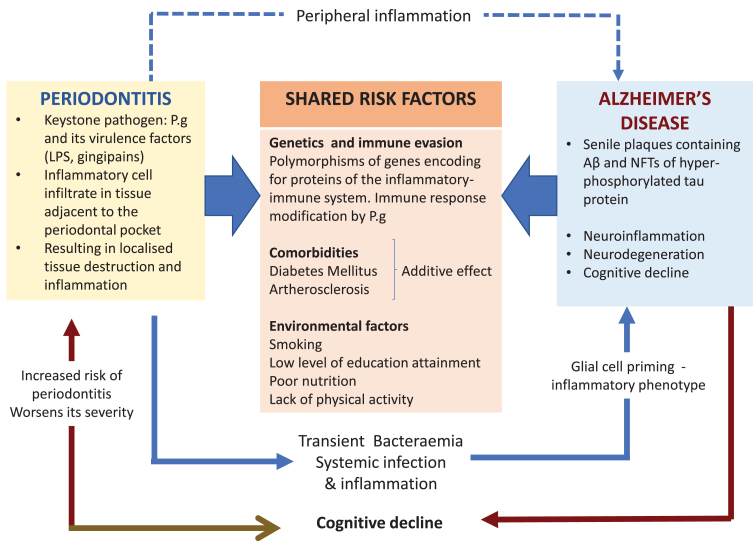
Fig. 1.
The keystone periodontal pathogen, P. gingivalis (P.g), can enter the bloodstream during episodes of transient bacteremia and gain access to the brain via multiple routes including a leaky blood-brain barrier. The microbial invasion triggers the cerebral immune response resulting in neuroinflammation and in the formation of the two diagnostic lesions of AD. Periodontitis can exert its influence indirectly by sustaining peripheral inflammation (blue dotted arrow). This can affect glial cells by priming them into a pro-inflammatory phenotype. In addition, this could also overload and overwhelm the clearing of toxic neuropeptides from the central nervous system (CNS). The potential causal relationship of periodontitis and AD is further supported by the shared risk factors.