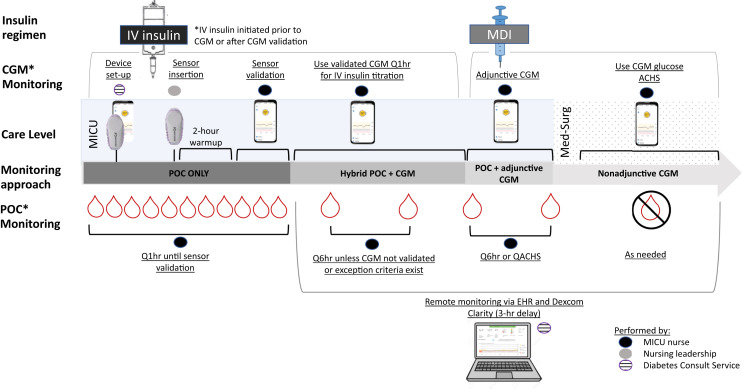
Fig. 1.
Hybrid CGM + POC glucose monitoring. Hybrid CGM +POC glucose monitoring occurred in several phases. Diabetes consult service members performed device set-up tasks prior to delivering the devices to the ICU units. The nursing leadership team worked with MICU providers to identify appropriate patients with anticipated or current IV insulin orders. The nursing leadership team performed sensor insertion and paired the transmitter with the cell phone/receiver. Once paired, a 2-hour warm-up period was initiated, followed by a sensor validation period. The IV insulin infusion was titrated every hour using the POC BG value until initial validation was achieved. Then titration was performed using the CGM unless Q6 hour sensor-meter pairs were discordant or other exception criteria occurred. Additional sensors could be placed if the patient had ongoing IV insulin requirements following initial sensor expiration or removal. When patients were transitioned off IV insulin, Q6 hour POC testing was continued along with adjunctive CGM while in the MICU or until sensor expiration. Once transferred to a medical surgical floor, CGM could be used nonadjunctively (to replace POC testing) according to the institution’s global Hyperglycemia in COVID-19 Patients guideline. The Diabetes consult service utilized Dexcom Clarity, which operates on a 3-hour delay, to retrospectively visualize patient data and analyze glucose trends. BG = blood glucose; CGM = continuous glucose monitoring; COVID-19 = coronavirus disease 2019; EHR = electronic health record; ICU = intensive care unit; IV = intravenous; MDI = multiple daily injection; MICU = medical intensive care unit; POC = point of care (arterial, capillary).