Abstract
The COVID-19 pandemic has presented novel challenges for the entire health-care continuum, requiring transformative changes to hospital and post-acute care, including clinical, administrative, and physical modifications to current standards of operations. Innovative use and adaptation of long-term acute care hospitals (LTACHs) can safely and effectively care for patients during the ongoing COVID-19 pandemic. A framework for the rapid changes, including increasing collaboration with external health-care organizations, creating new methods for enhanced communication, and modifying processes focused on patient safety and clinical outcomes, is described for a network of 94 LTACHs. When managed and modified correctly, LTACHs can play a vital role in managing the national health-care pandemic crisis.
Key Words: critical care, health-care utilization, mechanical ventilation
Abbreviations: LTACH, long-term acute care hospital; MV, mechanical ventilation; PPE, personal protective equipment; RE, resilience engineering; VOH, virtual operational huddle
A major threat of SARS-CoV-2 is that hospitals have experienced a dramatic surge in laboratory-confirmed COVID-19 cases and have reached ICU bed or ventilator utilization capacity.1 , 2 Analysts in health policy and systems research have recently indicated that long-term acute care hospitals (LTACHs) could provide a significant resource to increase the capacity of care venues able to treat patients with both active and downstream sequelae of COVID-19.3 LTACHs are specialized hospitals that provide prolonged acute and intensive care for patients with chronic or persistent critical illness, while focusing on patient recovery and return to a functional life.4 Because LTACH care “focuses on continued medical stabilization, management of critical infusions, optimizing respiratory status, and facilitation of functional recovery,”2 it has led a number of physician-researchers to conclude that the LTACH clinical setting is conducive to the ongoing treatment of patients with COVID-19 who require hospitalization and post-acute care.
Approximately 16% of hospitalized COVID-19 patients require treatment in the ICU;5 , 6 many of these patients also require mechanical ventilation (MV). Care for MV patients is a primary specialization in LTACHs, which have experienced critical care clinicians and respiratory therapists in an accredited acute care hospital setting.7 Patients with COVID-19 can develop post-ICU syndrome8, 9, 10, 11 or chronic critical illness that requires more intensive and prolonged hospitalization, as well as specialized interventions.12
Although LTACH staff have the skills necessary for treatment of COVID-19 patients, extensive preparations and transformations are required for treating patients with a highly virulent virus. Many of the changes required to adequately and safely treat potentially infectious patients are similar to adaptations made by traditional hospitals.13 , 14 However, additional clinical, operational, and environmental changes are required for LTACHs to treat COVID-19 patients because of the extended time required for patient recovery while limiting virus transmissibility.15 The following is a description of the preparation and rapid dissemination and implementation of changes to a distributed, nationwide network of 94 LTACHs in response to the COVID-19 pandemic. Many of the operational changes and strategies presented here may aid other LTACHs and health systems in adapting for the treatment of critically ill patients during surge periods.
Setting
