Since March 2020, all continents have been burdened with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic, which has led to a considerable health crisis.1 The magnitude of the challenges posed by the pandemic exceeded the expectations of the scientific community and public authorities, who rapidly developed strategies to properly manage the disease.2, 3, 4 However, the measures adopted to address the pandemic differed among European countries, including the type of lockdown, border closings, school closures, the use of facial masks, accessories protection, the use of SARS-CoV-2 reverse transcription polymerase chain reaction, and point-of-care for rapid-antigen detection diagnostic tests.5 These discrepancies have led to confusion for the population and to chaotic directions for physicians on how to manage the health crisis. Pediatricians have received contradicting information and recommendations regarding the role of children in the spread of coronavirus disease 2019 (COVID-19).5 This situation was due, in part, to drawing an arbitrary parallel with the influenza model.6 However, we learned that the number of confirmed pediatric cases is relatively low and that they account for <1% of hospitalized cases and deaths.5 , 7
This pandemic has had a major impact on pediatric clinical practice, with a major reduction in several routine medical services, as reported for the pediatric transplant activity in Europe8 or the decline in the practice of throat culture.9 In addition, the reduction in person-to-person contacts turned pediatric care from a direct face-to-face to a predominantly virtual-care practice.9
In this context, many pediatric research units throughout Europe and particularly those involved in infectious disease and epidemiology have devoted their funds and human resources to COVID-19 research. This situation raised the concern of the European societies of pediatrics, who are worried about the future of research in the area of pediatric infectious diseases. The aim of this commentary is to give a brief overview of the impact of the COVID-19 pandemic on pediatric infectious disease research and report on a French experience.
Changes in Infectious Diseases Research Revealed by Publication Trends
Because PubMed reflects scientific production, we searched in this database for the evolution of a few key subjects that we considered as sentinel topics to investigate the trend in pediatric infectious diseases research. As indicators we arbitrarily selected pneumococcal disease, a frequent pediatric infectious disease,10 and meningococcal diseases, an infectious disease with a severe prognosis.11 We searched key words related to these 2 conditions by MEDLINE via PubMed to compare them with publications on COVID-19. We focused on articles published since 2010, with no language restriction (last search October 1, 2020). For pneumococcal diseases, search terms were “Streptococcus pneumoniae” or “pneumococc∗” and “child∗” or “pediatric∗”; for meningococcal diseases, the terms were “Neisseria meningitidis” or “meningococc∗” and “child∗” or “pediatric∗”. For COVID-19, search the terms used were “COVID-19” or “Coronavirus disease 2019” or “SARS-CoV-2” and “child∗” or “pediatric∗”.
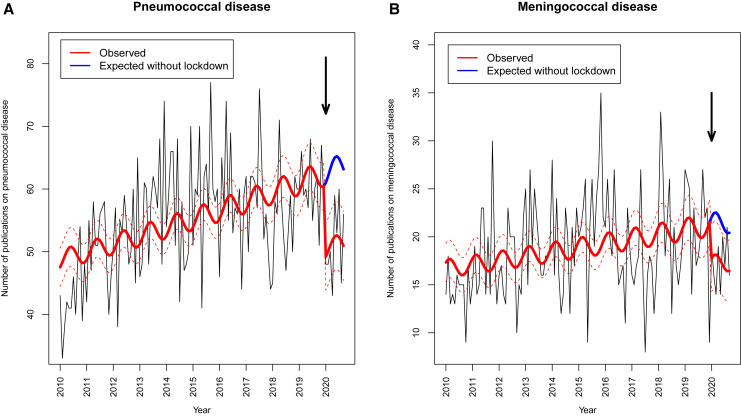
From January 1, 2010, to September 30, 2020, we found 7096 publications on pneumococcal and 2418 on meningococcal disease, including 464 and 156 respectively published in 2020. By comparison, we found 6731 publications on COVID-19 in 2020. Using interrupted time–series analysis with quasi-Poisson regression models,12 accounting for pre-existing secular trend and seasonality, we estimated the change in monthly publication rate of pneumococcal and meningococcal disease articles. For pneumococcal and meningococcal diseases, the monthly number of publications in 2020 decreased by 19% (95% CI 10%-27%, P = .0002) and 17% (95% confidence interval 1%-33%, P = .038), respectively (Figure, A and B; available at www.jpeds.com). Although these data confirm that research into COVID-19 is currently considered of crucial importance, at the same time they show that it may be detrimental to research on other pediatric infectious diseases.
