous changes even during the period during which our survey was available. However, in the scheme of the pandemic, the results from our study will provide a baseline understanding to the specialty and to future researchers and will enable us to become more adaptive at addressing future outbreaks.
In conclusion, because we currently find ourselves in the midst of an evolving situation, it is important to reflect on the quick changes that have been made, the challenges we face, and the positive results that have been achieved. Programs have taken steps to decrease exposure by transitioning to virtual didactics and by decreasing the number of elective cases. Because of the decreased caseload, residents have become concerned about meeting their graduation requirements. This emphasizes the need for CODA and AAOMS to review the program requirements for the upcoming years. Among residents, we found a perception of lack of PPE access. Although most residents reported feeling safe, we still found a number who reported feelings of anxiety and apprehension. PDs have understood and largely shared the concerns of their residents. Moving forward, it will be important to systematically study the effects of the changes on both residents and program training. The lessons learned and changes implemented are likely to forever change our clinical practices. Finally, at the time of submission, 1,360,705 cases of COVID-19 in the United States and 4,256,991 cases around the world had been reported.9 , 15 The pandemic has contributed to 82,340 deaths in the United States and 291,487deaths around the world.15
Acknowledgments
Thank you to all the healthcare and essential workers and, in particular, to the OMS residents, staff, and faculty in the United States and around the world, who have continued to work selflessly, in some cases without proper PPE, to ensure the well-being and survival of their patients. The authors would like to thank Thomas B. Dodson, Andrea B. Burke, and Melanie Lang for their contributions developing the survey used in the present study. Finally, the authors would like to thank the AAOMS and ACOMS for their assistance in the delivery of the survey to their members.
Footnotes
The present study was supported in part by the Department of Oral and Maxillofacial Surgery’s Laboratory for Applied Clinical Research Fund.
Conflict of Interest Disclosures: Dr. Jasjit K. Dillon is the recipient of an Oral and Maxillofacial Surgery Foundation and Osteo Science Foundation grant. All other authors do not have any relevant financial relationship(s) with a commercial interest.
Supplementary data associated with this article can be found in the online version, at https://doi.org/10.1016/j.joms.2020.05.026.
Supplementary Data
A 51-Question Survey regarding the Early Effect of COVID-19 on OMSRTP.
References
- 1.Holshue M.L., DeBolt C., Lindquist S. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Washington State Report First COVID-19 Death. CDC Online Newsroom. https://www.cdc.gov/media/releases/2020/s0229-COVID-19-first-death.html Available at:
- 3.Van Dorp L., Acman M., Richard D. Emergence of genomic diversity and recurrent mutations in SARS-CoV-2. Infect Genet Evol. 2020;83:104351. doi: 10.1016/j.meegid.2020.104351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization WHO Director-General's opening remarks at the media briefing on COVID-19 – 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 Available at:
- 5.Ayanian J.Z. Editor’s comment: Mental health needs of health care workers providing frontline COVID-19 care. JAMA Health Forum. https://jamanetwork.com/channels/health-forum/fullarticle/2764228 Available at: [DOI] [PubMed]
- 6.Centers for Disease Control and Prevention Healthcare Infection Prevention and Control FAQs for COVID-19. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-faq.html Available at:
- 7.Panesar K., Dodson T.B., Lynch J. Evolution of COVID-19 guidelines for University of Washington oral and maxillofacial surgery patient care. https://doi.org/10.1016/j.joms.2020.04.034 [e-pub ahead of print]. J Oral Maxillofac Surg. [DOI] [PMC free article] [PubMed]
- 8.American Association of Oral and Maxillofacial Surgeons 2018-2019 OMS Program, Resident and Faculty Summary Report. https://www.aaoms.org/docs/education_research/edu_training/aaoms_faculty_resident_summary.pdf Available at:
- 9.The COVID Tracking Project Most Recent Data. https://covidtracking.com/data Available at:
- 10.Commission on Dental Accreditation Additional Post-CODA Meeting Guidance on Interruption of Education Related to COVID-19 for the Class of 2020 (April 14, 2020) https://www.ada.org/∼/media/CODA/Files/COVID19_Guidance_InterruptionofEducation_Class2020.pdf?la=en Available at:
- 11.Commission on Dental Accreditation Guidance Document: Temporary Flexibility in Accreditation Standards to Address Interruption of Education Reporting Requirements Resulting from COVID-19 for the Class of 2020. https://www.ada.org/∼/media/CODA/Files/OMS_Flexibility_4_20.pdf?la=en Available at:
- 12.Elledge R., Houlton S., Hackett S. “Flipped classrooms” in training in maxillofacial surgery: Preparation before the traditional didactic lecture? Br J Oral Maxillofac Surg. 2018;56:384. doi: 10.1016/j.bjoms.2018.04.006. [DOI] [PubMed] [Google Scholar]
- 13.Carlson E.R. COVID-19 and educational engagement. J Oral Maxillofac Surg. 2019 doi: 10.1016/j.joms.2020.04.033. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.University of Washington Medicine The Huddle. Dr. John Lynch: Announcing Antibody Testing for Employees. https://huddle.uwmedicine.org/news/dr-john-lynch-announcing-antibody-testing-employees Available at:
- 15.Johns Hopkins Coronavirus Resource Center COVID-19 Map. https://coronavirus.jhu.edu/map.html Available at:
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A 51-Question Survey regarding the Early Effect of COVID-19 on OMSRTP.