The network of 94 LTACHs considered here spans 27 states yet shares a similar operating model, with central management by the parent organization.16 Network LTACHs provide intensive, prolonged hospital-level care, including 24-hour nursing and respiratory therapy services, staffing ratios commensurate with patient acuity, and ancillary services such as physical, occupational, and speech-language rehabilitation. Most LTACH patients are referred from an ICU where they have been treated for at least 3 days, the primary admission criterion used by Centers for Medicare & Medicaid Services.17 LTACHs facilitate recovery from critical illnesses through specific processes designed to improve functional recovery, providing more extensive services than skilled nursing facilities or inpatient rehabilitation hospitals, which serve patients of lesser acuity and different treatment requirements. Unlike skilled nursing facilities and inpatient rehabilitation hospitals, LTACHs are licensed, accredited, and certified as acute care hospitals, with comparable acute medical/surgical floors, telemetry, and ICU capability. LTACHs provide evidence-based strategies for liberation from prolonged mechanical ventilation that emphasize reducing adverse ventilator-associated events, including pneumonia and infection, while ensuring personal nutrition needs.18 , 19 The multidisciplinary approach of LTACHs includes intensivists, nurses, respiratory therapists, physical therapists, pharmacists, dietitians, subspecialist physicians, and case managers.20
Pandemic-Related Modifications
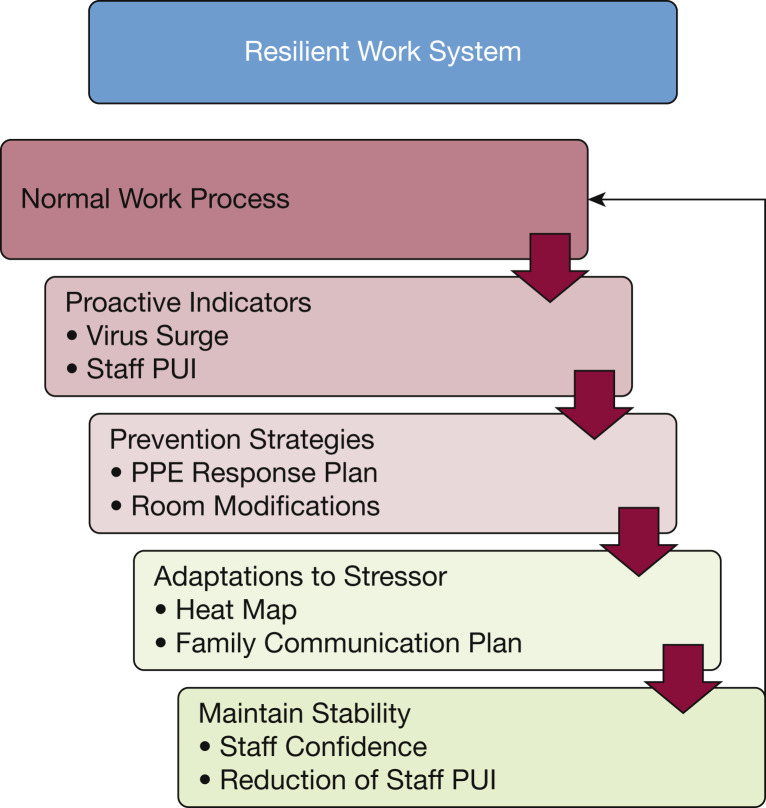
Transforming an LTACH hospital or hospital system into an effective and efficient operation to treat patients during a pandemic requires new pathways for enhanced communication, increased collaboration with external health-care organizations, and modification of processes that are focused on patient safety and clinical outcomes. Typically, health-care process improvements occur through redesigning, managing constraints and resources in parallel, eliminating redundant steps, and synchronizing tasks,21 which was demonstrated by the University of Washington Medicine’s Post-Acute Care Network health system’s three-phased approach in response to the COVID-19 pandemic.22 Many of the changes made in response to the pandemic may become standard practice.23 With the urgency of a health system-wide COVID-19 response, institutions benefit from resilience engineering (RE), or the rapid development of processes specifically designed to respond to changes. RE is associated with the ability of an organization to recover quickly to a stable state, allowing it to continue operations during and after the presence of significant stresses (Fig 1 ).24, 25, 26, 27 After examining our normal work processes, three levels of modifications using RE were made to our LTACHs, depending on their location and responsiveness to the needs of regional hospitals: (1) transforming LTACHs into a COVID-19 treatment center; (2) preparing LTACHs to admit and treat COVID-19 recovery patients; and 3) preparing LTACHs to treat non-COVID-19 ICU overflow patients. Many of these additional processes were similar to those developed by traditional hospitals in response to the pandemic but required personalization and further adaptation to fit into the LTACH workflow, to provide treatment for COVID-19 patients and those recovering from the consequences of COVID-19 infection.
Figure 1.
Resilient work system flow chart, highlighting system changes as a response to the COVID-19 pandemic and patient needs. Components of a resilient work system include characterization of normal work processes, development of proactive indicators and prevention strategies, which lead to adaptations to stressors, resulting in maintenance of stability. Successful process changes become part of normal work processes, completing the cycle. PPE = personal protective equipment; PUI = patients under investigation.
