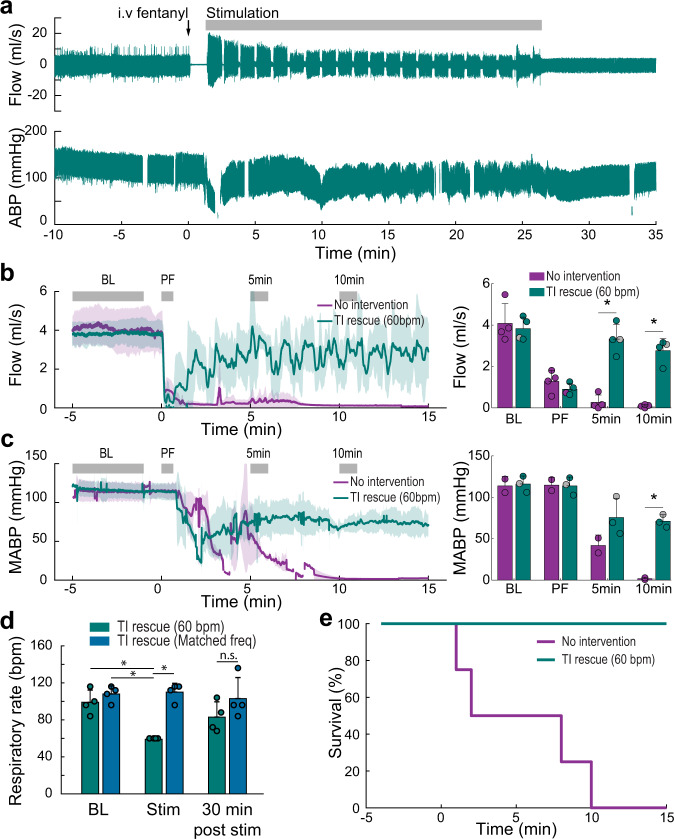
Fig. 2. Intramuscular TI stimulation (TI rescue) prevents fatal apnea by restoring diaphragm activation after opioid overdose.
Spontaneously breathing rats under urethane anesthesia received an intravenous injection of fentanyl (30 mcg/kg) sufficient to cause lasting respiratory suppression. Following fentanyl dosing, animals received intramuscular TI stimulation or no intervention. Panel a shows an example of sustained restoration of respiratory airflow when the stimulation was initiated shortly after opioid overdose-induced apnea, and was delivered with a pattern of 60 s on and 3 s off until spontaneous breathing resumed. Note: The gaps in the blood pressure traces indicate when arterial blood samples were taken. b Average respiratory airflow (two-way ANOVA: group F(1) = 40.84, p < 0.0001; time F(3) = 41.86, p < 0.0001; interaction F(3) = 21.4, p < 0.0001) and (c) mean arterial blood pressure (MABP) (n = 4 animals/group, two-way ANOVA: group F(1) = 19.81, p = 0.0008; time F(3) = 45.95, p < 0.0001; interaction F(3) = 7.82 p = 0.0037). The gray bars indicate time periods selected for quantitative comparison (Baseline–BL, immediately Post Fentanyl–PF, five minutes–5 min, and ten minutes–10 min after fentanyl). The gray dots indicate data points from the animals used for the example traces in panel a, (mean + 1 standard deviation; asterisk (*) indicates p < 0.05). d TI stimulation restored ventilation and prevented fatal apnea in all animals (TI rescue). TI stimulation with a 1 Hz beat frequency produced a respiratory rate of 60 breaths per minute (bpm) during stimulation. When the beat frequency was targeted to the endogenous respiratory rate, there was no difference in the evoked vs. spontaneous respiratory rate (n = 4 animals, two-way ANOVA: group F(1) = 22.64, p = 0.0002; time F(3) = 3.85, p = 0.0407; interaction F(3) = 5.03, p = 0.0183). e Survival curve for no-intervention (n = 4 animals) and TI rescue (60 bpm) conditions (n = 4 animals).