Abstract
Objective
To measure the extent to which the provision of mammograms was impacted by the COVID‐19 pandemic and surrounding guidelines.
Data Sources
De‐identified summary data derived from medical claims and eligibility files were provided by Independence Blue Cross for women receiving mammograms.
Study Design
We used a difference‐in‐differences approach to characterize the change in mammograms performed over time and a queueing formula to estimate the time to clear the queue of missed mammograms.
Data Collection
We used data from the first 30 weeks of each year from 2018 to 2020.
Principal Findings
Over the 20 weeks following March 11, 2020, the volume of screening mammograms and diagnostic mammograms fell by 58% and 38% of expected levels, on average. Lowest volumes were observed in week 15 (April 8 to 14), when screening and diagnostic mammograms fell by 99% and 74%, respectively. Volumes began to rebound in week 19 (May), with diagnostic mammograms reaching levels to similar to previous years’ and screening mammograms remaining 14% below expectations. We estimate it will take a minimum of 22 weeks to clear the queue of missed mammograms in our study sample.
Conclusions
The provision of mammograms has been significantly disrupted due to the COVID‐19 pandemic.
Keywords: COVID‐19, early detection of cancer, mammography, missed diagnosis, preventive medicine
What is Known on This Topic
Mammograms are widely used to detect and diagnose breast cancer in women.
The COVID‐19 pandemic has disrupted the provision and delivery of medical care.
The extent to which the provision of mammograms—a particular type of preventive care—has been impacted is unknown.
What This Study Adds
The provision of routine screening mammograms dropped by 99% by early April 2020, began to rebound in May, and reached a level of 14% below expectations by the end of July.
Diagnostic mammograms, performed when breast cancer might be suspected, decreased by 74% by early April, and then rebounded to levels on par with previous years by the end of July.
Estimations based on queueing principles suggest that a minimum of 22 weeks will be needed to clear the queue of missed mammograms; in the worst‐case scenario, demand will exceed capacity by so much that the queue will continue to grow.
1. INTRODUCTION
The ongoing COVID‐19 pandemic has transformed the provision and delivery of medical care. Between March 15 and March 30, 2020, 34 states enacted social distancing orders prohibiting nonessential and elective medical procedures. 1 Many of these orders also restricted nonessential travel of individuals, including travel to nonurgent medical appointments. On April 7, 2020, both the Centers for Disease Control and Prevention (CDC) and the Centers for Medicare and Medicaid Services (CMS) published guidelines recommending the postponement of nonurgent procedures, including preventive care screenings. 2 , 3
These guidelines directly affected screening mammograms, which are widely used to detect early‐stage breast cancer in asymptomatic women. In 2018, 72.8% of women aged 50 to 74 (nearly 35 million women in the United States) received a mammogram within the past 2 years. 4
In addition to the routine screening of women without symptoms, mammography is also used for the diagnostic evaluation of women who feel a palpable mass in the breast or had a previously abnormal screening result. 5 These diagnostic mammograms happen less frequently, averaging to about 1.7 million annually. 6 Compared to those who first have a screening mammogram that is then followed by a diagnostic mammogram, women who are diagnosed with breast cancer after having received only a diagnostic mammogram are more likely to be diagnosed with regional and metastatic breast cancers 7 ; such cancers diagnosed at more advanced stages are typically followed by more aggressive treatments.
In this study, we analyzed the effects of the COVID‐19 pandemic on the provision of mammograms. Using data from a private health insurer, Independence Blue Cross (Independence), we documented the extent to which the provision of mammograms was impacted by the pandemic and its surrounding guidelines, differentiating between screening and diagnostic mammograms. We also developed estimates around how long it may take to clear the queue of missed mammograms attributable to the pandemic.
2. METHODS
2.1. Data
De‐identified summary data derived from medical claims and eligibility files were provided by Independence for women aged 40 years and older receiving screening mammograms and diagnostic mammograms since 2018. All data on patient demographics and prior cancer diagnoses also came from Independence.