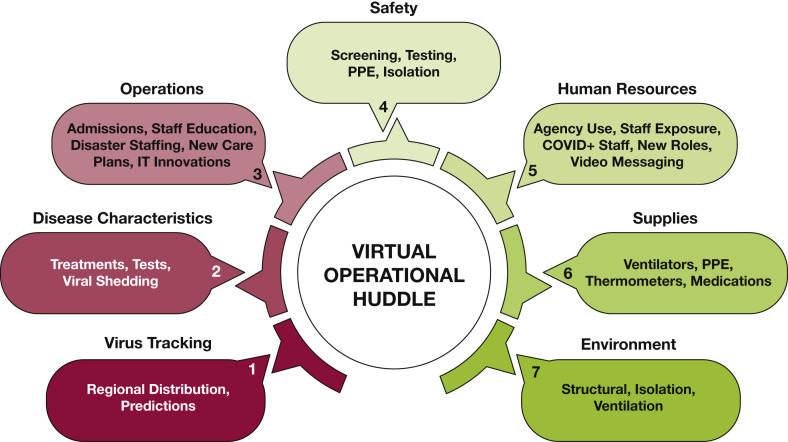
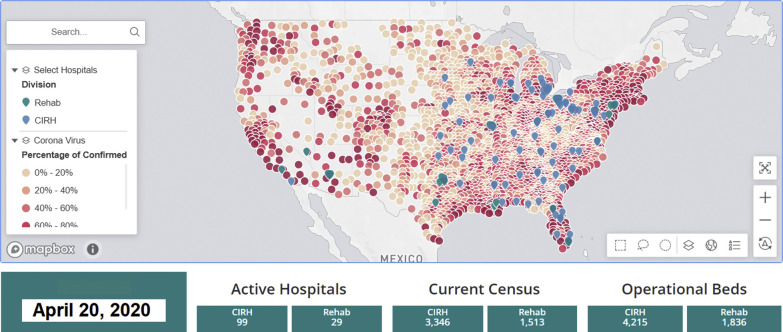
An ongoing awareness of the status of a system is important for designing resilient processes.28 As such, a vital component of our LTACH’s resilient work system was a central hub communication network, similar in concept to clinical daily huddles and rounds shown to be effective in providing quality patient care, but controlled centrally through the conveyance of essential information in an emergency management and incident command center design.29, 30, 31 Our version of the central hub, called the virtual operational huddle (VOH), began on March 3, 2020, and served as a real-time review of the current status of hospital operations throughout the network (Fig 2 ). The VOH included daily communication with more than 100 executive and regional senior leaders and staff in support of critical functions in hospital operations, including clinical, administrative, human resources, supply and logistics, legal, compliance, and quality. Each VOH started with a summary of COVID-19 incidence by region, with emphasis on county locations near LTACHs in the network. We developed a heat map application based on data from the Johns Hopkins COVID Dashboard (Fig 3 ).32 Each regional leader in the network shared the heat map results with individual LTACH administrators, who communicated with local acute care hospitals to more effectively assist them in responding to surges of COVID-19 patients.
Figure 2.
Schematic of the virtual operational huddle, a central hub used at all network long-term acute care hospitals. Components of the virtual operational huddle include leadership updates, discussions of all major issues, and opportunities for improvement encountered in each department and segment related to hospital operations. PPE = personal protective equipment.
Figure 3.
COVID-19 heat map, adapted for use during the virtual operational huddle to allow LTACHs to be more responsive to regional needs. COVID-19 heat map with LTACH locations shown in blue COVID-19 data from Johns Hopkins29 was downloaded, and COVID-19 cases in counties surrounding LTACH network hospital locations were incorporated into a US map. CIRH = Critical Illness Recovery Hospital; LTACH = long-term acute-care hospital.
Resilient work systems must be flexible enough to manage and not merely reduce variability, especially with rapidly evolving COVID-19 information and care recommendations. After a VOH review of potential surge locations, we provided an updated clinical review of COVID-19 infections and potential treatments and therapies, together with a review of the most current literature, current US clinical trials, and an epidemiological review of infection and mortality projection models, augmented by an infectious disease physician specialist. This up-to-date information allowed LTACH staff to effectively make preparations to treat COVID-19 recovery patients and, if necessary, treat those with active infection.
During the VOH, success and opportunities of operational changes included the development of updated procedures and timing for screening COVID-19 infection, the effective use of personal protective equipment (PPE) (with a buddy system to ensure adequate protection), additional precautionary hygiene practices, and a review of available resources. We developed contingency plans to account for staff quarantine or prolonged illness, to maintain staffing ratios for treating COVID-19 recovery patients and non-COVID-19 ICU overflow patients. A 2% increase in staff-to-patient ratios was necessary in several LTACHs to maintain the necessary level of services. We established a dedicated COVID-19 e-mail box to triage and address all questions from LTACH staff, along with Frequently Asked Questions documents and all-employee messaging via a dedicated network portal site, to keep everyone abreast of updated guidelines for PPE, testing, and self-quarantine procedures after exposure.