Figure.
The dynamics of monthly publication rates in 2020 of A, pneumococcal and B, meningococcal disease articles in PubMed by interrupted time–series analysis with quasi-Poisson regression models, accounting for pre-existing secular trend and seasonality.
Shift of Paradigm
Pneumococcal and meningococcal disease provide a good example of how a redirection of resources to COVID-19 could be detrimental to research on other infectious diseases. First, the ecological niche of N meningitidis is the oropharynx of adolescents and young adults. The national lockdown applied in many countries to deal with the first COVID-19 wave led to strong contact mitigations in all ages. Specific mitigation measures are now targeting young adults and adolescents, who had contributed to spreading the virus, leading to the “second wave.” These measures include mandatory wearing of facial masks in high schools, colleges, and universities to reduce contacts between students. If these measures are sufficient to stop SARS-CoV-2 spread among young adults, they also may affect the transmission and carriage of other pathogens of the nasopharyngeal flora. Second, the ecological niche of S pneumoniae is the nasopharynx of young children. The epidemiology of this pathogen is highly affected by close contacts between young children and antibiotics exposure. Several studies emphasize that day-care attendance modalities and antibiotic exposure affect pneumococcal carriage and antibiotic resistance of strains.13 , 14
Recent data have documented the striking reduction in frequency of acute respiratory tract infections in pediatric emergency departments following COVID-19 mitigation measures.9 , 15 Because acute respiratory tract infections are the first cause of antibiotic prescription, their decrease may lead to substantially changing the antimicrobial selective pressure applied to nasopharyngeal pathogens of young children, including S pneumoniae.16 , 17
Several reports have shown that the incidence of specific pathogen infections such as influenza viruses, respiratory syncytial virus, meningococcus, and pneumococcus was reduced in many countries.18, 19, 20, 21 Australia reported a concurrent lower frequency of respiratory syncytial virus detection and admission to hospital for bronchiolitis in 2020 as compared with preceding years.19 In this country, despite schools reopening, a 99.4% reduction was reported in influenza detection following Australian public health measures.21 Influenza data reported to the World Health Organization's FluNet platform from 3 Southern Hemisphere areas (Oceania, South America, and Southern Africa) showed very low influenza activity during June to August 2020.18 These data suggest that the epidemiology of these infectious diseases may change in an unpredictable manner in the coming months and years, requiring close and active surveillance.18, 19, 20, 21
During the current health emergency, the top priority of many clinical research centers was to ensure proper care for children. COVID-19 research was helpful in several European countries, as the data generated and related information helped clinicians in their daily practices.7 , 22, 23, 24, 25, 26, 27 However, many clinical research groups have questioned how they could perform clinical trials not necessarily related to COVID-19 during the pandemic.22
To this regard, the increase in telemedicine use, electronic consent, and several other distant methods combined offered an opportunity to move to virtual research compatible with COVID-19 constraints.22 Furthermore, early in the pandemic's first wave, the US Food and Drug Administration proposed new guidance for industry to maintain research productivity so as to avoid the disruption of new and ongoing clinical trials.23
A French Experience
In light of the COVID-19 pandemic, the research working group on infectious diseases coordinated by the Clinic and Therapeutics Association for Children of Val-de-Marne and the French Association of Ambulatory Pediatrics made available to clinicians working in ambulatory settings and hospitals all the existing platforms of data exchange used for its studies.28 In early February 2020, through its pediatric bacterial meningitis network and by a fast-track process, the Clinic and Therapeutics Association for Children of Val-de-Marne recruited 60 pediatric ward units throughout France to conduct a national hospital-based prospective surveillance of SARS-CoV-2 infection.28 , 29 In contrast with the initial data reported on SARS-CoV-2, the study found that children <3 months old accounted for a large part of children admitted to hospital but were at the lowest risk of severe infection.29 These findings helped to better identify the risk of severe disease progression in children. Similarly, in Spain a registry was developed based on an existing network including 30 secondary and tertiary hospitals to obtain information on COVID-19 cases in children and to monitor the severity of the multisystem inflammatory syndrome in young patients.30 , 31 These data confirm the ability of European pediatric research centers to promptly react to emergencies by adopting effective solutions to the challenges to which they are exposed. However, at the same time the European pediatric societies are concerned regarding the future of pediatric infectious disease research in fields different than COVID-19, due to a major redirection of efforts and financial resources.