Data on mammograms performed between the first 30 weeks of 2018, 2019, and 2020 (ending July 28, 2020), inclusive, using claims data posted by August 31, 2020, were used for analysis. We limited our sample to mammograms performed during or before week 30 of 2020 to account for claims lag, which occurs because some claims may take several weeks to post after the service is delivered. Additionally, we chose week 30 as the cutoff based on Independence's historical data, which shows that 95% of claims are posted within 4 weeks of the mammogram being performed.
Screening mammograms and diagnostic mammograms were identified using the Healthcare Common Procedure Coding System (HCPCS) procedure codes. When a single claim included codes for both types of mammograms, we followed Independence's approach of classifying the claim as a screening mammogram; in these cases, providers may have detected a suspicious finding on the initial screening mammogram and then proceeded with a more in‐depth examination during the same visit.
2.2. Analytic approach
First, we compared the characteristics of women receiving screening and diagnostic mammograms before and after the beginning of the COVID‐19 pandemic. We defined the pre period as the first 30 weeks of 2018, the first 30 weeks of 2019, and the first 10 weeks of 2020; the post period was defined as weeks 11 to 30 of 2020. We set the post period to begin in week 11 of 2020 since that is when the WHO declared COVID‐19 to be a pandemic, 8 the US President declared a national emergency, 9 the United States surpassed 1000 cases, 10 and many states began to enact social distancing orders. In Pennsylvania, where 78% of our sample is drawn from, this is the week when the Governor announced the closure of schools and suspension of large gatherings. 11 A statewide nonessential business closure order was enacted the following week, along with guidance for health care providers to suspend nonurgent and elective care. 12 The delivery of these health care services was allowed to resume on May 9 (week 19). 13
Next, we characterized the change in the volume of screening mammograms and diagnostic mammograms conducted over time. We estimated the volume of weekly mammograms over weeks 1 to 30 of 2018, 2019, and 2020, controlling for year‐specific effects as well as seasonality in the provision of mammograms in weeks 11 to 30 compared to weeks 1 to 10. Specifically, our regression model is given by:
| (1) |
where is an indicator that equals one if the week is in the 11th week of the year or later. Since women with a prior diagnosis of breast cancer may have been impacted differently than those without, we repeated this estimation on a stratified sample of women with versus without a prior diagnosis of breast cancer. Then, we calculated the percent reduction in mammograms utilization during weeks 11 to 30 of 2020 as follows:
| (2) |
where captures the expected volume of mammograms that would have occurred in the absence of the pandemic.
Finally, we estimated how long it may take for women who missed a mammogram (of either type) during weeks 11 to 30 of 2020 to receive one. To do so, we applied the following basic queueing formula for cases in which demand exceeds capacity:
| (3) |
Here, equals the total number of missed mammograms, which can be calculated as . To account for a best‐case versus worst‐case scenario, we used an upper bound and lower bound of , which we estimated by assuming that (a) the post‐week 30 capacity is reduced by 10% (best case) or 50% (worst case) to accommodate social distancing guidelines and additional cleaning protocols, but (b) hours of operation are extended by 25% (worst case) or 50% (best case) per week, and (c) weekly demand going forward remains at the levels observed at week 30. 14 Hence, capacity may be as low as 62.5% to as high as 135% of prepandemic levels, before accounting for the baseline weekly demand after week 30. To estimate prepandemic capacity, we assumed that the maximum number of weekly mammograms (of either type) observed in 2019 reflects the capacity (ie, 100% utilization).
3. RESULTS
Table 1 compares the characteristics of women receiving screening and diagnostic mammograms before and after the beginning of the COVID‐19 pandemic. Among women receiving screening mammograms, those who received one after March 11, 2020, tended to be slightly older, had more time elapse between the current and previous mammogram, and were more likely to have a previous breast cancer diagnosis compared to those who received one before then. Among women receiving diagnostic mammograms, those who received one after March 11, 2020, had more time elapse between the current and previous mammogram and were more likely to have a previous breast cancer diagnosis but did not meaningfully differ in age compared to those who received one before then.
TABLE 1.