Modifications for treating COVID-19 patients, which were polymerase chain reaction laboratory-confirmed COVID-19 positive through nasal swabs, also included physical and environmental changes throughout the LTACH network. Proper ventilation systems were constructed together with structural changes to facilitate clinical activities for the COVID-19 patients. Supply requirements were determined centrally with backup plans for all LTACHs and triage plans for equipment redistribution if needed. A daily PPE tracking tool was developed, together with tracking the location of ventilators that could be sent across the country to LTACHs in need. In addition to higher staffing ratios to limit the spread of infection, we experienced a higher rate structure for employees and agency staff to work in the COVID-19 environment, increased supplies (eg, PPE), additional transfer costs to move equipment such as ventilators to regions with higher COVID-19 outbreaks, and costs associated with COVID-19 tests. Overall, additional expense related to the COVID-19 pandemic represents approximately 2% to 3% of our total operating expenses for the year. Individual LTACHs may experience different expense increases, depending on the geographic region and the degree of pandemic impact.
Local ICU capacity and projected needs dictated the type of LTACH response to accepting COVID-19 patients. A total of 992 adult (≥18 years) COVID-19-positive patients were admitted to 94 LTACHs from March through May 2020 (Table 1 ), with a dramatic 53% increase in the proportion of COVID-19 patients from April to May. In situations in which ICU beds were filled with an overwhelming increase in community infections, the aforementioned infrastructure changes allowed LTACHs to be transformed into acute care COVID-19 hospitals. Most of our LTACHs were already equipped to treat patients directly from the ICU; enhanced infection precautions were made at these locations to minimize the chance of horizontal transmission of the COVID-19 virus. Many COVID-19 patients were mechanically ventilated on arrival to the LTACH setting (48.1%) (Table 1). In regions of lower COVID-19 case volume, our LTACHs adapted to the more complex course of the prolonged COVID-19 patient population. COVID-19 patients stayed, on average, 26.7 days in the LTACH. Recovery support programs such as physical therapy, occupational therapy, and respiratory therapy were modified for COVID-19 patients, with the addition of a more structured cognitive therapy rehabilitation program. For example, an increased frequency of therapy treatments with reduced durations were made because of COVID-19 patients’ advanced deconditioned status and low endurance level, allowing for longer recovery time between sessions. More than 20% of COVID-19 patients recovered sufficiently to be discharged home (n = 212), whereas others required ongoing treatment at a lower-level-of-care facility (n = 524; 53%) (Table 1).
Table 1.
Characteristics of Patients With COVID-19 Treated in 94 LTACHs Admitted March Through May 2020
| Characteristic | Patients With COVID-19 n = 992 (13.2%) | Non-COVID-19 Patients n = 6,497 (86.8%) | Measure of Associationa |
|---|---|---|---|
| Demographics | |||
| Age, mean (SD) | 64.1 (13.0) | 64.7 (14.0) | 0.01b |
| Female, No. (%) | 439 (44.3) | 2,845 (43.8) | −0.01c,d |
| Race, No. (%) | 0.01c,e | ||
| Asian | 13 (1.3) | 40 (0.6) | |
| Black | 302 (30.4) | 1,232 (19.0) | |
| White | 572 (57.7) | 4,673 (71.9) | |
| Other | 105 (10.6) | 552 (8.5) | |
| LTACH Region, No. (%)f | 0.01c,e | ||
| East North Central | 488 (49.2) | 1,875 (28.9) | |
| South Atlantic | 196 (19.8) | 1,758 (27.1) | |
| Middle Atlantic | 116 (11.7) | 577 (8.9) | |
| East South Central | 64 (6.5) | 834 (12.8) | |
| Mountain | 45 (4.5) | 357 (5.5) | |
| West North Central | 44 (4.4) | 449 (6.9) | |
| West South Central | 29 (2.9) | 485 (7.5) | |
| Pacific | 10 (1.0) | 121 (1.9) | |
| South Central | 0 (0) | 41 (0.6) | |
| LTACH admission | |||
| STACH length-of-stay in days, mean (SD) | 26.7 (13.2) | 19.6 (13.8) | 0.17b,c |
| Patients requiring invasive mechanical ventilation, No. (%) | 447 (48.1) | 2,871 (44.2) | 0.08c,d |
| Patients with a tracheostomy in-place, No. (%) | 469 (62.2) | 3,178 (48.9) | 0.08c,d |
| LTACH Course | |||
| LOS, mean, days (SD) | 26.7 (19.2) | 31.5 (22.6) | −0.07b,c |
| Discharge disposition, No. (%)g | 0.01e | ||
| Mortality | 141 (14.3) | 1,133 (17.6) | |
| Home | 212 (21.5) | 1,186 (18.4) | |
| STACH (readmission) | 87 (8.8) | 644 (10.0) | |
| Lower level of careh | 524 (53.0) | 3,135 (48.7) | |
| Otheri | 24 (2.4) | 344 (5.3) |
LOS = length of stay; LTACH = long-term acute-care hospital; STACH = short-term acute-care hospital.
