Abstract
Introduction
To examine the impact of the COVID-19 pandemic on stroke, the number of stroke patients, time since last known well (LKW), morbidity, and mortality of stroke patients in Southwest Healthcare System (SHS), California (CA) and the United States (US) were analyzed during 2019 and compared to 2020. Our hypothesis is that there are regional differences in stroke outcome depending on location during the COVID-19 study period which influences stroke epidemiology and clinical stroke practice.
Methods
The American Heart Association's ‘Get with the Guidelines’ (GWTG) database was used to evaluate the following categories: code stroke, diagnosis of stroke upon discharge, inpatient mortality, modified Rankin Score (mRS) upon discharge (morbidity), and time since last known well (LKW). Stroke registry data from February through June 2019 and 2020 were collected for retrospective review.
Results
The total number of strokes decreased in the US and CA, but increased in SHS during the COVID-19 study period. The US and SHS demonstrated no change in stroke mortality, but CA demonstrated a higher stroke mortality during the COVID-19 pandemic. There was greater loss of independence with increased stroke morbidity in the US during the COVID-19 pandemic. There was a significant increase in time since LKW in the US and SHS, and an increase trend in time since LKW in CA during the COVID-19 study period.
Discussion
To understand the impact of the COVID-19 pandemic on stroke epidemiology, we propose that all stroke inpatients should receive a SARS-CoV-2 detection test and this result be entered into the GWTG database. We demonstrate that the regional distribution of stroke mortality in the US changed during the COVID-19 study period, with increased stroke mortality in CA. Stroke morbidity throughout the US was significantly worse during the COVID-19 pandemic. We propose methods to address the impact of the COVID-19 pandemic on clinical stroke practice such as the use of mobile stroke units, clinical trials using anti-inflammation drugs on SARS-CoV-2 positive stroke patients, and COVID stroke rehabilitation centers.
Key Words: COVID-19, SARS-CoV-2, Epidemiology, Ischemic stroke, Stroke mortality, Stroke, Morbidity
Introduction
The challenges brought on by the coronavirus disease 2019 (COVID-19) have been unprecedented. Since the United States (US) index case of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) appeared on January 19, 2020 in Snohomish County, Washington, there has been a logarithmic increase in diagnosed cases and over 350,000 attributable deaths in the US.1 On March 11, 2020, the World Health Organization declared COVID-19 a worldwide pandemic.2 Patients with COVID-19 have presented with headaches, neurological deficits, cerebral large vessel occlusion, and cerebral ischemia with encephalitis.3 , 4 Thrombosis with COVID-19 associated vascular inflammation of the medium and large cerebral vessels may contribute to stroke.5 Systemic cytokine and interleukin responses appear to play a role in the inflammatory response brought on by SARS-CoV-2.6 Furthermore, dysfunction of coagulation such as disseminated intravascular coagulation and thrombocytopenia has been found to increase the likelihood of embolic events resulting in cerebral ischemia in SARS-CoV-2 positive patients.7
Public fear regarding the COVID-19 pandemic is real and has altered behaviors which potentially can affect the delivery of critical medical treatments offered by emergency medical services and hospital systems.8 According to the New England Journal of Medicine, daily counts of patients presenting with stroke symptoms decreased in March of 2020.9 The American Stroke Association reported a decrease in emergency visits for stroke treatment during the global pandemic.2
To understand the regional effects of the COVID-19 pandemic on stroke outcomes, we studied the total number of strokes, times since last known well (LKW), morbidity and mortality of stroke patients in our regional Southwest Healthcare System (SHS) stroke program, California (CA), and the United States (US). We compared data from 2019 with equivalent data from 2020. Our hypothesis is that there are regional differences in stroke depending on location which will influence stroke epidemiology and clinical stroke practice during the COVID-19 study period.
Methods
We analyzed the American Heart Association's ‘Get with the Guidelines’ (GWTG) shared stroke registry dataset. SHS stroke data was entered originally by our data-entry technicians. Data used to represent CA or the US were entered independently by primary and comprehensive stroke centers in the stroke registry GWTG database. Data from February, March, April, May and June 2020 was used as an aggregate dataset and referred to as the COVID-19 study period. Data from February, March, April, May and June 2019 was used as an aggregate dataset and referred to as the time period prior to the COVID-19 pandemic.