Summary statistics of women receiving mammograms before and after March 11, 2020
| Screening mammograms | Diagnostic mammograms | |||||
|---|---|---|---|---|---|---|
| 1/1/2018‐3/10/2020 | 3/11/2020‐7/28/2020 | P‐value of difference | 1/1/2018‐3/10/2020 | 3/11/2020‐7/28/2020 | P‐value of difference | |
| Member‐level characteristics | ||||||
| Age | ||||||
| % 40‐49 | 26.32 | 25.12 | <.0001 | 30.44 | 29.95 | .33 |
| % 50‐59 | 37.31 | 37.09 | .49 | 31.86 | 31.38 | .34 |
| % 60‐69 | 26.72 | 28.04 | <.0001 | 23.37 | 24.61 | .007 |
| % 70+ | 9.66 | 9.74 | .66 | 14.33 | 14.06 | .48 |
| Time since previous mammogram (days) a | ||||||
| 40‐49 | 437 (125) | 497 (195) | <.0001 | 155 (182) | 212 (215) | <.0001 |
| 50‐59 | 437 (124) | 488 (178) | <.0001 | 171 (178) | 237 (225) | <.0001 |
| 60‐69 | 430 (117) | 482 (175) | <.0001 | 191 (180) | 252 (222) | <.0001 |
| 70+ | 420 (108) | 461 (150) | <.0001 | 242 (178) | 290 (212) | <.0001 |
| % Prior breast cancer diagnosis | 1.65 | 2.29 | <.0001 | 15.62 | 18.42 | <.0001 |
| % Prior cancer diagnosis, non‐breast cancer b | 0.83 | 0.88 | .45 | 1.02 | 1.08 | .56 |
| Average weekly mammograms | 3045.26 | 1398.50 | <.0001 | 798.27 | 511.65 | <.0001 |
| Total mammograms | 213,168 | 27,970 | 55,879 | 10,233 | ||
Based on claims posted as of August 31, 2020, for mammograms performed in the first 30 weeks of each year.
Data only available for subset of women for whom we observe a previous mammogram. We observe a previous mammogram for 64.21% of screening mammograms, 82.60% of diagnostic mammograms, and 68.47% of all mammograms.
Non‐breast cancers include colorectal cancer, endometrial cancer, lung cancer, and prostate cancer.
Figure 1 plots the change in the weekly count of screening mammograms (panel (a)) and diagnostic mammograms (panel (b)) conducted over the first 30 weeks of the year in 2018, 2019, and 2020. Trends in weeks 1 to 10 are similar across the three years, with a slight increase in level of mammograms conducted in 2020. Trends in weeks 11 to 30 are also similar in 2018 and 2019, with predictable dips in utilization during weeks with major holidays (Memorial Day in week 22 and Independence Day in week 27). In week 11 of 2020, we observe the beginning of a marked reduction in mammograms, with the weekly count of screening mammograms falling to almost none in weeks 13 to 16; diagnostic mammograms also drop substantially but not to levels that are quite as low. The volume of both types of mammograms began to gradually recover starting in week 19. By week 27, the volume of diagnostic mammograms has rebounded close to levels observed in previous years, while the volume of screening mammograms remained approximately 14% below expected levels.
FIGURE 1.