Point-biserial correlation coefficient,b Goodman and Kruskal lambda,e or phi coefficientd were used to indicate the strength of a measure’s relationship to a patient having COVID-19 based on the statistic’s divergence from zero, and in the case of b and d, whether there was either a negative or positive relationship.
Approximate significance at the .001 level for the test of association.
No network LTACH facilities are located in the New England region.
7,430 of the 7,489 total patients were discharged at the time of analysis.
Lower level of care includes inpatient rehabilitation hospitals and skilled nursing facilities.
“Other” includes left against medical advice, LTACH, nursing home, federal hospital, hospice, and unknown.
One stress adaptation to the pandemic was alteration of the care processes associated with patient-family services. We constructed a novel family support program in response to a necessary no-visitor policy implemented to protect patients and staff. We expedited this program’s development to fill the emotional void resulting from distancing, because close family communication is essential for the healing process.33, 34, 35, 36 This centrally managed program consisted of outpatient clinic staff redeployed from the parent health organization, including therapists, athletic trainers, and administrative staff. These additional staff members in each LTACH were specially trained on family and surrogate communication to provide clinical updates and support during the acute and recovery phases of COVID-19. Twice daily, these individuals discussed clinical results and functional status with patients’ families, fielded questions and requests from the family regarding their loved one, and facilitated family-clinical team communication. End-of-life issues were handled by nursing staff together with attending and palliative care physicians. Enhanced virtual support was also provided to families for patients with COVID-19 who died during their LTACH stay (n = 141, 14.3%) (Table 1).
The challenge with any work system modification is to develop prevention strategies, which adequately address complex, dynamic, and unstable systems. Processes arising from prevention strategies need to be dynamically stable and should contain specific adaptations for the system to remain under control. We developed adaptations that included wide-ranging strategies for physicians, clinical staff, and health-care partners, including local acute hospitals, in-network inpatient rehabilitation hospitals, and regional skilled nursing facilities. The VOH was critical in providing effective coordination of all LTACHs in the network based on varying levels of COVID-19 prevalence. Responding rapidly to virus surges in different locations was critical for ensuring adequate time for preparing all LTACHs to flexibly serve in any necessary capacity. During this time, LTACHs have continued to treat non-COVID-19 patients, with some patients at earlier stages in their critical illness admitted from the ICU to offload ICU resources, with a total of 6,497 patients admitted to our LTACH network without confirmed infection (Table 1). Based on our application data and LTACH EHR databases analyzing and projecting future surges and cold spots, modifications necessary to transform LTACHs acute care COVID-19 hospitals have been removed so the LTACHs could efficiently care for COVID-19 recovery patients and noninfected patients with chronic critical illness.
Discussion
After many modifications to the hospitals and hospital operations, approximately 1,000 COVID-19-positive patients and COVID-19 recovery patients were treated in 94 LTACHs from March through May 2020. We demonstrate that by following a resilient work system structure, LTACHs can rapidly adapt and transform within the health-care continuum from an LTACH to the role of a “Critical Illness Recovery Hospital” that can safely manage acutely ill patients with more severe clinical manifestations of SARS-CoV-2. LTACH care represents a unique combination of hospital acute care and longer-term recovery as a post-acute venue. With enhanced strategies coupled with accurate selection for admission, COVID-19-positive patients and COVID-19 recovery patients can be treated in LTACHs safely alongside patients without COVID-19.
