Abstract
Amidst the unprecedented global pandemic of COVID-19, attending to the needs of adolescents with diabetes mellitus became more challenging. They faced the uncertainty of access to care and the attendant problems of a lockdown. We present the nurse-led telehealth initiative for adolescents with diabetes mellitus, leveraging on existing infrastructure and resources with the aim of addressing the anticipated challenges that many of the adolescents might face. The initiative was well received among those who participated, and there were no significant adverse effects noted.
Keywords: Telehealth, COVID-19, Adolescent diabetes mellitus, Nurse-led
Implications and Contribution.
Providing care to young people with chronic conditions is challenging under the best circumstances. This report describes a nurse-led telehealth initiative to provide adolescent diabetes care during the coronavirus disease 2019 pandemic.
On January 30, 2020, World Health Organization declared coronavirus disease 2019 (COVID-19) as a Public Health Emergency of International Concern. Since then, the Singapore government implemented a series of measures to curb the spread of COVID-19 [1]. Amidst the lockdown, schools and workplaces were shut down, and most Singaporeans were made to stay home. This resulted in distruption to daily schedules, decreased social interaction with friends and teachers, and changes in activity and dietary habits. In line with these measures, the Ministry of Health (Singapore) also implemented directives to defer nonurgent health care services. Hence, we needed an alternative process to swiftly address the patients’ safety, as well as their continued access to health care and medication.
Unique Challenges During the Pandemic
Safeguarding of psychophysical health of the adolescents with diabetes mellitus (DM) in a lockdown situation was paramount. With the closure of schools, their daily routines were severely disrupted. They lost the protective structure of scheduled mealtimes and physical activities in school, as well as access to subsidized canteen meals. All these made the day-to-day administration of insulin more challenging. Depending on the adolescent’s level of competence with self-management, some would require more guidance to minimize probability of insulin misdosing. The consequence of the latter would result in undesirable fluctuation in glycemic levels.
World Health Organization recommends that all children and adolescents aged 6–17 years should do 60 minutes or more of physical activity daily, including moderate to vigorous aerobic activity, as well as muscle- and bone-strengthening activities. These same recommendations also apply to adolescents with DM [2]. Exercise confers far-reaching benefits on hemoglobin A1c (HbA1c), weight control, and vascular health [3], all of which help mitigate the cardiovascular risk in diabetic patients [4]. With the increased sedentary lifestyle and screentime as a result of the lockdown [5], we were concerned that these habits will have an adverse effect on their cardiovascular health, and hence, providing advice on alternatives for home-based physical activity was of great importance.
The COVID-19 pandemic lockdown and social distancing measures created additional psychosocial stressors to the adolescents. Those in their graduation year faced an uncertainty of jobs future in a climate of escalating unemployment [6]. Some adolescents found social distancing measures very demanding, during a unique time in their lives when they were gaining independence and prioritizing peers over family. Some expressed anxiety over their own health because people with chronic health conditions including DM have an increased risk of COVID-19–related mortality, although this phenomenon has not yet been reported in adolescents with DM [7]. Maintaining contact with the adolescents would serve as an oversight of the potential stressors.
Prepandemic Workflow
Our center is one of two public tertiary pediatric hospitals in Singapore and serves more than 300 patients with DM on active follow-ups care in line with recommendations made by the International Society for Paediatric and Adolescent Diabetes, which involve three monthly outpatient follow-ups for monitoring and education [2]. Starting from age 13 years, the adolescents commence on an Advanced Practice Nurse (APN)-led Structured Transition Education Program (STEP), which aims to address the unique challenges faced by adolescents living with DM by engaging, educating, and empowering them with skills to manage DM (including home self-monitoring blood glucose, exercise care, hypoglycemia and ketones management, review of dietary behaviors, and psychosocial health). These essentials will prepare them for transition into adult DM services by age 18–21 years. We selected this group of patients to embark on a telehealth pilot initiative because: (1) STEP would not be interrupted; (2) adolescents have shown to exhibit the worst glycemic control among individuals with type 1 DM across the lifespan, hence a particularly vulnerable group of patients [3,8]; (3) high ownership of personal electronic devices among adolescents conferred better accessibility to telehealth [4,9]. In addition, we hoped that telehealth would also offer the opportunity to address the unique challenges of COVID-19 pandemic highlighted earlier [1], [2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13].