Conclusions
COVID-19 has redirected the interests and resources of research in infectious diseases and consequentially is changing the profile of the related scientific literature. If confirmed, the trend could become a real threat to the advancement of extensive knowledge in this area of science, with unpredictable long-term consequences. This working group would like to emphasize the importance of a common effort by pediatric societies to safeguard and ensure adequate resources to the ongoing and future research in pediatric infectious diseases areas besides COVID-19. Finally, we highlight the particular need to continue devoting research to new vaccines and treatments for pediatric infectious diseases, through effective International/European task-sharing. The French Association of Ambulatory Pediatrics is actively engaged in pursuing these goals within the frame of its membership in the European Paediatric Association and urges the other well-established European networks to join their common efforts.
Footnotes
The authors declare no conflicts of interest.
Appendix
References
- 1.Worldometer. Report on covid-19 coronavirus pandemic. https://www.worldometers.info/coronavirus/
- 2.de Weck O., Krob D., Lefei L., Lui P., Rauzy A., Zhang X. Handling the COVID-19 crisis: toward an agile model-based systems approach. Systems Engineering. 2020 doi: 10.1002/sys.21557. [DOI] [Google Scholar]
- 3.Lazzerini M., Putoto G. COVID-19 in Italy: momentous decisions and many uncertainties. Lancet Glob Health. 2020;8:e641–e642. doi: 10.1016/S2214-109X(20)30110-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bedford J., Enria D., Giesecke J. Living with the COVID-19 pandemic: act now with the tools we have. Lancet. 2020;396:1314–1316. doi: 10.1016/S0140-6736(20)32117-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.European Center for Disease Control and Prevention (ECDC) COVID-19 in children and the role of school settings in COVID-19 transmission.Technical report. https://www.ecdc.europa.eu/en/publications-data/children-and-school-settings-covid-19-transmission
- 6.Tsang T.K., Fang V.J., Chan K.H. Individual correlates of infectivity of influenza A virus infections in households. PLoS One. 2016;11:e0154418. doi: 10.1371/journal.pone.0154418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parri N., Lenge M., Buonsenso D. Coronavirus Infection in Pediatric Emergency Departments Research Group. Children with Covid-19 in pediatric emergency departments in Italy. N Engl J Med. 2020;383:187–190. doi: 10.1056/NEJMc2007617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Doná D., Torres Canizales J., Benetti E. Pediatric transplantation in Europe during the COVID-19 pandemic: early impact on activity and healthcare. Clin Transplant. 2020;34:e14063. doi: 10.1111/ctr.14063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Somekh I., Somech R., Pettoello-Mantovani M., Somekh E. Changes in routine pediatric practice in light of coronavirus 2019 (COVID-19) J Pediatr. 2020;224:190–193. doi: 10.1016/j.jpeds.2020.05.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.European Centre for Disease Prevention and Control (ECDC) Invasive pneumococcal disease. https://www.ecdc.europa.eu/en/invasive-pneumococcal-disease
- 11.US Centers For Disease Control and Prevention (CDC) Meningococcal Disease. https://www.cdc.gov/meningococcal/index.html
- 12.Dean C.B. Testing for overdispersion in Poisson and binomial regression models. J Am Stat Assoc. 1992;87:451–457. [Google Scholar]
- 13.Katz A., Leibovitz E., Timchenko V.N. Antibiotic susceptibility, serotype distribution and vaccine coverage of nasopharyngeal and oropharyngeal Streptococcus pneumoniae in a day-care centre in St. Petersburg, Russia. Scand J Infect Dis. 2007;39:293–298. doi: 10.1080/00365540600987741. [DOI] [PubMed] [Google Scholar]
- 14.Levy C., Ouldali N., Caeymaex L., Angoulvant F., Varon E., Cohen R. Diversity of serotype replacement after pneumococcal conjugate vaccine implementation in Europe. J Pediatr. 2019;213:252–253 e3. doi: 10.1016/j.jpeds.2019.07.057. [DOI] [PubMed] [Google Scholar]