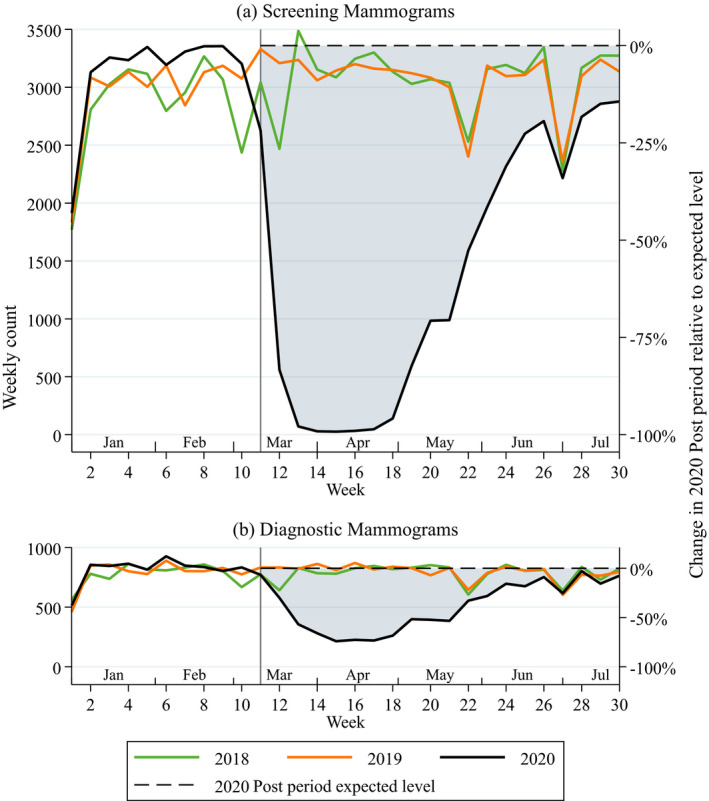
Trends in count of weekly mammograms in weeks 1 to 30 of the year. Notes. Based on claims posted as of August 31, 2020, for mammograms performed in the first 30 weeks of each year. Week 11 (vertical gray line) indicates the beginning of the post period. Dotted horizontal line shows the expected volume of mammograms that would have occurred during the post period in 2020 in the absence of the COVID‐19 pandemic. Shaded region captures missed mammograms during the post period in 2020. [Color figure can be viewed at wileyonlinelibrary.com]
To quantify the magnitude of this decrease and obtain estimates of missing mammograms, we estimate Equation (1) and present the results in Table 2. We find that the slight increase in mammogram utilization observed in the first 10 weeks of 2020 is not statistically significant, but the drop in utilization during weeks 11 to 30 of the same year is highly significant ( = −1961 for screening mammograms (P < .001); =−314 for diagnostic mammograms (P < .001)). From Equation (2), we find that this corresponds to a 58% (95% CI: 42%‐74%) reduction in screening mammograms and a 38% (95% CI: 25%‐51%) reduction in diagnostic mammograms on average across the 20‐week period, relative to the expected volume of mammograms that would have occurred during this period in the absence of the pandemic (ie, dashed line in Figure 1). At the weekly level, mammogram utilization reached their lowest levels in week 15, at which point screening mammograms fell by 99.2% (95% CI: 99.1%‐99.3%) and diagnostic mammograms fell by 74% (95% CI: 71%‐77%), relative to expected levels.
TABLE 2.
Impact of the COVID‐19 pandemic on weekly count of mammograms performed
| All women | Women with prior diagnosis of breast cancer | Women without prior diagnosis of breast cancer | ||||
|---|---|---|---|---|---|---|
| Screening | Diagnostic | Screening | Diagnostic | Screening | Diagnostic | |
| Year 2019 | 108.90 | 11.30 | −0.20 | 3.00 | 109.10 | 8.30 |
| (186.40) | (47.27) | (5.12) | (9.61) | (182.54) | (38.99) | |
| Year 2020 | 290.10 | 41.20 | 3.60 | 9.60 | 286.50 | 31.60 |
| (192.56) | (45.10) | (5.69) | (8.13) | (187.90) | (38.52) | |
| Post | 230.10 | 12.35 | 1.35 | 12.00+ | 228.75 | 0.35 |
| (153.72) | (33.66) | (4.30) | (7.20) | (150.19) | (28.08) | |
| Year 2019 x Post | −101.15 | 0.50 | 0.55 | −0.00 | −101.70 | 0.50 |
| (206.43) | (52.33) | (5.78) | (10.79) | (202.20) | (43.33) | |
| Year 2020 x Post | −1961.30*** | −314.40*** | −21.65* | −41.15** | −1939.65*** | −273.25*** |
| (330.31) | (67.36) | (8.22) | (12.86) | (323.19) | (57.11) | |
| Constant | 2839.60*** | 772.50*** | 48.70*** | 113.80*** | 2790.90*** | 658.70*** |
| (137.64) | (29.17) | (3.89) | (6.40) | (134.32) | (23.96) | |
| Observations | 90 | 90 | 90 | 90 | 90 | 90 |
| R‐squared | 0.56 | 0.48 | 0.22 | 0.22 | 0.56 | 0.51 |
| % change in 2020 Post period relative to expected levels | −58.38*** | −38.06*** | −40.35*** | −30.39*** | −58.67*** | −39.56*** |
| (8.128) | (6.751) | (12.44) | (8.281) | (8.084) | (6.767) | |
| Mammograms missed in 2020 Post period | −39,226*** | −6,288*** | −433*** | −823*** | −38,793*** | −5,465*** |
| (6606) | (1347) | (164.4) | (257.2) | (6464) | (1142) | |
Based on claims posted as of August 31, 2020, for mammograms performed in the first 30 weeks of each year. Baseline year is 2018 and baseline weeks are the first 10 weeks of the year. Post refers to weeks 11 to 30 of the year. Robust standard errors are reported in parentheses. *P < .05, **P < .01, ***P < .001.