Use of Telehealth—A Bridging Solution
The telehealth initiative began in February 2020 in accordance to the National Telemedicine Guidelines [10], reaching out to both adolescents with type1 DM on insulin therapy as well as those with type 2 DM on oral hypoglycemic agents alone or needing additional insulin therapy. The key components of the telehealth service included (1) teleconsultation platform, (2) payment platform, (3) laboratory tests, (4) and medication collection/delivery. The workflow began with the APN sending a text message to inform on clinic conversion to telehealth service. Once verbal consent was obtained, the APN would provide information to the adolescents and their parents regarding laboratory test for blood HbA1c, collection/delivery of medication, and electronic submission of available home blood glucose profile. The patients were required to come to hospital only for laboratory test and medication collection. Prescriptions were prefilled and transmitted electronically via a closed-loop prescribing system setup with the hospital pharmacy. This allowed for expedited in-person collection of medications; there was also the option of medication home delivery.
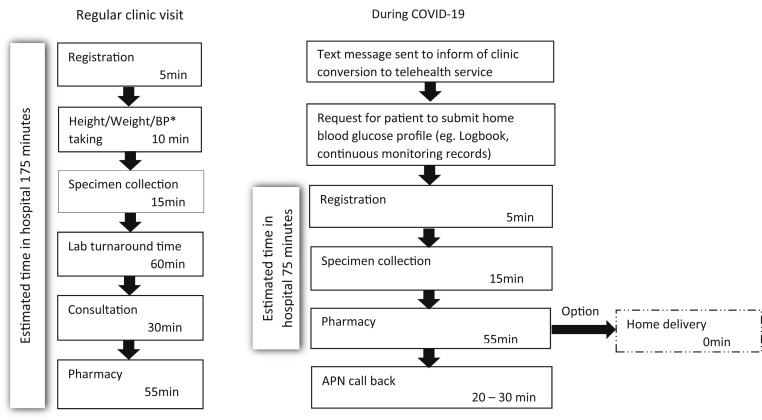
Once HbA1c result was available, an audio-call back (approximately 20–30 minutes) was conducted, covering topics in STEP, addressing any titration of insulin and issues arising from the COVID-19 crisis. Figure 1 compares the workflows of a regular APN in-person clinic visit and a telehealth consultation. There was an appreciable reduction in time spent in hospital with the modified workflow.
Figure 1.
Flowchart showing workflow of a regular clinic visit versus a modified workflow with the use of telehealth during COVID-19. Estimated time taken in hospital displayed in minutes, based on recent internal clinic review. BP, blood pressure.
Between February and June 2020, a total of 60 adolescents were scheduled for in-person clinic consultations. Thirty-five adolescents used the telehealth service, 17 requested to postpone consultation, four preferred to continue with in-person clinic consultation, and four were uncontactable. Of the 35 adolescents, the APN attended to 28 patients with type 1 DM and seven patients with type 2 diabetes. Main concerns shared were issues on adjusting insulin doses during school closure and modifying food choices to better stabilize glycemia fluctuations.
As part of the hospital quality improvement initiatives, we conducted a user experience survey, for which 14 adolescents and six parents responded. Sixty-three percent of the adolescents felt very satisfied with the administrative processes of telehealth service (instructions/information/guidance from registration, laboratory HbA1c test, and collection of medication are simple and convenient) and will choose APN-led telehealth service. Seventy percent felt very satisfied with duration of time spent on APN-led assessment and consultation with at ease to speak, adequate opportunity to ask questions, and being understood over the telehealth session. Both the adolescents and parents reported that telehealth was similar (80%) to in-person clinic, and 20% reported superior to the in-person clinics. Sixty-five percent of the adolescents and 67% of parents would continue to use this telehealth care with the APN. Feedback from adolescents and parents suggested that spending less time in the hospital greatly reduced their anxiety around contracting COVID-19.
During the same period, there were no emergency visits for diabetes-related adverse events, and HbA1c levels remained stable (averaging HbA1c of 8.2%) among those who had already returned for a second visit.
Discussion
Studies have shown that timely use of telehealth for DM care has encouraging results in (1) detecting early signs of deterioration; (2) education for self-management; and (3) possible reduction in the visits to emergency rooms and hospital admissions [11]. This engagement also gave the APN an opportunity to screen for potential COVID-19–related issues highlighted earlier. The timely identification of at-risk individuals allowed for onward referral to social services for psychological support or financial assistance.
