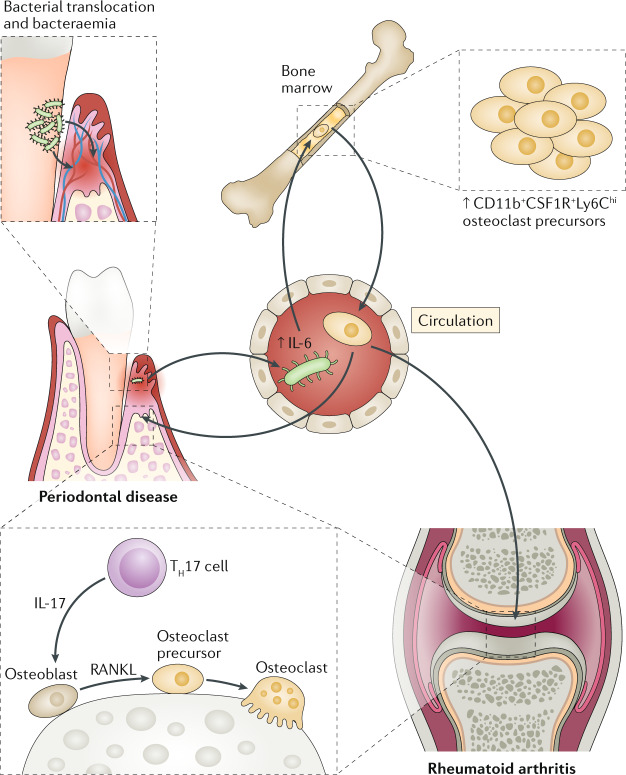
Fig. 2. Periodontal bacterial translocation leading to bacteraemia and alterations in the bone marrow that promote osteoclastogenesis in different sites.
Periodontal bacteria may translocate through the ulcerated epithelium of the periodontal pockets into the circulation, causing bacteraemia and systemic inflammation. Blood-borne Porphyromonas gingivalis causes an increase in the serum levels of IL-6, which in turn induces the expansion of an osteoclast precursor population (defined as CD11b+CSF1R+Ly6Chi) in the bone marrow. This osteoclast precursor population displays enhanced osteoclastogenic lineage bias and populates various bone resorption sites, where it can differentiate into mature osteoclasts, in response to locally produced receptor activator of NF-κB ligand (RANKL) (for example, produced by osteoblasts stimulated by T helper 17 (TH17) cell-derived IL-17). This concept may be a mechanism whereby the bone marrow might link periodontitis to other bone loss disorders, such as rheumatoid arthritis.