Demographics were collected including age, gender, race, and National Institutes of Health Stroke Score (NIHSS) in 2019 and 2020. There were no significant differences in each of these categories. Patients with a discharge diagnosis of stroke and code stroke patients were identified to analyze total number of stroke patients admitted to the hospital. LKW was recorded in minutes. Modified Rankin Scores (mRS) were extracted from patients who had a discharge diagnosis of stroke. Modified RS score of 6 was death and used to determine overall mortality. Patients with a mRS of 0-3 were considered independent, whereas mRS 4-5 were considered dependent. Independence was determined to be mobility without necessary assistance. All mRS numbers were obtained at discharge.
Statistical analysis
The study design is a retrospective, unspecified analysis of data for primary and comprehensive stroke centers. Total numbers of patients from February through June 2019 and February through June 2020 were extracted from the stroke registry GWTG database to analyze code stroke, discharge diagnosis of stroke, mRS 6 (mortality), and mRS 0-3 (morbidity). The median number of minutes since LKW from February through June 2019 and February through June 2020 were extracted from the GTWG stroke registry. A stratified analysis of total numbers of code strokes, discharge diagnosis of stroke, mRS 6, mRS 0-3 and median numbers since LKW from February through June 2019 were compared to February through June 2020 using independent two-sample T tests. The threshold for statistical significance was set at a p-value less than .05. Statistical analyses were carried out using SAS 9.4 Software (Cary, NC).
Results
Total number of stroke patients
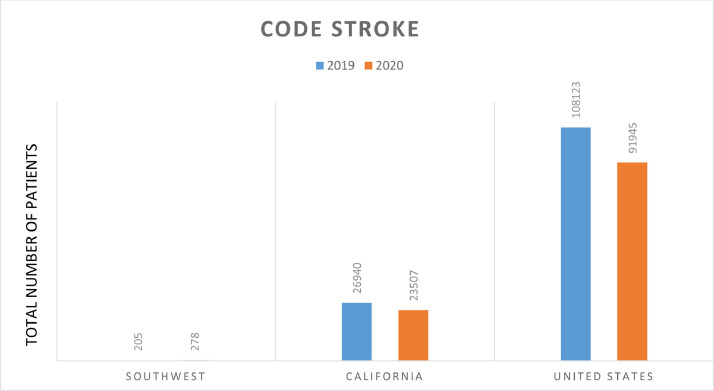
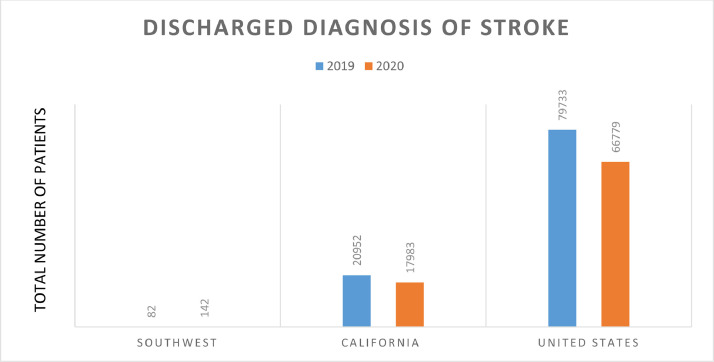
Code stroke and discharge diagnosis of stroke were used to identify stroke in the GWTG dataset. Fig. 1 demonstrates the total number of code stroke patients from February through June 2019, and were compared to the equivalent months in 2020. Fig. 2 demonstrates the total number of patients discharged with stroke diagnosis from February through June 2019 and was compared to 2020. SHS demonstrated an increase in the total number of code stroke patients and an increase in total number of patients discharged with diagnosis of stroke in 2020, compared to 2019 (p=.007 and p=0.0012, respectively). California demonstrated a decrease in the total number of code stroke patients and a decrease in the total number of patients discharged with the diagnosis of stroke in 2020, compared to 2019 (p=.02 and p=0.0267, respectively). The US demonstrated a decrease in the total number of code stroke patients and a decrease in total number of patients discharged with diagnosis of stroke in 2020, compared to 2019 (p=.01 and p=0.015, respectively).
Fig. 1.
Total number of code stroke patients from February through June 2019 compared to 2020. Significant decrease for CA and the US.