A stratified analysis shows that while this reduction in mammogram utilization was experienced by both women with or without a prior diagnosis of breast cancer, the average percent reduction was less among women with a prior diagnosis of breast cancer (a decrease of 40% (95% CI: 16%‐65%) for screening mammograms and 30% (95% CI: 14%‐47%) for diagnostic mammograms) compared to those without (59% (95% CI: 43%‐74%) for screening mammograms and −40% (95% CI: 26%‐53%) for diagnostic mammograms).
Using the estimates of for screening and diagnostic mammograms, respectively, we find that there were approximately 45,500 (95% CI: 30,100‐61,000) total missed mammograms over the course of the 20‐week post period. Assuming prepandemic capacity to be 4,200 mammograms per week, we would expect to be able to accommodate 2,630 (worst case) to 5,670 (best case) mammograms per week after week 30, before accounting for a baseline weekly demand of 3,640 in this period. Using Equation (3), we then estimate that, in the best‐case scenario, it will take 22 weeks to clear the queue of patients whose mammograms were missed or delayed. In the worst‐case scenario, demand will exceed capacity by so much that the queue will continue to grow.
4. DISCUSSION
The effect of COVID‐19 on breast cancer screenings has been dramatic. We show that, over the course of about five weeks from mid‐March to early April of 2020, screening mammograms covered by Independence came to a near halt—decreasing by 99% of the expected levels. Diagnostic mammograms—performed when breast cancer might be suspected—decreased at a slower rate, dropping by 74% of the expected levels. These unprecedented reductions in mammograms suggest that policies, regulations, and recommendations enacted to minimize unnecessary exposure to COVID‐19 in the medical setting were effective in reducing nonurgent care.
Our analyses rely on claims data, which allow us to track the weekly number of mammograms across numerous hospitals, outpatient clinics, and health systems. Nevertheless, there are important limitations as well. Our data are limited to commercially insured individuals and do not include mammograms performed for Medicare Part B beneficiaries or for uninsured women. It is possible that the trends in mammograms for these subpopulations would be different than for privately insured women, although we have little reason to expect that utilization patterns would have looked very different during the period since mid‐March of 2020. Using claims data, we are also unable to observe whether the mammogram yielded a positive or negative diagnosis for breast cancer, which limits our ability to address the question of net health impact resulting from mammograms that were conducted during this period.
When considering the overall impact of the substantial reductions in mammography we observe, one must weigh both the potential benefits and harms. On the one hand, reductions in screening mammography due to COVID‐19 likely will not significantly impact the many women who would have tested negative had they received a mammogram. For low‐risk women, less frequent screening may in fact yield similar outcomes. 15 Some 10% of women who may have received a false positive reading may even experience an increased quality of life. 16 For a subset of women, however, a missed or delayed mammogram may lead to a breast cancer diagnosis at a more advanced stage 17 or a larger tumor, 18 although the survival benefit of early diagnosis has not been definitively established. Previous studies suggest that the incidence of true‐positive mammograms may range from 0.51% 19 to 0.82%. 20 By extrapolation, our estimate of 39,200 missed screening mammograms translates to 200 to 320 women within the insurer's population that will experience a delayed breast cancer diagnosis, of which 130 to 200 will be a diagnosis of an invasive cancer. The rate of true‐positive diagnosis among the estimated 6,300 missing diagnostic mammograms can be assumed to be similar or higher, as diagnostic mammograms are only scheduled following an abnormal finding.