This pilot initiative was made possible by leveraging on the institution’s existing infrastructure of telehealth and integrated pharmacy services and available subsidies through Medisave (Singapore’s healthcare financing framework) on the diabetes-related care[12].
As our service shifted into a modular system, little additional manpower was required to pilot this initiative. This meant minimal disruption to existing workflows and ensured continuity of individualized care. The reduction of contact time in hospital limited exposure of both health care providers and patients to potential risk for infection. This also allowed us to conserve the use of protective equipment.
We recognize that the use of other DM biotechnology such as intermittent/continuous glucose monitoring systems can complement telehealth services [13]. This will eliminate the need for patients to return for blood tests during the COVID-19 pandemic. Unfortunately, these are not easily accessible largely because of the prohibitive costs.
Conclusion
Pandemics pose unique challenges to health care delivery and services, and contingencies need to be planned for in advance. As health systems are being reconfigured, telemedicine has served to bridge the need for continuity of care of patients during COVID-19 pandemic, especially in the management of chronic diseases. Our telehealth initiative was well-received, and no adverse outcomes were observed. As COVID-19 continues to spread globally, we hope to provide some insight into the challenges faced by adolescents with DM and practical steps in providing care for them during the crisis.
Acknowledgments
Deepest appreciation to all adolescents and parents who were receptive to the use of telehealth.
Footnotes
Conflicts of interest: There were no potential conflicts of interest to declare.
Funding Sources
No funding was received for this write up.
References
- 1.Ministry of Health Singapore Updates on COVID-19 (Coronavirus disease 2019) www.moh.gov.sg Available at:
- 2.Pihoker C., Forsander G., Fantahun B. ISPAD Clinical Practice Consensus Guidelines 2018: The delivery of ambulatory diabetes care to children and adolescents with diabetes. Pediatr Diabetes. 2018;19:84–104. doi: 10.1111/pedi.12757. [DOI] [PubMed] [Google Scholar]
- 3.MacMillan F., Kirk A., Mutrie N. A systematic review of physical activity and sedentary behavior intervention studies in youth with type 1 diabetes: Study characteristics, intervention design, and efficacy. Pediatr Diabetes. 2014;15:175–189. doi: 10.1111/pedi.12060. [DOI] [PubMed] [Google Scholar]
- 4.Reddigan J.I., Riddell M.C., Kuk J.L. The joint association of physical activity and glycaemic control in predicting cardiovascular death and all-cause mortality in the US population. Diabetologia. 2012;55:632–635. doi: 10.1007/s00125-011-2374-3. [DOI] [PubMed] [Google Scholar]
- 5.Pietrobelli A., Pecoraro L., Ferruzzi A. Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: A longitudinal study. Obesity (Silver Spring) 2020 doi: 10.1002/oby.22861. Epub 2020/04/30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc Health. 2020;4:421. doi: 10.1016/S2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang I., Lim M.A., Pranata R. Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia - a systematic review, meta-analysis, and meta-regression. Diabetes Metab Syndr. 2020;14:395–403. doi: 10.1016/j.dsx.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Foster N.C., Beck R.W., Miller K.M. State of type 1 diabetes management and outcomes from the T1D exchange in 2016-2018. Diabetes Technol Ther. 2019;21:66–72. doi: 10.1089/dia.2018.0384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Youth Council Singapore Youth statistics in brief 2019. https://www.nyc.gov.sg/en/initiatives/resources/youth-statistics-in-brief/ Available at:
- 10.Ministry of Health Singapore National telemedicine guidelines. www.moh.gov.sg Available at:
- 11.Ellis D.A., Naar-King S., Chen X. Multisystemic therapy compared to telephone support for youth with poorly controlled diabetes: Findings from a randomized controlled trial. Ann Behav Med. 2012;44:207–215. doi: 10.1007/s12160-012-9378-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ministry of Health Singapore Time-limited extension of CHAS subsidy and use of Medisave for follow up of chronic conditions through video consultations in view of COVID-19. www.moh.gov.sg/covid-19/vc Available at:
- 13.Greenwood D.A., Young H.M., Quinn C.C. Telehealth remote monitoring systematic review: Structured self-monitoring of blood glucose and impact on A1C. J Diabetes Sci Technol. 2014;8:378–389. doi: 10.1177/1932296813519311. [DOI] [PMC free article] [PubMed] [Google Scholar]