Fig. 2.
Total number of patients discharged with stroke diagnosis from February through June 2019, compared to 2020. Significant decrease for CA and the US.
Outcomes: mortality
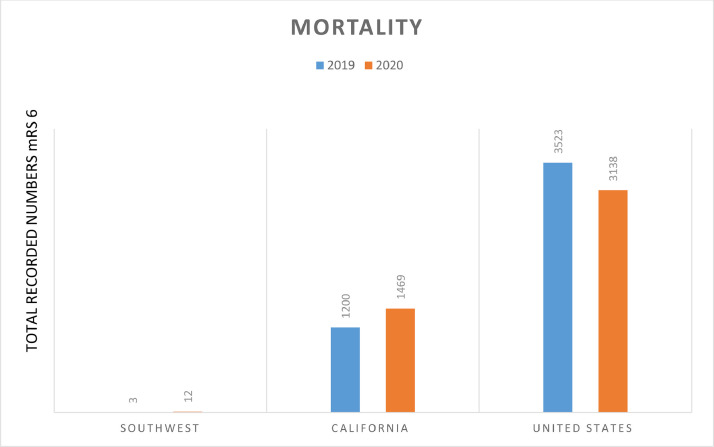
Mortality was determined by evaluating patients with mRS 6 (death) in the GWTG database. Fig. 3 shows the total number of patients recorded with mRS 6 from February through June 2019, compared to 2020. There was no statistical difference in mRS 6 at SHS or the US from 2019 to 2020 (p=0.329 and p=0.3, respectively). However, there was a significant increase in mortality in CA during the COVID-19 pandemic, compared to 2019 (p=.0005).
Fig. 3.
Total patients recorded with mRS 6 (death) from February through June 2019, compared to 2020. No significant differences demonstrated in SHS or the US. Significant increase in mortality in CA during the 2020 COVID-19 pandemic.
Outcomes: morbidity
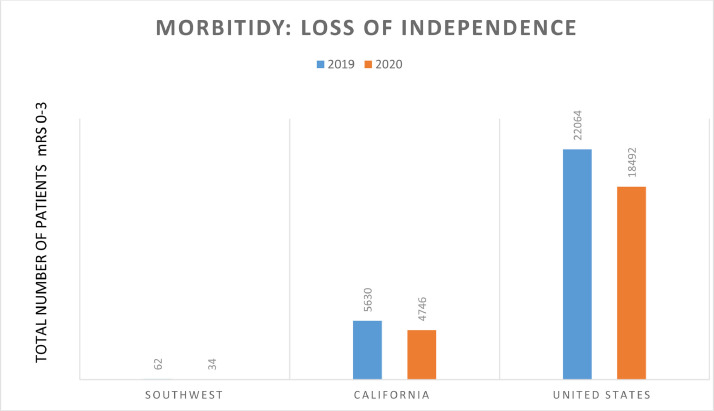
Morbidity was determined by a loss of independence. A decrease in mRS 0-3 was defined as a loss of independence. Fig. 4 demonstrates total patients with mRS 0-3 from February through June 2019, compared to 2020. There were no significant differences in mRS 0-3 at SHS and CA during the COVID-19 pandemic, compared to 2019 (p=0.3, p=0.4, respectively). There was a significant decrease in mRS 0-3 in the US during the COVID-19 pandemic, compared to 2019 (p=.018).
Fig. 4.
Total patients with mRS 0-3 from February through June 2019, compared to 2020. Significant decrease in amount of independent patients in the US. No significant changes seen in SHS or CA.
Time since LKW
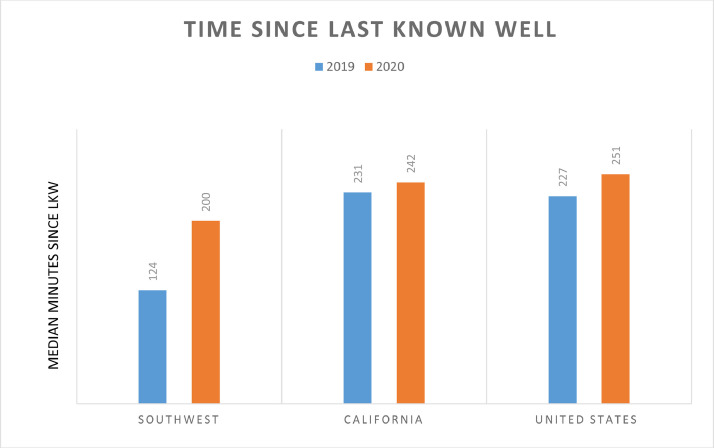
The median number of minutes since LKW February through June 2019 was compared to 2020 in Fig. 5 . SHS and the US demonstrated a significant increase in the median number of minutes since LKW during the COVID-19 pandemic, compared to 2019 (p=.03 and p=.012, respectively). In CA, there was a non-significant trend increase in the median minutes since LKW during the COVID-19 pandemic, compared to 2019 (p=0.125).