Because many patients with COVID-19 respiratory failure require prolonged MV, LTACHs are positioned to help enhance and ensure recovery. LTACHs have developed specialized strategies for liberation from prolonged mechanical ventilation, promoting physical recovery through innovative therapies and nutrition programs while reducing the risk of adverse ventilator-associated events, including pneumonia and infection. LTACHs also require high-acuity nursing capabilities to treat patients with chronic critical illness.
In addition to providing treatment for patients with severe response to the virus, LTACHs also provide care for COVID-19-positive patients who require support during recovery. The long-term sequelae of post-COVID patients fits the LTACH model of care. Post-acute care has been recognized as required for COVID-19 patient recovery; respiratory physiotherapy and other post-acute rehabilitation are necessary to return these individuals to functional levels as quickly as possible.37, 38, 39, 40, 41, 42 Even with a less severe COVID-19 response, therapy may be required to counteract muscle weakness that could delay patient recovery.17
With the rising number of cases and hospitalizations with the COVID-19 pandemic, the primary concerns of the health-care community continue to include resource shortages and overcrowding, as hospital and ICU capacity reaches critical volumes in many locations,43 supporting the need for alternative treatment venues such as LTACHs in response to this burden. After repurposing nonclinical hospital space (eg, lobbies, hallways), hospitals, local governments, and relief organizations have also employed nonclinical spaces such as convention centers, parking structures, and field tents, and have triaged patients using telehealth services. The critical care staffing pool of specially trained physicians, nurses, and respiratory therapists is also strained, as the demand for ICU beds and critical care services has skyrocketed in many parts of the country. LTACHs provide a source of additional high-acuity beds and well-experienced critical care staff to help support hospitals during this pandemic.
Our network of 94 LTACHs has demonstrated preparation and implementation of modifications that support the treatment of active COVID-19 patients and patients recovering from moderate-to-severe response to COVID-19 infection. We show that LTACHs successfully play a dual role as a substitute for ICU beds in regions with high COVID-19 surge levels and as a post-ICU provider or partner in the continuum of care. LTACHs have a critical role to play in caring for patients during COVID-19 pandemic and future crises that overwhelm our health-care system.
Acknowledgments
Author contributions: A. M. G. takes responsibility for the content of the manuscript, including the data and analysis. A. M. D. and W. O. B.-C. had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. K. S. M. and S. I. H. contributed substantially to the study design, data analysis and interpretation, and the writing of the manuscript.
Financial/nonfinancial disclosures: None declared.
References
- 1.Ma X., Vervoort D. Critical care capacity during the COVID-19 pandemic: global availability of intensive care beds. J Crit Care. 2020;58:96–97. doi: 10.1016/j.jcrc.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aziz S., Arabi Y.M., Alhazzani W. Managing ICU surge during the COVID-19 crisis: rapid guidelines. Intensive Care Med. 2020;46(7):1303–1325. doi: 10.1007/s00134-020-06092-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Makam A.N., Grabowski D.C. How can we ramp up hospital capacity to handle the surge of COVID-19 patients? Long-term acute care hospitals can play a critical role. Health Affairs. 2020 doi: 10.1377/hblog20200410.606195. [DOI] [Google Scholar]
- 4.Miller T., Canfield C., Buckingham T. Long-term acute care: where does it fit in the health care continuum? Am J Crit Care. 2016;25(4):364–367. doi: 10.4037/ajcc2016766. [DOI] [PubMed] [Google Scholar]
- 5.Grasselli G., Pesenti A., Cecconi M. Early experience and forecast during an emergency response in Lombardy. Italy. JAMA. 2020;323(16):1545–1546. doi: 10.1001/jama.2020.4031. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Severe outcomes among patients with Coronavirus disease 2019 (COVID-19) United States, February 12-March 16, 2020. https://www.cdc.gov/mmwr/volumes/69/wr/mm6912e2.htm?s_cid=mm6912e2_w. Key Updates for Week 29, ending July 18, 2020. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html. Accessed July 22, 2020.