Our data also show that mammography volumes in our sample began to rebound starting in May. By the end of July, the volume of diagnostic mammograms reached levels similar to those observed in previous years, while the volume of screening mammograms remained somewhat below expected levels. This is consistent with our expectation that diagnostic mammograms would receive priority over routine screening mammograms, especially in light of limited capacity. Absent any prioritization and assuming all women with missed mammograms would seek to receive one after the resumption of nonurgent health care services, our estimates suggest that it would take 22 weeks to clear the queue in the best‐case scenario. In the worst‐case scenario, the queue would continue to grow, in which case providers would need to resort to prioritizing high‐risk patients and delaying low‐risk patients’ screenings for a year or more.
Our data only represent a fraction of women around the country and around the world affected by altered protocols for the provision of nonurgent health care services. Breast cancer is not the only form of cancer with reduced screening rates. Given the importance of early detection in the effective management of cancer, the full implications of these changes in screening patterns may not be realized for years to come. Health systems have wisely and effectively enacted policies that mitigate the spread of COVID‐19, but cancer will not wait for health systems to resume normalcy. Delaying mammograms today may lead to increased demand in the future; a combination of increased demand for screening and reduced screening availability due to spread mitigation efforts could challenge health care systems’ capacity for screening. As COVID‐19 establishes a new norm in routine medical care for the foreseeable future, policymakers, researchers and administrators should continuously reassess daily operations to optimize care for all patients—including those for which the true threat may take years to manifest.
CONFLICT OF INTEREST
None.
Supporting information
Supplementary Material
ACKNOWLEDGMENTS
Joint Acknowledgment/Disclosure Statement: A Bergman was partially supported by the National Institutes of Health under grant T32‐5T32HS26116. AM Bond reported receiving grants outside this work from Arnold Ventures, Physicians Foundation, and the American Medical Association. D Ellis, JM Bailey, R Brooks, and A Smith‐McLallen were employed by Independence Blue Cross during the course of the study. The views expressed in this paper are solely the authors' and do not reflect the views of the National Institutes of Health, Arnold Ventures, Physicians Foundation, the American Medical Association, or Independence Blue Cross.
Song H, Bergman A, Chen AT, et al. Disruptions in preventive care: Mammograms during the COVID‐19 pandemic. Health Serv Res.2021;56:95–101. 10.1111/1475-6773.13596
REFERENCES
- 1. American Medical Association . Factsheet: State Action Related to Delay and Resumption of “Elective” Procedures during COVID‐19 Pandemic. 2020. https://www.ama‐assn.org/system/files/2020‐05/state‐elective‐procedure‐chart.pdf. Accessed June 6, 2020
- 2. Centers for Disease Control and Prevention . Outpatient and Ambulatory Care Settings: Responding to Community Transmission of COVID‐19 in the United States. Centers for Disease Control and Prevention; Published February 11, 2020. https://www.cdc.gov/coronavirus/2019‐ncov/hcp/ambulatory‐care‐settings.html. Accessed June 6, 2020 [Google Scholar]
- 3. Centers for Medicare & Medicaid Services . Non‐Emergent, Elective Medical Services, and Treatment Recommendations. 2020. https://www.cms.gov/files/document/31820‐cms‐adult‐elective‐surgery‐and‐procedures‐recommendations.pdf
- 4. National Cancer Institute . Breast Cancer Screening. Published 2020. https://progressreport.cancer.gov/detection/breast_cancer
- 5. Bevers TB, Helvie M, Bonaccio E, et al. Breast cancer screening and diagnosis, version 3.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2018;16(11):1362‐1389. 10.6004/jnccn.2018.0083 [DOI] [PubMed] [Google Scholar]