Fig. 5.
Median minutes since LKW during 2020 COVID-19 pandemic, compared to 2019. Significant increase in minutes since LKW for SHS and the US. Non-significant trend increase in median minutes since LKW in CA during 2020 COVID-19 pandemic, compared to 2019.
Discussion
The COVID-19 pandemic has been associated with unprecedented morbidity and mortality worldwide. We report that there were significantly decreased strokes, no significant increase in stroke mortality, and a significant increase in stroke morbidity with greater loss of independence during the COVID-19 study period in the US. In CA, we identified a significant increase in stroke mortality with no change in morbidity despite having significantly fewer stroke admissions statewide. In our region of southern CA, SHS experienced a greater number of strokes along with no change in mortality or morbidity.
Decreased hospital admissions for stroke during the COVID-19 pandemic has been reported. Clinical investigators in Piacenza, Italy experienced deceased number of strokes per month from 51 to 6 during the onset of the COVID-19 pandemic.10 Even though SHS demonstrated an increase in the number of strokes, we believe this was a result of diversion of patients from a neighboring hospital which closed their stroke program in January 2020. Speculation that SARS-CoV-2 infection would lead to increased strokes ensued because other viral illness leading to Influenza Pneumonia has been associated with increased stroke rates.11 There is no data to suggest that SARS-CoV-2 infection lowers the stroke rate. Nonetheless, the GWTG dataset during the months of February through June 2020 demonstrated a decreased stroke rate during the COVID-19 pandemic in the US and CA. There are several ways to interpret this data. Deceased stroke hospitalization rates could potentially be a result of increased prehospital stroke mortality. Also, fear of infection at the hospital may have prevented individuals from traveling to the hospital for care. GWTG database is unable to account for stroke-like symptoms reported to outpatient primary care clinics. Possibly an outpatient GWTG registry may be developed for primary care physicians to report stroke symptoms in patients with COVID-19 who refuse to go to the hospital. An aggressive public education campaign should be considered to encourage patients with stroke-like symptoms to seek immediate hospital attention. In addition, it is possible that patients who present to the hospital with both respiratory symptoms and mild neurological deficits are being triaged for their respiratory symptoms alone, leading to under-reporting of stroke in the hospital. Furthermore, oxygen requirements create significant challenges during transportation and acquisition of neuroimaging, which may impede the diagnosis of stroke. Implementation of a robust mobile stroke unit program covered by medical insurance may improve access to stroke care and improve clinical stroke practice outcomes for patients who refuse to obtain an evaluation in the Emergency Department.
The incidence of stroke in the COVID-19 population will be determined when each code stroke patient receives the SARS-CoV-2 detection test. From February through June 2020, SARS-CoV-2 detection testing was not common due to lack of test availability. In the later part of 2020, some hospitals adopted a policy of universal inpatient SARS-CoV-2 testing. SARS-CoV-2 detection testing performed on all code stroke patients would allow us to analyze the incidence, distribution, and control of stroke in the patients with COVID-19. Once SARS-CoV-2 detection is incorporated into the GWTG database, the impact of SARS-CoV-2 infection on the epidemiology of stroke will be discoverable.
Increased mortality in CA suggests that the impact of COVID-19 on stroke is distributed unequally throughout the US. It is difficult to postulate exactly why stroke mortality is increased in CA and not in the entire US. Risk factors and clinical practice patterns in CA should be analyzed in further investigation and compared to states which has a lower mortality. A mortality analysis on all states through the end of 2020 would further detail the impact of COIVD-19 on the distribution of stroke mortality in the US. It would be important to see whether or not the increase in mortality in CA is sustained throughout 2020.