- 15.Angoulvant F., Ouldali N., Yang D.D. COVID-19 pandemic: impact caused by school closure and national lockdown on pediatric visits and admissions for viral and non-viral infections, a time series analysis. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Trinh N.T.H., Cohen R., Lemaitre M. Community antibiotic prescribing for children in France from 2015 to 2017: a cross-sectional national study. J Antimicrob Chemother. 2020;75:2344–2352. doi: 10.1093/jac/dkaa162. [DOI] [PubMed] [Google Scholar]
- 17.Danino D., Givon-Lavi N., Ben-Shimol S., Greenberg D., Dagan R. understanding the evolution of antibiotic-nonsusceptible pneumococcal nasopharyngeal colonization following pneumococcal conjugate vaccine implementation in young children. Clin Infect Dis. 2019;69:648–656. doi: 10.1093/cid/ciy926. [DOI] [PubMed] [Google Scholar]
- 18.Olsen S.J., Azziz-Baumgartner E., Budd A.P. Decreased influenza activity during the COVID-19 Pandemic—United States, Australia, Chile, and South Africa, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1305–1309. doi: 10.15585/mmwr.mm6937a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Britton P.N., Hu N., Saravanos G. COVID-19 public health measures and respiratory syncytial virus. Lancet Child Adolesc Health. 2020;4:e42–e43. doi: 10.1016/S2352-4642(20)30307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Taha M.K., Deghmane A.E. Impact of COVID-19 pandemic and the lockdown on invasive meningococcal disease. BMC Res Notes. 2020;13:399. doi: 10.1186/s13104-020-05241-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yeoh D.K., Foley D.A., Minney-Smith C.A. The impact of COVID-19 public health measures on detections of influenza and respiratory syncytial virus in children during the 2020 Australian winter. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Felix C. Clinical Research in the Time of COVID-19. Int J Radiat Oncol Biol Phys. 2020;108:489–490. doi: 10.1016/j.ijrobp.2020.06.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.US Food & Drug Administration 2020 Guidance on conduct of clinical trials of medical products during COVID-19 public health emergency: guidance for industry, investigators, and institutional review boards. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/fda-guidance-conduct-clinical-trials-medical-products-during-covid-19-public-health-emergency
- 24.Galvan Casas C., Catala A., Carretero Hernandez G. Classification of the cutaneous manifestations of COVID-19: a rapid prospective nationwide consensus study in Spain with 375 cases. Br J Dermatol. 2020;183:71–77. doi: 10.1111/bjd.19163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Posfay-Barbe K.M., Wagner N., Gauthey M., Moussaoui D., Loevy N., Diana A. COVID-19 in children and the dynamics of infection in families. Pediatrics. 2020;146:e20201576. doi: 10.1542/peds.2020-1576. [DOI] [PubMed] [Google Scholar]
- 26.Somekh E., Gleyzer A., Heller E. The role of children in the dynamics of intra family coronavirus 2019 spread in densely populated area. Pediatr Infect Dis J. 2020;39:e202–e204. doi: 10.1097/INF.0000000000002783. [DOI] [PubMed] [Google Scholar]
- 27.Somekh I., Yakub Hanna H., Heller E., Bibi H., Somekh E. Age-dependent sensory impairment in COVID-19 infection and its correlation with ACE2 expression. Pediatr Infect Dis J. 2020;39:e270–e272. doi: 10.1097/INF.0000000000002817. [DOI] [PubMed] [Google Scholar]
- 28.Levy C., Vie le Sage F., Varon E., Chalumeau M., Grimprel E., Cohen R. Pediatric ambulatory and hospital networks for surveillance and clinical epidemiology of community-acquired infections. J Pediatr. 2018;194:269–270.e2. doi: 10.1016/j.jpeds.2017.11.050. [DOI] [PubMed] [Google Scholar]
- 29.Ouldali N., Yang D.D., Madhi F. Factors associated with severe SARS-CoV-2 infection in children: a French national surveillance. Pediatrics. 2020 doi: 10.1542/peds.2020-023432. [DOI] [PubMed] [Google Scholar]
- 30.Moraleda C., Serna-Pascual M., Soriano-Arandes A., Silvia Simó S., Epalza C., Santos M. Multi-inflammatory syndrome in children related to SARS-CoV-2 in Spain. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tagarro A., Epalza C., Santos M., Sanz-Santaeufemia F.J., Otheo E., Moraleda C. Screening and severity of coronavirus disease 2019 (COVID-19) in children in Madrid, Spain. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]