- 7.Rak K.J., Ashcraft L.E., Kuza C.C. Effective care practices in patients receiving prolonged mechanical ventilation. an ethnographic study. Am J Respir Crit Care Med. 2020;201(7):823–831. doi: 10.1164/rccm.201910-2006OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Inoue S., Hatakeyama J., Kondo Y. Post-intensive care syndrome: its pathophysiology, prevention, and future directions. Acute Med Surg. 2019;6(3):233–246. doi: 10.1002/ams2.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sasannejad C., Ely E.W., Lahiri S. Long-term cognitive impairment after acute respiratory distress syndrome: a review of clinical impact and pathophysiological mechanisms. Crit Care. 2019;23(1):352. doi: 10.1186/s13054-019-2626-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.LaBuzetta J.N., Rosand J., VranceanuvA -M. Review: post-intensive care syndrome: unique challenges in the neurointensive care unit. Neurocrit Care. 2019;31(3):534–545. doi: 10.1007/s12028-019-00826-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carfi A., Bernabei R., Landi F. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324(6):603–605. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stam H.J., Stucki G., Bickenbach J. Covid-19 and post intensive care syndrome: a call for action. J Rehabil Med. 2020;52(4) doi: 10.2340/16501977-2677. [DOI] [PubMed] [Google Scholar]
- 13.Griffin K.M., Karas M.G., Ivascu N.S., Lief L. Hospital preparedness for COVID-19: a practical guide from a critical care perspective. Am J Respir Crit Care Med. 2020;201(11):1337–1344. doi: 10.1164/rccm.202004-1037CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wax R.S., Christian M.D. Practical recommendations for critical care and anesthesiology teams caring for novel Coronavirus (2019-nCoV) patients. Can J Anaesth. 2020;67(5):568–576. doi: 10.1007/s12630-020-01591-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Robbins A., Beilman G.J., Amdahl Transforming a long-term acute care hospital into a COVID-19-designated hospital. Surg Infect (Larchmt) 2020;21(9):729–731. doi: 10.1089/sur.2020.155. [DOI] [PubMed] [Google Scholar]
- 16.Select Medical. 4714 Gettysburg Road, Mechanicsburg, PA 17055.
- 17.Centers for Medicare & Medicaid Services. https://www.federalregister.gov/documents/2019/08/16/2019-16762/medicare-program-hospital-inpatient-prospective-payment-systems-for-acute-care-hospitals-and-the
- 18.Jubran A., Grant B.J.B., Duffner L.A. Long-term outcome after prolonged mechanical ventilation: a long-term acute-care hospital study. Am J Respir Crit Care Med. 2019;199(12):1508–1516. doi: 10.1164/rccm.201806-1131OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fan E., Zakhary B., Amaral A. Clinical practice guideline: summary for clinicians. Liberation from mechanical ventilation in critically ill adults. Ann Am Thorac Soc. 2017;14(3):441–443. doi: 10.1513/AnnalsATS.201612-993CME. [DOI] [PubMed] [Google Scholar]
- 20.Szubski C., Tellez A., Barsoum W. Predicting discharge to a long-term acute care hospital after admission to an intensive care unit. Am J Crit Care. 2014;23(4):e46–e53. doi: 10.4037/ajcc2014985. [DOI] [PubMed] [Google Scholar]
- 21.Rutherford P.A., Provost L.P., Kotagal U.R., Luther K., Anderson A. Institute for Healthcare Improvement; Cambridge, MA: 2017. Achieving hospital-wide patient flow. IHI White Paper. [Google Scholar]
- 22.Kim G., Wang M., Pan H. A health system response to COVID-19 in long-term care and post-acute care: a three-phase approach. J Am Geriatr Soc. 2020;68(6):1155–1161. doi: 10.1111/jgs.16513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Woolliscroft J.O. Innovation in response to the COVID-19 pandemic crisis. Acad Med. 2020;95(8):1140–1142. doi: 10.1097/ACM.0000000000003402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wiig S., Aase K., Billett S. Defining the boundaries and operational concepts of resilience in the resilience in healthcare research program. BMC Health Serv Res. 2020;20(1):330. doi: 10.1186/s12913-020-05224-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fallah-Aliabadi S., Ostadtaghizadeh A., Ardalan A. Towards developing a model for the evaluation of hospital disaster resilience: a systematic review. BMC Health Serv Res. 2020;20(1):64. doi: 10.1186/s12913-020-4915-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rosso C.B., Saurin T.A. The joint use of resilience engineering and lean production for work system design: a study in healthcare. Appl Ergon. 2018;71:45–56. doi: 10.1016/j.apergo.2018.04.004. [DOI] [PubMed] [Google Scholar]