During the time period from February through June 2020, we identified a significant increase in disability in the US which we termed ‘loss of independence’. There were significantly fewer patients discharged as mRS 0-3, which indicates that stroke survivors suffered significantly greater disabling neurological deficits. It is possible that neurovascular inflammation associated with COVID-19 increased the severity of stroke, giving rise to a greater loss of independence seen in the US. The COVID-19 inflammatory cascade occurs when SARS-CoV-2 Spike (S) glycoprotein binds to the angiotensin converting enzyme 2 (ACE2) on the cell surface of respiratory epithelium. This interaction downregulates the alternative renin-angiotensin system (RAS), and upregulates the classical RAS pathway associated with inflammation.12 Drugs such as angiotensin receptor blockers have been shown to reduce the risk of stroke through inhibition of the classical RAS inflammatory cascade.13 However, angiotensin receptor blockers have also been shown to upregulate ACE2 receptor expression, which may increase the infectivity of SARS-CoV-2. Clinical studies are currently underway to test the effects of angiotensin receptor blockers on patients with active SARS-CoV-2 infection. Perhaps in regions with higher stroke mortality such as CA, it would be reasonable to perform clinical investigation with angiotensin receptor blockers in combination with intravenous thrombolytics or endovascular thrombectomy as treatment for COVID-19 stroke patients.
Furthermore, a generalized ‘loss of independence’ throughout the country may be due to challenges associated with rehabilitation of the stroke patient. Inpatient physical therapy may be limited by oxygen requirements and the small size of a negative pressure isolation room. Devices used for lifting or standing upright may be unavailable due to cross-contamination risk. Stroke patients are experiencing significant delays in being transferred to rehabilitation. Skilled nursing homes (SNF) do not accept COVID-19 patients and require two negative SARS-CoV-2 tests prior to acceptance to the facility. Delays in obtaining critical rehabilitation services may result in a worse mRS at discharge. The development of a COVID-19 rehabilitation center for stable COVID-19 stroke patients may open up much needed hospital beds and potentially improve stroke morbidity nationwide. It is important to note that mRS data on GWTG database is recorded in approximately 50% of stroke patients entered into the database. Accuracy in reporting morbidity would increase with greater numbers of mRS entered into the database.
We validated prior claims that there was an increase in time since LKW in the US.14 Delay in hospital presentation places patients in jeopardy of falling out of the window for intravenous thrombolytic or endovascular treatment. Delays in LKW may have contributed to increased loss of independence in the US. SHS demonstrated significant increases in time since LKW, but did not see an increase in loss of independence. This demonstrates that the impact of COVID-19 on the epidemiology of stroke is multifactorial. Risk factors affecting stroke outcome may be related to the infection itself or to the social consequences of the COVID-19 pandemic.
Further investigation of the GWTG database is necessary to examine the impact of COVID-19 on stroke morbidity and mortality from the months of July through December 2020. Analysis of stroke mortality in all fifty states would allow us to understand the distribution of stroke risk in the US associated with the COVID-19 pandemic. We identify that marketing and education to encourage patients to obtain emergency stroke treatment is needed now more than ever. Possibly development of a robust mobile stroke unit fleet is in order if patients continue to refuse care or delay reporting to the hospital. Furthermore, we propose that all stroke inpatients should be tested for SARS-CoV-2 and results should entered into the GWTG database to learn the impact of SARS-CoV-2 infection on stroke epidemiology. Finally, we identify nationwide increases in loss of independence after stroke during the COVID-19 pandemic. Clinical trials examining the use of angiotensin receptor blockers for COVID-19 stroke patients and the development of COVID-19 stroke rehabilitation centers may be considered to address the impact of COVID-19 on clinical stroke practice.
Disclosures
There are no disclosures for any of the authors listed in this article.
