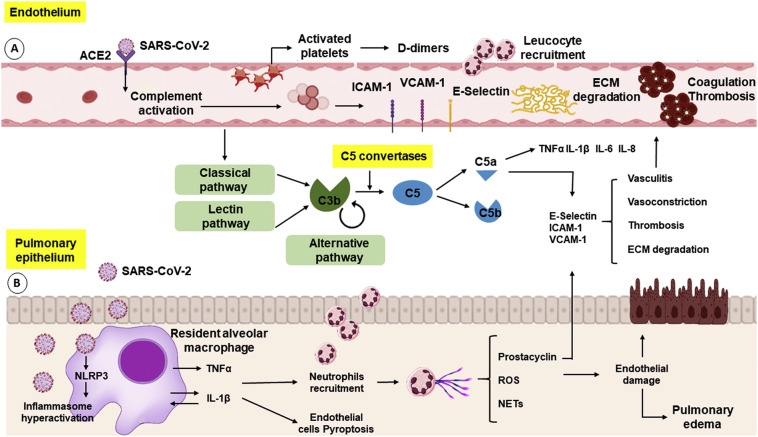
Fig. 1.
Endothelial cells and pulmonary epithelium in SARS-CoV-2 infection. (A) The binding of SARS-CoV-2 to the ACE2 receptor on EC leads to the activation of the complement system, a set of plasma proteins with opsonization functions in the immune system. The activation of the complement system induces pro-inflammatory cytokines release (e.g.: TNFα, IL-1β, IL-6, IL-8) and the recruitment of phagocytic cells. The release of these cytokines promotes the activation of the endothelium leading to the expression of selectins (E-selectin and P-selectin) and integrins (ICAM and VCAM) and promote the recruitment of neutrophils and monocytes, causing damage to the endothelium through the release of ROS, production of NETs, degradation of the extracellular matrix (ECM) and more pro-inflammatory cytokines release. The lesion in the endothelium induces the activation of the coagulation cascade and platelet activation leading to coagulation and thrombosis and increasing D-dimers formation. (B) The SARS-CoV-2 infection activates NLRP3, a cytosolic receptor in phagocyte cells, leading to the inflammasome, activating caspase 1 and exacerbating the production of IL-1β and TNFα, which in turn, lead to the recruitment of neutrophils, increased production of ROS and NETs, causing endothelial damage, pulmonary edema, and cell death.