- 27.Costella M.F., Saurin T.A., Macedo Guimarães L.B. A method for assessing health and safety management systems from the resilience engineering perspective. Saf Sci. 2009;47:1056e67. [Google Scholar]
- 28.Iflaifel M., Lim R.H., Ryan K., Crowley C. Resilient health care: a systematic review of conceptualisations, study methods and factors that develop resilience. BMC Health Serv Res. 2020;20(1):324. doi: 10.1186/s12913-020-05208-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meyer B.A., Conners S. How the fastest growing academic health center prepared for the COVID-19 surge. Becker’s Hospital Review. https://www.beckershospitalreview.com/hospital-management-administration/how-the-fastest-growing-academic-health-center-prepared-for-the-covid-19-surge.html
- 30.Franklin B.J., Gandhi T.K., Bates D.W. Impact of multidisciplinary team huddles on patient safety: a systematic review and proposed taxonomy. BMJ Qual Saf. 2020;29(10):1–2. doi: 10.1136/bmjqs-2019-009911. [DOI] [PubMed] [Google Scholar]
- 31.Jones K.J., Crowe J., Allen J.A. The impact of post-fall huddles on repeat fall rates and perceptions of safety culture: a quasi-experimental evaluation of a patient safety demonstration project. BMC Health Serv Res. 2019;19(1):650. doi: 10.1186/s12913-019-4453-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Johns Hopkins Coronavirus Resource Center, Johns Hopkins University COVID-19 United States Cases by County. https://coronavirus.jhu.edu/map.html Accessed March through July, 2020.
- 33.Hart J.L., Turnbull A.E., Oppenheim I.M., Courtright K.R. Family-centered care during the COVID-19 era. J Pain Symptom Manage. 2020;60(2):e93–e97. doi: 10.1016/j.jpainsymman.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Davidson J.E., Jones C., Bienvenu O.J. Family response to critical illness: postintensive care syndrome—family. Crit Care Med. 2012;40(2):618–624. doi: 10.1097/CCM.0b013e318236ebf9. [DOI] [PubMed] [Google Scholar]
- 35.Goldfarb M., Bibas L., Burns K. Family engagement in the cardiovascular intensive care unit in the COVID era. Can J Cardiol. 2020;36(8):1327.e1–1327.e2. doi: 10.1016/j.cjca.2020.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hado E., Feinberg L.F. Amid the COVID-19 pandemic, meaningful communication between family caregivers and residents of long-term care facilities is imperative. J Aging Soc Policy. 2020;32(4-5):410–415. doi: 10.1080/08959420.2020.1765684. [DOI] [PubMed] [Google Scholar]
- 37.Kiekens C., Boldrini P., Andreoli A. Rehabilitation and respiratory management in the acute and early post-acute phase. “Instant paper from the field” on rehabilitation answers to the Covid-19 emergency. Eur J Phys Rehabil Med. 2020;56(3):323–326. doi: 10.23736/S1973-9087.20.06305-4. [DOI] [PubMed] [Google Scholar]
- 38.COVID-19 exposes the critical importance of patient rehabilitation. World Health Organization Europe. 2020. http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/4/covid-19-exposes-the-critical-importance-of-patient-rehabilitation
- 39.Wiesner B., Bachmann M., Blum T.G. Responsibilities of weaning centers during the COVID-19 pandemic outbreak: recommendations for the assignment of ICU capacities in COVID-19 patients as shown by the Berlin-Brandenburg POST-SAVE-Model. Pneumologie. 2020;74(6):358–365. doi: 10.1055/a-1153-9710. [Article in German; Abstract available in German from the publisher] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sheehy L.M. Considerations for postacute rehabilitation for survivors of COVID-19. JMIR Public Health Surveill. 2020;6(2) doi: 10.2196/19462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tumlinson A., Altman W., Glaudemans J. Post-acute care preparedness in a COVID-19 world. J Am Geriatr Soc. 2020;68(6):1150–1154. doi: 10.1111/jgs.16519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tenforde M.W., Kim S.S., Lindsell C.J. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network—United States, March-June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(30):993–998. doi: 10.15585/mmwr.mm6930e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kaplan L.J., Kleinpell R., Maves R.C., Doersam J.K., Raman R., Ferraro D.M. Critical care clinician reports on coronavirus disease 2019: results from a national survey of 4,875 ICU providers. Critical Care Explorations. 2020;2(5) doi: 10.1097/CCE.0000000000000125. [DOI] [PMC free article] [PubMed] [Google Scholar]