References
- 1.Holshue M, DeBolt C, Lindquist S, Lofy K, Wiesman J, Bruce H, Spitters C, Ericson K, Wilkerson S, Tural A, Diaz G, Cohn A, Fox L, Patel A, Gerber S, Kim L, Tong S, Lu X, Lindstrom S, Pallansch M, Weldon W, Biggs H, Uyeki T, Pillai S. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929–936. doi: 10.1056/NEJMoa2001191. Epub 2020 Jan 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Heart Association/American Stroke Association Stroke Council Leadership Temporary emergency guidance to US stroke centers during the COVID-19 pandemic. Stroke. 2020;51:1910–1912. doi: 10.1161/STROKEAHA.120.030023. [DOI] [PubMed] [Google Scholar]
- 3.Zayet S, Klopfenstein T, Kovacs R, Stancescu S, Hagenkotter B. Acute cerebral stroke with multiple infarctions and COVID-19. Emerg Infect Dis. 2020;26(9):2258–2260. doi: 10.3201/eid2609.201791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zulgarnain I, Balson L, Madathil S. Massive bilateral stroke in a Covid-19 patient. BMJ Case Rep CP. 2020;13 doi: 10.1212/WNL.0000000000009713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk BM, Hoh B, Jauch EC, Kidwell CS, Leslie-Mazwi TM, Ovbiagele B, Scott PA, Sheth KN, Southerland AM, Summers DV, Tirschwell DL. 2018 Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American heart association/American stroke association. Stroke. 2018;49(3):e46–e99. doi: 10.1161/str.0000000000000158. [DOI] [PubMed] [Google Scholar]
- 6.Kempuraj D, Selvakumar G, Ahmed M, Raikwar S, Thangavel R, Khan A, Burton C, James D, Zaheer A. COVID-19, mast cells, cytokine storm, psychological stress, and neuroinflammation. Neuroscientist. 2020;26(5-6):402–414. doi: 10.1177/1073858420941476. [DOI] [PubMed] [Google Scholar]
- 7.Barrios-Lopez J, Rego-García I, Muñoz Martínez C, Romero-Fábrega J, Rodríguez Rivero, M Ruiz Giménez J, Escamilla-Sevilla F, Mínguez-Castellanos A, Fernández Pérez M. Ischemic stroke and SARS-CoV-2 infection: a causal or incidental association? Neurologia. 2020;35(5):295–302. doi: 10.3201/eid2609.201791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bullrich M, Fridman S, Mandzia J, Mai L, Khaw A, Vargas Gonzalez J, Bagur J, Sposato L. COVID-19: Stroke admissions, emergency department visits, and prevention clinic referrals. Can J Neurol Sci. 2020;47(5):693–696. doi: 10.1017/cjn.2020.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral effect of Covid-19 on stroke evaluation in the United States. N Engl J Med. 2020;383(4):400–401. doi: 10.1056/NEJMc2014816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morelli N, Rota E, Terracciano C, Immovilli P, Spallazzi M, Colombi D, Zaino D, Michieletti E, Guidetti D. The battling case of ischemic stroke disappearance from the casualty department in the COVID-19 era. Eur Neurol. 2020;83(2):213–215. doi: 10.1159/000507666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Warren-Gash C, Blackburn R, Whitaker H, McMenamin J, Hayward AC. Laboratory-confirmed respiratory infections as triggers for acute myocardial infarction and stroke: a self-controlled case series analysis of national linked datasets from Scotland. Eur Respir J. 2018;51(3) doi: 10.1183/13993003.01794-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Divani AA, Andalib S, Di Napoli M, Lattanzi S, Hussain M.S, Biller J, McCullough LD, Azarpazhooh MR, Seletska A, Mayer SA, Torbey M. Coronavirus disease 2019 and stroke: clinical manifestations and pathophysiological insights. J Stroke Cerebrovasc Dis. 2020;29(8) doi: 10.1016/j.jstrokecerebrovasdis.2020.104941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Keating G. Losartan/hydrochlorothiazide: a review of its use in the treatment of hypertension and for stroke risk reduction in patients with hypertension and left ventricular hypertrophy. Drugs. 2009;69(9):1239–1265. doi: 10.2165/00003495-200969090-00008. [DOI] [PubMed] [Google Scholar]
- 14.Schirmer CM, Ringer AJ, Arthur AS, Binning MJ, Fox WC, James RF, Levitt MR, Tawk RG, Vaznedaroglu E, Walker M, Spiotta AM, Endovascular Research Group (ENRG) Delayed presentation of acute ischemic strokes during the Covid-19 crisis. J Neurointerv Surg. 2020;12(7):639–642. doi: 10.1136/neurintsurg-2020-016299. [DOI] [PubMed] [Google Scholar]