- 6. Vlahiotis A, Griffin B, Stavros AT, Margolis J. Analysis of utilization patterns and associated costs of the breast imaging and diagnostic procedures after screening mammography. Clin Outcomes Res. 2018;10:157‐167. 10.2147/CEOR.S150260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lefeuvre D, Catajar N, Le Bihan BC, et al. Breast cancer screening: impact on care pathways. Cancer Med. 2019;8:4070‐4078. 10.1002/cam4.2283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cucinotta D, Vanelli M. WHO Declares COVID‐19 a pandemic. Acta Bio Medica Atenei Parm. 2020;91(1):157‐160. 10.23750/abm.v91i1.9397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. The White House . Proclamation on Declaring a National Emergency Concerning the Novel Coronavirus Disease (COVID‐19) Outbreak. The White House. Published March 13, 2020. https://www.whitehouse.gov/presidential‐actions/proclamation‐declaring‐national‐emergency‐concerning‐novel‐coronavirus‐disease‐covid‐19‐outbreak/. Accessed June 6, 2020
- 10. Centers for Disease Control and Prevention . Coronavirus disease 2019 (COVID‐19) in the U.S. Centers for Disease Control and Prevention. Published June 5, 2020. https://www.cdc.gov/coronavirus/2019‐ncov/cases‐updates/cases‐in‐us.html. Accessed June 6, 2020
- 11. Pennsylvania Department of Health . PA Coronavirus (COVID‐19) Update Archive March 2020. Published March 31, 2020. https://www.health.pa.gov:443/topics/disease/coronavirus/Pages/March‐Archive.aspx. Accessed September 3, 2020
- 12. Pennsylvania Department of Health . All non‐life‐sustaining businesses in Pennsylvania to close physical locations as of 8 pm today to slow spread of Covid‐19. Published March 19, 2020. https://www.governor.pa.gov/newsroom/all‐non‐life‐sustaining‐businesses‐in‐pennsylvania‐to‐close‐physical‐locations‐as‐of‐8‐pm‐today‐to‐slow‐spread‐of‐covid‐19/. Accessed September 3, 2020
- 13. Pennsylvania Department of Health . Guidance on COVID‐19 for health care providers. Published online May 9, 2020. https://www.health.pa.gov/topics/Documents/Diseases%20and%20Conditions/Guidance%20on%20COVID‐19%20for%20Health%20Care%20Providers.pdf. Accessed June 6, 2020
- 14. Moy L, Toth HK, Newell MS, Plecha D, Leung JWT, Harvey JA. Response to COVID‐19 in breast imaging. J Breast Imaging. 2020;2(3):180‐185. 10.1093/jbi/wbaa025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Trentham‐Dietz A, Kerlikowske K, Stout NK, et al. Tailoring breast cancer screening intervals by breast density and risk for women aged 50 years or older: collaborative modeling of screening outcomes. Ann Intern Med. 2016;165(10):700‐712. 10.7326/M16-0476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Seely JM, Alhassan T. Screening for breast cancer in 2018—what should we be doing today? Curr Oncol. 2018;25(S1):S115‐S124. 10.3747/co.25.3770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Unger‐Saldaña K, Miranda A, Zarco‐Espinosa G, Mainero‐Ratchelous F, Bargalló‐Rocha E, Miguel L‐L. Health system delay and its effect on clinical stage of breast cancer: multicenter study. Cancer. 2015;121(13):2198‐2206. 10.1002/cncr.29331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tartter PI, Pace D, Frost M, Bernstein JL. Delay in diagnosis of breast cancer. Ann Surg. 1999;229(1):91‐96. 10.1097/00000658-199901000-00012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lehman CD, Arao RF, Sprague BL, et al. National performance benchmarks for modern screening digital mammography: update from the breast cancer surveillance consortium. Radiology. 2017;283(1):49‐58. 10.1148/radiol.2016161174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fenton JJ, Xing G, Elmore JG, et al. Short‐term outcomes of screening mammography using computer‐aided detection: a population‐based study of Medicare enrollees. Ann Intern Med. 2013;158(8):580‐587. 10.7326/0003-4819-158-8-201304160-00002 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


